TOPICS
2. Mechanisms of Peripheral Nerve Injury
3. Risk Factors for Peripheral Nerve Injury
5. Types of Peripheral Nerve Injury
The majority of complications involving peripheral nerves are unrelated to the anesthetic technique and more likely due to obstetric circumstances. A survey of 6057 women who delivered in Chicago1 reported an incidence of lower extremity nerve injuries of approximately 1% (24 lateral femoral cutaneous nerve, 22 femoral nerve, 3 peroneal nerve, 3 lumbosacral plexus, 2 sciatic nerve, 3 obturator nerve, and 5 radicular injuries).1 Significant risk factors for peripheral nerve injury (PNI) were nulliparity and a prolonged second stage of labor, but not neuraxial anesthesia. The findings of this survey corroborate those of the Leeds study,2 stating that “that postpartum neurologic dysfunction is more frequent if specifically sought, and support the clinical impression that significant neurological deficits occur irrespective of the use of regional anaesthesia.”
EPIDEMIOLOGY
The detection of PNI may be spuriously increasing as a result of the routine follow-up performed by the anesthesia team in the immediate postpartum period to detect complications linked to the practice of neuraxial anesthesia (eg, postdural puncture headache, epidural hematoma, nerve root damage). On the other hand, with the changes in obstetric practices regarding intolerance for protracted labor and difficult forceps delivery, the prevalence of these complications will likely decrease. The new obstetric guidelines show a preference for cesarean delivery as opposed to prolonged labor and forceps assistance in these situations.
Neurologic complaints due to factors associated with labor and delivery are seen in 1.6 to 4.8/10,000 of parturients, and those attributed to the possible deficits related to regional anesthetic techniques are found in 0 to 1.2/10,000 of parturients.3
MECHANISMS OF PERIPHERAL NERVE INJURY
Acute nerve injury may occur as a consequence of transection, traction, compression of a nerve, or vascular injury.4
• Compression or traction on a nerve can result in compromised perineural blood flow and lead to ischemia. This may cause focal demyelination and conduction block. However, symptoms are usually transient, because the focal demyelization is a reversible phenomenon.
