Key Concepts
 In addition to potent analgesia, regional anesthesia may lead to reductions in the stress response, systemic analgesic requirements, opioid-related side effects, general anesthesia requirements, and possibly the incidence of chronic pain.
In addition to potent analgesia, regional anesthesia may lead to reductions in the stress response, systemic analgesic requirements, opioid-related side effects, general anesthesia requirements, and possibly the incidence of chronic pain.
 Regional anesthetics should be administered in an area where standard hemodynamic monitors, supplemental oxygen, and resuscitative medications and equipment are readily available.
Regional anesthetics should be administered in an area where standard hemodynamic monitors, supplemental oxygen, and resuscitative medications and equipment are readily available.
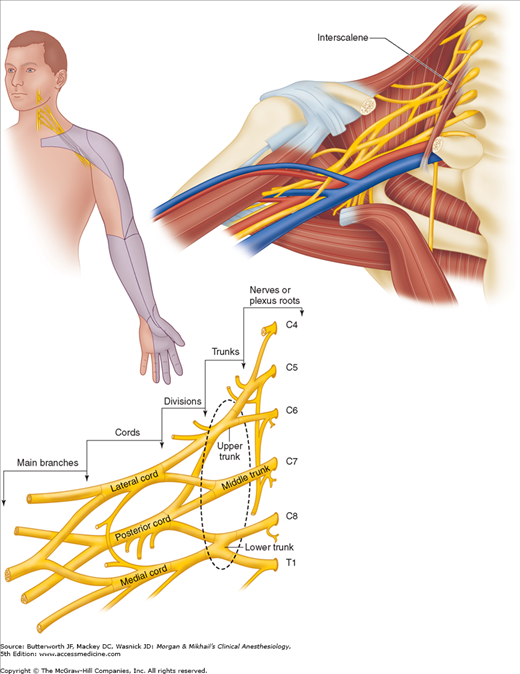
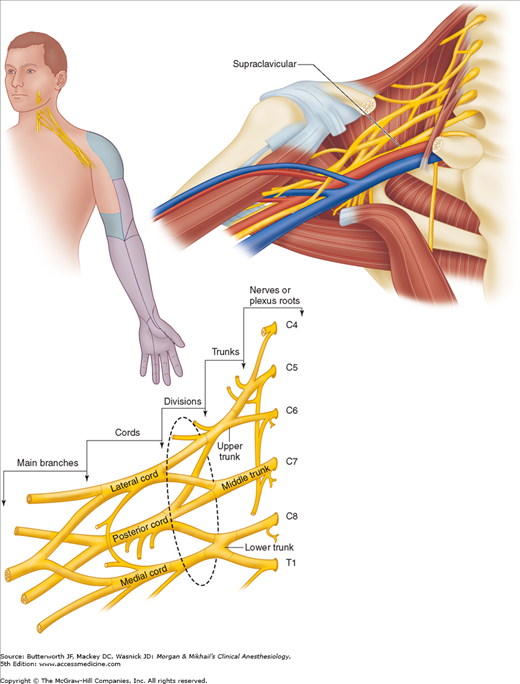
 Local anesthetic may be deposited at any point along the brachial plexus, depending on the desired block effects: interscalene for shoulder and proximal humerus surgical procedures; and supraclavicular, infraclavicular, and axillary for surgeries distal to the mid-humerus.
Local anesthetic may be deposited at any point along the brachial plexus, depending on the desired block effects: interscalene for shoulder and proximal humerus surgical procedures; and supraclavicular, infraclavicular, and axillary for surgeries distal to the mid-humerus.
 A properly performed interscalene block invariably blocks the ipsilateral phrenic nerve, so careful consideration should be given to patients with severe pulmonary disease or preexisting contralateral phrenic nerve palsy.
A properly performed interscalene block invariably blocks the ipsilateral phrenic nerve, so careful consideration should be given to patients with severe pulmonary disease or preexisting contralateral phrenic nerve palsy.
