Chapter 17
Pharmacokinetic Alterations in the Critically Ill
Effects of Altered Physiology on Pharmacokinetics
Renal Dysfunction
Although low-molecular-weight drugs (that are not highly protein bound) are filtered at the glomerulus and then partially reabsorbed, most drugs eliminated by the kidney are secreted. The dose or interval of drugs eliminated renally by either mechanism must be changed when renal function is impaired. Renal clearance of medications decreases in proportion to decreases in creatinine clearance (CrCl).
Dialysis
Whether a drug is affected by hemodialysis depends on the drug’s physicochemical properties and the method of hemodialysis. In general, highly water-soluble drugs are more dialyzable than are water-insoluble drugs. Drugs with large molecular weights, large volumes of distribution (>2 L/kg), and extensive protein binding are not removed by conventional intermittent hemodialysis with low flux filters; however, high-flux dialysis may remove larger molecules. Currently, the majority of patients receive hemodialysis with high-flux filters. In addition to the physiochemical properties of a medication, the amount of drug removed by hemodialysis depends on the length of the hemodialysis session, the rate of blood flow, and dialysate. Patients receiving ultrafiltration will have lower percentages of drug removal than those receiving hemodialysis. If a medication is significantly removed by hemodialysis, patients may require a supplemental dose following the dialysis session. Continuous renal replacement therapy uses membranes that are similar to high-flux filters and approximates a CrCl of 30 to 60 mL/min depending on rate of blood flow and dialysate (Chapter 20). Medications in these patients should be adjusted accordingly.
Obesity
A relatively new challenge in health care is the management of patients who are overweight, obese, or morbidly obese (Chapter 29). Although this represents a growing proportion of patients, information regarding the pharmacokinetic changes in these patients is scarce. Information about the oral absorption of medications in obese patients is lacking, and it is unclear what changes occur in this population, if any. Patients undergoing gastric bypass represent an understudied population in regard to oral absorption of medications. No conclusion regarding altered absorption in this population can be made. Obese patients commonly have increases in cardiac output, total blood volume, and organ mass. These changes theoretically contribute to an increased volume of distribution; however, the clinical significance of this is unknown. Serum albumin and total protein are not altered in obese patients, thus distribution of medications that are significantly bound to plasma proteins should not change. Medications that are highly lipophilic may have higher volumes of distribution; however, not all lipophilic drugs distribute to adipose tissue. The decision of dosing a medication on a predicted or lean (also referred to as “ideal”), total, or adjusted body weight should be based on published clinical data. In general, the metabolism of drugs that undergo phase II conjugation may be increased, whereas the metabolism of drugs that undergo phase I metabolism can vary based on the specific cytochrome P450 enzyme involved.
Transdermal Drug Delivery
The drawbacks of the administration of medications via the transdermal route should be carefully considered in the critically ill population. Decreased perfusion to subcutaneous and epidermal tissue may make absorption erratic and unreliable for drug administration. Furthermore, certain medications such as fentanyl have increased absorption in febrile states, which may lead to adverse events from unpredictable drug administration. Certain other drugs (nicotine, clonidine, Androderm, or scopolamine) have patches with aluminum in their backing such that they may not be worn in a magnetic resonance imaging (MRI) machine or during cardioversion. Rapid escalation or de-escalation of dose is typically not possible because of the longer onset and offset of transdermal medications. Overall, caution should be used when choosing transdermal medications, and other more reliable routes of medication administration should be chosen when possible.
Aminoglycosides
Aminoglycosides, specifically gentamicin, are also used for synergistic effects against gram-positive organisms (Staphylococcus spp., Enterococcus spp., and Streptococcus spp.). The dosing strategy and goal peak concentrations for synergy differ from those associated with managing infections due to gram-negative bacteria. Table 17.1 contains dosing strategies and goal serum concentrations for traditional, once-daily, or extended interval and synergy dosing. Peak and trough concentrations are typically recommended for patients receiving traditional or synergy dosing. Peaks should be obtained at steady state, 1 hour after completing the infusion of the fourth or fifth dose. Troughs should be obtained at steady state prior to the fourth or fifth dose. A random level 6 to 14 hours after the first dose should be obtained in patients receiving once-daily or extended interval dosing. This level should be applied to various nomograms that aid in dosing. Figure 17.1 is the most commonly used nomogram, the Hartford nomogram. Patients on the borderline of a dosage interval should be dosed using the greater dosage interval. In patients receiving amikacin, the random level should be divided by 2 before applying the nomogram.
TABLE 17.1
Dosing Strategies and Desired Therapeutic Concentrations for Aminoglycosides
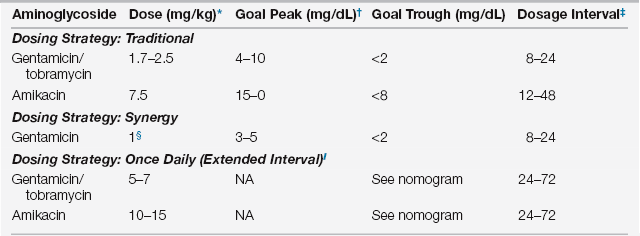
∗If actual body weight (ABW) > 120% of predicted body weight (PBW), use adjusted body weight (AdjW) where AdjBW = (ABW − PBW) ∗ 0.4 + PBW. Note: PBW (kg) for men = 50 + 2.3 × number of inches above 60 inches in height; PBW (kg) for women = 45.5 + 2.3 × number of inches above 60 inches in height.
†Goal peak will depend on severity and location of infection.
‡Dosage interval (hours) should be adjusted based on renal function.
§This can be given as 3 mg/kg once daily in patients with streptococcal endocarditis.
 In order to apply the Hartford nomogram, doses of 7 mg/kg for gentamicin/tobramycin and 15 mg/kg for amikacin must be used. (See the bibliography for other nomograms for lower doses that are not included here.)
In order to apply the Hartford nomogram, doses of 7 mg/kg for gentamicin/tobramycin and 15 mg/kg for amikacin must be used. (See the bibliography for other nomograms for lower doses that are not included here.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