• In more serious injuries, the axons of the nerve can be damaged. In this case, the damage can be permanent, or if temporary, the symptoms will disappear slowly.
• Neuraxial anesthesia can mask the early symptoms of PNI. Residual numbness or weakness can be attributed falsely to residual local anesthetic effect. Thus, a high index of suspicion for PNI must be maintained in the face of unintended extended sensory or motor block.
RISK FACTORS FOR PERIPHERAL NERVE INJURY
Risk factors may be maternal or fetal.5,6
• Maternal obesity
• Abnormal presentation
• Persistent occiput posterior position
• Fetal macrosomia/fetus large for gestational age
Risk factors may be related to the labor.5,6
• Breakthrough pain during epidural labor analgesia
• Prolonged second stage of labor
• Difficult instrumental delivery
• Prolonged use of the lithotomy position
SYMPTOMS
PNIs typically result in a neurologic deficit in the distribution of a specific peripheral nerve. Neurologic or neurosurgical consultation and immediate imaging studies should be obtained if there is any question about the etiology of prolonged anesthesia; it is necessary to rule out an epidural/spinal hematoma because PNI can be confused with epidural hematoma. However, symptoms that are suggestive of PNI versus epidural hematoma include absence of back pain with PNI, unilateral block, and regression (rather than progression) of the symptoms. When the roots are touched at the level of the spinal cord, secondary to neuraxial anesthesia, the distribution of the symptoms will be more extended. As for PNI, depending on the nerve damaged, the symptoms and circumstances of the injury will be different (Figure 16-1).7,8
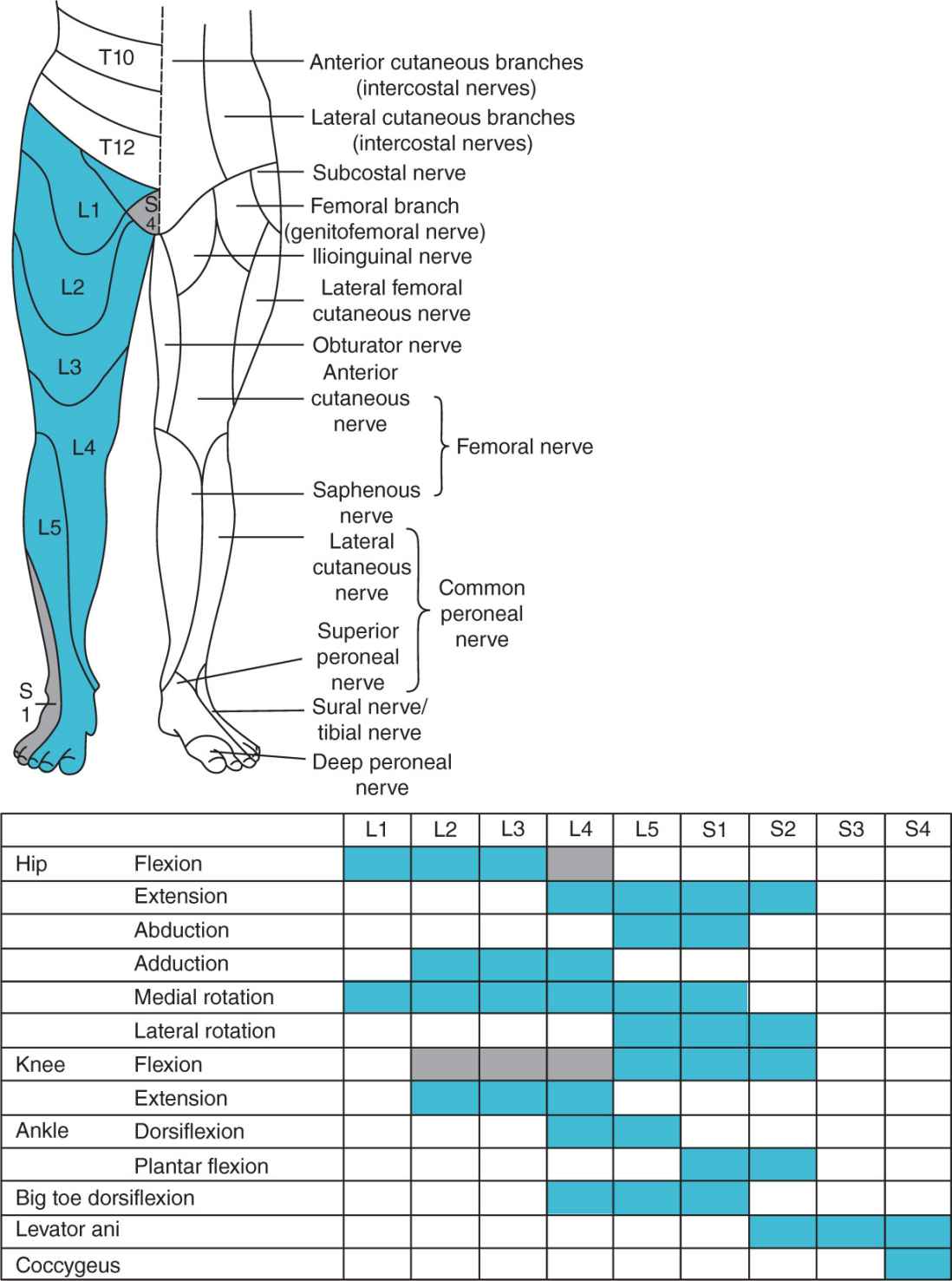
Figure 16-1. Sensory innervation of the lower extremity. Precise identification of the location of the deficit will aid in assessing improvement and suggest possible etiologies for the deficit.
TYPES OF PERIPHERAL NERVE INJURY
Lumbosacral Trunk: L4 and L5 Roots
ANATOMY
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