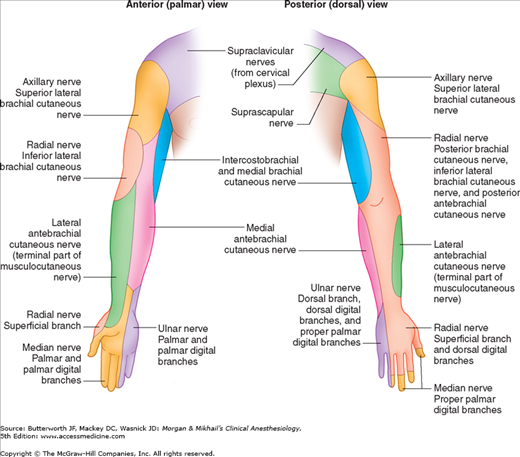
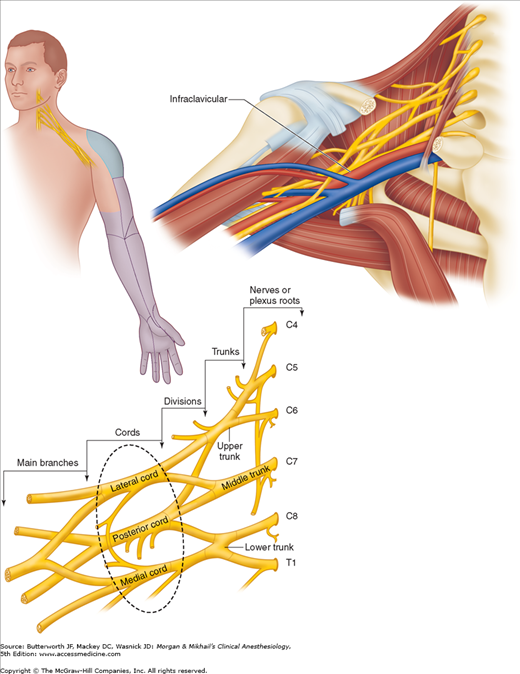
 Brachial plexus block at the level of the cords provides excellent anesthesia for procedures at or distal to the elbow. The upper arm and shoulder are not anesthetized with this approach. As with other brachial plexus blocks, the intercostobrachial nerve (T2 dermatome) is spared.
Brachial plexus block at the level of the cords provides excellent anesthesia for procedures at or distal to the elbow. The upper arm and shoulder are not anesthetized with this approach. As with other brachial plexus blocks, the intercostobrachial nerve (T2 dermatome) is spared.
 The axillary, musculocutaneous, and medial brachial cutaneous nerves branch from the brachial plexus proximal to the location in which local anesthetic is deposited during an axillary nerve block, and thus are usually spared.
The axillary, musculocutaneous, and medial brachial cutaneous nerves branch from the brachial plexus proximal to the location in which local anesthetic is deposited during an axillary nerve block, and thus are usually spared.
 Often it is necessary to anesthetize a single terminal nerve, either for minor surgical procedures with a limited field or as a supplement to an incomplete brachial plexus block. Terminal nerves may be anesthetized anywhere along their course, but the elbow and the wrist are the two most favored sites.
Often it is necessary to anesthetize a single terminal nerve, either for minor surgical procedures with a limited field or as a supplement to an incomplete brachial plexus block. Terminal nerves may be anesthetized anywhere along their course, but the elbow and the wrist are the two most favored sites.
 Intravenous regional anesthesia, also called a Bier block, can provide intense surgical anesthesia for short surgical procedures (45-60 min) on an extremity.
Intravenous regional anesthesia, also called a Bier block, can provide intense surgical anesthesia for short surgical procedures (45-60 min) on an extremity.
 A femoral nerve block alone will seldom provide surgical anesthesia, but it is often used to provide postoperative analgesia for hip, thigh, knee, and ankle procedures.
A femoral nerve block alone will seldom provide surgical anesthesia, but it is often used to provide postoperative analgesia for hip, thigh, knee, and ankle procedures.
 Posterior lumbar plexus blocks are useful for surgical procedures involving areas innervated by the femoral, lateral femoral cutaneous, and obturator nerves. Complete anesthesia of the knee can be attained with a proximal sciatic nerve block.
Posterior lumbar plexus blocks are useful for surgical procedures involving areas innervated by the femoral, lateral femoral cutaneous, and obturator nerves. Complete anesthesia of the knee can be attained with a proximal sciatic nerve block.
 Blockade of the sciatic nerve may occur anywhere along its course and is indicated for surgical procedures involving the hip, thigh, knee, lower leg, and foot.
Blockade of the sciatic nerve may occur anywhere along its course and is indicated for surgical procedures involving the hip, thigh, knee, lower leg, and foot.
 Popliteal nerve blocks provide excellent coverage for foot and ankle surgery, while sparing much of the hamstring muscles, allowing lifting of the foot with knee flexion, thus easing ambulation. All sciatic nerve blocks fail to provide complete anesthesia for the cutaneous medial leg and ankle joint capsule, but when a saphenous (or femoral) block is added, complete anesthesia below the knee is provided.
Popliteal nerve blocks provide excellent coverage for foot and ankle surgery, while sparing much of the hamstring muscles, allowing lifting of the foot with knee flexion, thus easing ambulation. All sciatic nerve blocks fail to provide complete anesthesia for the cutaneous medial leg and ankle joint capsule, but when a saphenous (or femoral) block is added, complete anesthesia below the knee is provided.
 A complete ankle block requires a series of five nerve blocks, but the process may be streamlined to minimize needle insertions. All five injections are required to anesthetize the entire foot; however, many surgical procedures involve only a few terminal nerves, and only affected nerves should be blocked.
A complete ankle block requires a series of five nerve blocks, but the process may be streamlined to minimize needle insertions. All five injections are required to anesthetize the entire foot; however, many surgical procedures involve only a few terminal nerves, and only affected nerves should be blocked.
 Intercostal blocks result in the highest blood levels of local anesthetic per volume injected of any block in the body, and care must be taken to avoid toxic levels of local anesthetic.
Intercostal blocks result in the highest blood levels of local anesthetic per volume injected of any block in the body, and care must be taken to avoid toxic levels of local anesthetic.
 The thoracic paravertebral space is defined posteriorly by the superior costotransverse ligament, anterolaterally by the parietal pleura, medially by the vertebrae and the intervertebral foramina, and inferiorly and superiorly by the heads of the ribs.
The thoracic paravertebral space is defined posteriorly by the superior costotransverse ligament, anterolaterally by the parietal pleura, medially by the vertebrae and the intervertebral foramina, and inferiorly and superiorly by the heads of the ribs.
 The subcostal (T12), ilioinguinal (L1), and iliohypogastric (L1) nerves are targeted in the transversus abdominus plane block, providing anesthesia to the ipsilateral lower abdomen below the umbilicus.
The subcostal (T12), ilioinguinal (L1), and iliohypogastric (L1) nerves are targeted in the transversus abdominus plane block, providing anesthesia to the ipsilateral lower abdomen below the umbilicus.
Peripheral Nerve Blocks: Introduction
An understanding of regional anesthesia anatomy and techniques is required of the well-rounded anesthesiologist. Although anatomic relationships have not changed over time, our ability to identify them has evolved. From the paresthesia-seeking techniques described by Winnie in the mid-twentieth century, to the popularization of the nerve stimulator, to the introduction of ultrasound guidance, anesthesiologists and their patients have benefitted from technology’s evolution. The field of regional anesthesia has accordingly expanded to one that addresses not only the intraoperative concerns of the anesthesiologist, but also longer term perioperative pain management.  In addition to potent analgesia, regional anesthesia may lead to reductions in the stress response, systemic analgesic requirements, opioid-related side effects, general anesthesia requirements, and possibly the development of chronic pain.
In addition to potent analgesia, regional anesthesia may lead to reductions in the stress response, systemic analgesic requirements, opioid-related side effects, general anesthesia requirements, and possibly the development of chronic pain.
Patient Selection
The selection of a regional anesthetic technique is a process that begins with a thorough history and physical examination. Although many patients are candidates for regional anesthesia/analgesia, as with any medical procedure a risk-benefit analysis must be performed. The risk-benefit ratio often favors regional anesthesia in patients with multiple comorbidities for whom a general anesthetic carries a greater risk. In addition, patients intolerant to systemic analgesics (eg, those with obstructive sleep apnea or at high risk for nausea) may benefit from the opioid-sparing effects of a regional analgesic. Patients with chronic pain and opioid tolerance may receive optimal analgesia with a continuous peripheral nerve block (so-called perineural local anesthetic infusion).
A comprehensive knowledge of anatomy and an understanding of the planned surgical procedure are important for selection of the appropriate regional anesthetic technique. If possible, discussion with the surgeon about various considerations (tourniquet placement, bone grafting, projected surgical duration) is ideal. Also, knowing the anticipated course of recovery and anticipated level of postoperative pain will often influence specific decisions regarding a regional anesthetic technique (eg, a single-injection versus continuous peripheral nerve block).
Risks & Contraindications
Patient cooperation and participation are key to the success and safety of every regional anesthetic procedure; patients who are unable to remain still for a procedure may be exposed to increased risk. Examples include younger pediatric patients and some developmentally delayed individuals, as well as patients with dementia or movement disorders. Bleeding disorders and pharmacological anticoagulation heighten the risk of local hematoma or hemorrhage, and this risk must be balanced against the possible benefits of regional block. Specific peripheral nerve block locations warranting the most concern are posterior lumbar plexus and paravertebral blocks owing to their relative proximity to the retroperitoneal space and neuraxis, respectively.
Placement of a block needle through a site of infection can theoretically track infectious material into the body, where it poses a risk to the target nerve tissue and surrounding structures. Therefore, the presence of a local infection is a relative contraindication to performing a peripheral nerve block. Indwelling perineural catheters can serve as a nidus of infection; however, the risk in patients with systemic infection remains unknown.
Although nerve injury is always a possibility with a regional anesthetic, some patients are at increased risk. Individuals with a preexisting condition (eg, peripheral neuropathy or previous nerve injury) may have a higher incidence of complications, including prolonged or permanent sensorimotor block. The precise mechanisms have yet to be clearly defined but may involve local ischemia from high injection pressure or vasoconstrictors, a neurotoxic effect of local anesthetics, or direct trauma to nerve tissue.
Other risks associated with regional anesthesia include local anesthetic toxicity from intravascular injection or perivascular absorption. In the event of a local anesthetic toxic reaction, seizure activity and cardiovascular collapse may occur. Supportive measures should begin immediately, including solicitation of assistance with a code blue, the initiation of cardiopulmonary resuscitation, lipid emulsion administration to sequester local anesthetic, and preparation for cardiopulmonary bypass.
Choice of Local Anesthetic
The decision about which local anesthetic to employ for a particular nerve block depends on the desired onset, duration, and relative blockade of sensory and motor fibers. Potential for toxicity should be considered, as well as site-specific risks. A detailed discussion of local anesthetics is provided elsewhere (see Chapter 16).
Preparation
 Regional anesthetics should be administered in an area where standard hemodynamic monitors, supplemental oxygen, and resuscitative medications and equipment are readily available. Patients should be monitored with pulse oximetry, noninvasive blood pressure, and electrocardiography; measurement of end-tidal CO2 and fraction of inspired oxygen (Fio2) should also be available. Positioning should be ergonomically favorable for the practitioner and comfortable for the patient. Intravenous premedication should be employed to allay anxiety and minimize discomfort. A relatively short-acting benzodiazepine and opioid are most often used and should be titrated for comfort while ensuring that patients respond to verbal cues. Sterile technique should be strictly observed.
Regional anesthetics should be administered in an area where standard hemodynamic monitors, supplemental oxygen, and resuscitative medications and equipment are readily available. Patients should be monitored with pulse oximetry, noninvasive blood pressure, and electrocardiography; measurement of end-tidal CO2 and fraction of inspired oxygen (Fio2) should also be available. Positioning should be ergonomically favorable for the practitioner and comfortable for the patient. Intravenous premedication should be employed to allay anxiety and minimize discomfort. A relatively short-acting benzodiazepine and opioid are most often used and should be titrated for comfort while ensuring that patients respond to verbal cues. Sterile technique should be strictly observed.
Block Techniques
A field block is a local anesthetic injection that targets terminal cutaneous nerves (Figure 46-1). Field blocks are used commonly by surgeons to minimize incisional pain and may be used as a supplementary technique or as a sole anesthetic for minor, superficial procedures. Anesthesiologists often use field blocks to anesthetize the superficial cervical plexus for procedures involving the neck or shoulder; the intercostobrachial nerve for surgery involving the medial upper extremity proximal to the elbow (in combination with a brachial plexus nerve block); and the saphenous nerve for surgery involving the medial leg or ankle joint (in combination with a sciatic nerve block). Field blocks may be undesirable in cases where they obscure the operative anatomy, or where local tissue acidosis from infection prevents effective local anesthetic functioning.
Formerly the mainstay of regional anesthesia, this technique is now rarely used for nerve localization. Using known anatomic relationships and surface landmarks as a guide, a block needle is placed in proximity to the target nerve or plexus. When a needle makes direct contact with a sensory nerve, a paresthesia (abnormal sensation) is elicited in its area of sensory distribution.
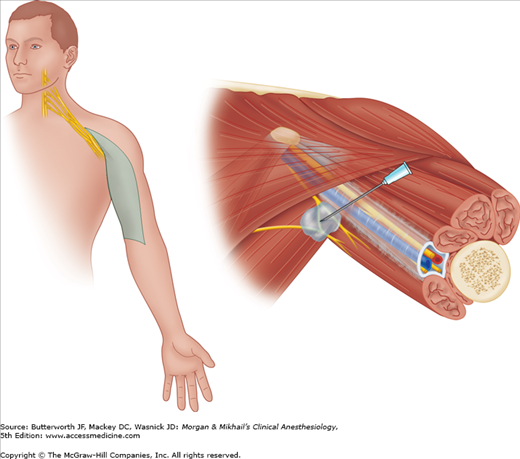
For this technique, an insulated needle concentrates electrical current at the needle tip, while a wire attached to the needle hub connects to a nerve stimulator—a battery-powered machine that emits a small amount (0-5 mA) of electric current at a set interval (usually 1 or 2 Hz). A grounding electrode is attached to the patient to complete the circuit (Figure 46-2). When the insulated needle is placed in proximity to a motor nerve, muscle contractions are induced, and local anesthetic is injected. Although it is common to redirect the block needle until muscle contractions occur at a current less than 0.5 mA, there is scant evidence to support this specific current in all cases. Similarly, although some have suggested that muscle contraction with current less than 0.2 mA implies intraneural needle placement, there is little evidence to support this specific cutoff. Nonetheless, most practitioners inject local anesthetic when current between 0.2 and 0.5 mA results in a muscle response. For most blocks using this technique, 30-40 mL of anesthetic is usually injected with gentle aspiration between divided doses.
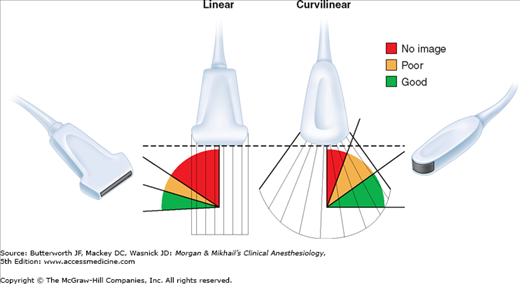
Ultrasound for peripheral nerve localization is becoming increasingly popular; it may be used alone or combined with other modalities such as nerve stimulation. Ultrasound uses high-frequency (1-20 MHz) sound waves emitted from piezoelectric crystals that travel at different rates through tissues of different densities, returning a signal to the transducer. Depending on the amplitude of signal received, the crystals deform to create an electronic voltage that is converted into a two-dimensional grayscale image. The degree of efficiency with which sound passes through a substance determines its echogenicity. Structures and substances through which sound passes easily are described as hypoechoic and appear dark or black on the ultrasound screen. In contrast, structures reflecting more sound waves appear brighter—or white—on the ultrasound screen, and are termed hyperechoic.
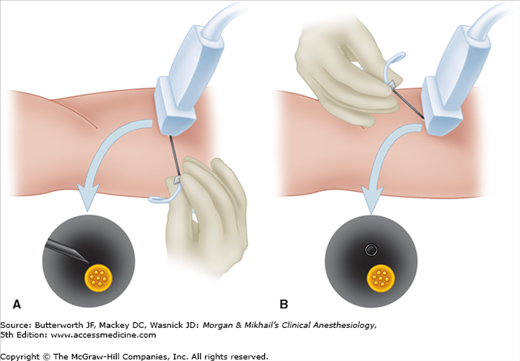
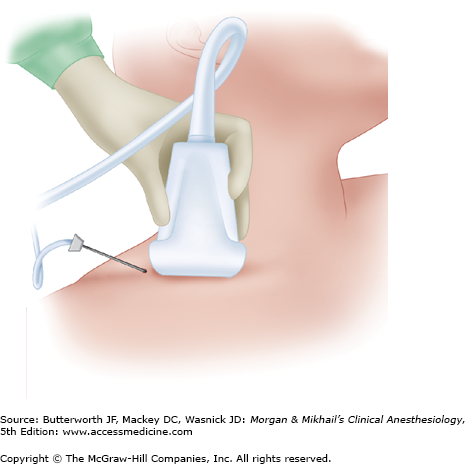
The optimal transducer varies depending upon the depth of the target nerve and approach angle of the needle relative to the transducer (Figure 46-3). High-frequency transducers provide a high-resolution picture with a relatively clear image but offer poor tissue penetration and are therefore used predominantly for more superficial nerves. Low-frequency transducers provide an image of poorer quality but have better tissue penetration and are therefore used for deeper structures. Transducers with a linear array offer an undistorted image and are therefore often the first choice among practitioners. However, for deeper target nerves that require a more acute angle between the needle and long-axis of the transducer, a curved array (curvilinear) transducer will maximize returning ultrasound waves, providing the optimal needle image (Figure 46-3). Nerves are best imaged in cross-section, where they have a characteristic honeycomb appearance (“short axis”). Needle insertion can pass either parallel (“in plane”) or not parallel (“out of plane”) to the plane of the ultrasound waves (Figure 46-4). Unlike nerve stimulation alone, ultrasound guidance allows for a variable volume of local anesthetic to be injected, with the final amount determined by what is observed under direct vision. This technique usually results in a far lower injected volume of local anesthetic (10-30 mL).
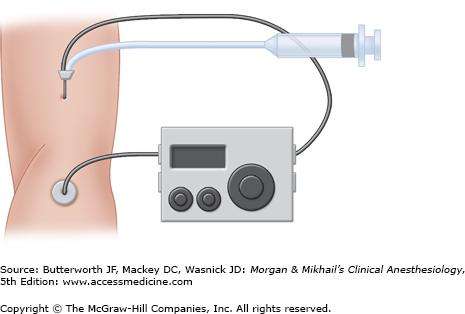
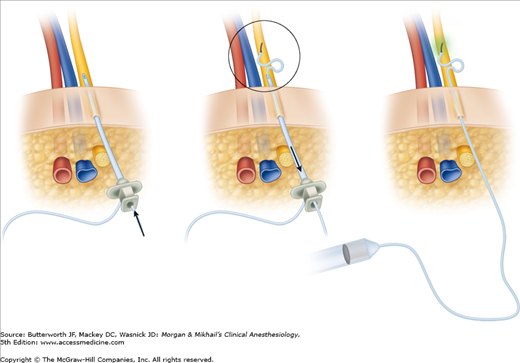
Also termed perineural local anesthetic infusion, continuous peripheral nerve blocks involve the placement of a percutaneous catheter adjacent to a peripheral nerve, followed by local anesthetic administration to prolong a nerve block (Figure 46-5). Potential advantages appear to depend on successfully improving analgesia and include reductions in resting and dynamic pain, supplemental analgesic requirements, opioid-related side effects, and sleep disturbances. In some cases patient satisfaction, ambulation, and functioning may be improved; an accelerated resumption of passive joint range-of-motion realized; and reduced time until discharge-readiness as well as actual discharge from the hospital or rehabilitation center achieved.
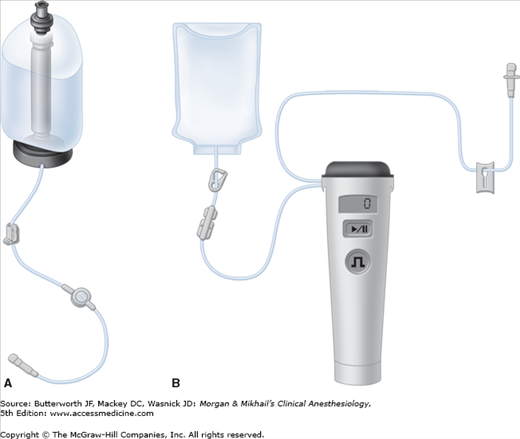
There are many types of catheters, including nonstimulating and stimulating, flexible and more rigid, through-the-needle and over-the-needle. Currently, there is little evidence that a single design results in superior effects. Local anesthetic is the primary medication infused, as adjuvants do not add benefits to perineural infusions (unlike single-injection peripheral nerve blocks). Long-acting local anesthetics (eg, ropivacaine) are more commonly used as they provide a more favorable sensory-to-motor block ratio (optimizing analgesia while minimizing motor block). In an attempt to further minimize any induced motor block, dilute local anesthetic (0.1-0.2%) is often infused; however, recent evidence suggests that it is the total dose, and not concentration, that determines the majority of block effects. Unlike single-injection peripheral nerve blocks, no adjuvant added to a perineural local anesthetic infusion has been demonstrated to be of benefit. The local anesthetic may be administered exclusively as repeated bolus doses or a basal infusion, or as a combination of the two methods. Using a small, portable infusion pump (Figure 46-6), continuous peripheral nerve blocks may be provided on an ambulatory basis.
As with all medical procedures, there are potential risks associated with continuous peripheral nerve blocks. Therefore, these infusions are usually reserved for patients having procedures expected to result in postoperative pain that is difficult to control with oral analgesics and will not resolve in less time than the duration of a single-injection peripheral nerve block. Serious complications, which are relatively rare, include systemic local anesthetic toxicity, catheter retention, nerve injury, infection, and retroperitoneal hematoma formation. In addition, a perineural infusion affecting the femoral nerve increases the risk of falling, although to what degree and by what specific mechanism (eg, sensory, motor, or proprioception deficits) remain unknown.
Upper Extremity Peripheral Nerve Blocks
The brachial plexus is formed by the union of the anterior primary divisions (ventral rami) of the fifth through the eighth cervical nerves and the first thoracic nerves. Contributions from C4 and T2 are often minor or absent. As the nerve roots leave the intervertebral foramina, they converge, forming trunks, divisions, cords, branches, and then finally terminal nerves. The three distinct trunks formed between the anterior and middle scalene muscles are termed superior, middle, and inferior based on their vertical orientation. As the trunks pass over the lateral border of the first rib and under the clavicle, each trunk divides into anterior and posterior divisions. As the brachial plexus emerges below the clavicle, the fibers combine again to form three cords that are named according to their relationship to the axillary artery: lateral, medial, and posterior. At the lateral border of the pectoralis minor muscle, each cord gives off a large branch before ending as a major terminal nerve. The lateral cord gives off the lateral branch of the median nerve and terminates as the musculocutaneous nerve; the medial cord gives off the medial branch of the median nerve and terminates as the ulnar nerve; and the posterior cord gives off the axillary nerve and terminates as the radial nerve.  Local anesthetic may be deposited at any point along the brachial plexus, depending on the desired block effects (Figure 46-7): interscalene for shoulder and proximal humerus surgical procedures; and supraclavicular, infraclavicular, and axillary for surgeries distal to the mid-humerus.
Local anesthetic may be deposited at any point along the brachial plexus, depending on the desired block effects (Figure 46-7): interscalene for shoulder and proximal humerus surgical procedures; and supraclavicular, infraclavicular, and axillary for surgeries distal to the mid-humerus.
An interscalene brachial plexus block is indicated for procedures involving the shoulder and upper arm (Figure 46-8). Roots C5-7 are most densely blocked with this approach; and the ulnar nerve originating from C8 and T1 may be spared. Therefore, interscalene blocks are not appropriate for surgery at or distal to the elbow. For complete surgical anesthesia of the shoulder, the C3 and C4 cutaneous branches may need to be supplemented with a superficial cervical plexus block or local infiltration.
Contraindications to an interscalene block include local infection, severe coagulopathy, local anesthetic allergy, and patient refusal.  A properly performed interscalene block invariably blocks the ipsilateral phrenic nerve (completely for nerve stimulation techniques; unclear for ultrasound-guided techniques), so careful consideration should be given to patients with severe pulmonary disease or preexisting contralateral phrenic nerve palsy. The hemidiaphragmatic paresis may result in dyspnea, hypercapnia, and hypoxemia. A Horner’s syndrome (myosis, ptosis, and anhidrosis) may result from proximal tracking of local anesthetic and blockade of sympathetic fibers to the cervicothoracic ganglion. Recurrent laryngeal nerve involvement often induces hoarseness. In a patient with contralateral vocal cord paralysis, respiratory distress may ensue. Other site-specific risks include vertebral artery injection (suspect if immediate seizure activity is observed), spinal or epidural injection, and pneumothorax. Even 1 mL of local anesthetic delivered into the vertebral artery may induce a seizure. Similarly, intrathecal, subdural, and epidural local anesthetic spread is possible. Lastly, pneumothorax is possible due to the close proximity of the pleura.
A properly performed interscalene block invariably blocks the ipsilateral phrenic nerve (completely for nerve stimulation techniques; unclear for ultrasound-guided techniques), so careful consideration should be given to patients with severe pulmonary disease or preexisting contralateral phrenic nerve palsy. The hemidiaphragmatic paresis may result in dyspnea, hypercapnia, and hypoxemia. A Horner’s syndrome (myosis, ptosis, and anhidrosis) may result from proximal tracking of local anesthetic and blockade of sympathetic fibers to the cervicothoracic ganglion. Recurrent laryngeal nerve involvement often induces hoarseness. In a patient with contralateral vocal cord paralysis, respiratory distress may ensue. Other site-specific risks include vertebral artery injection (suspect if immediate seizure activity is observed), spinal or epidural injection, and pneumothorax. Even 1 mL of local anesthetic delivered into the vertebral artery may induce a seizure. Similarly, intrathecal, subdural, and epidural local anesthetic spread is possible. Lastly, pneumothorax is possible due to the close proximity of the pleura.
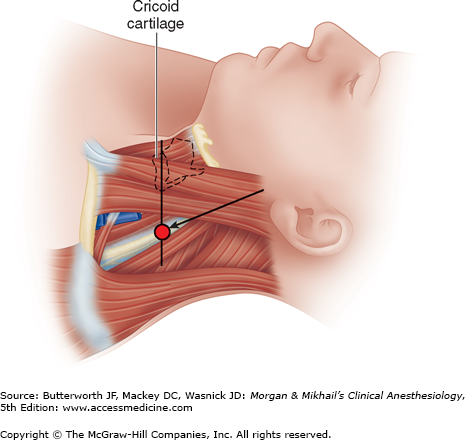
The brachial plexus passes between the anterior and middle scalene muscles at the level of the cricoid cartilage, or C6 (Figure 46-9). Palpation of the interscalene groove is usually accomplished with the patient supine and the head rotated 30° or less to the contralateral side. The external jugular vein often crosses the interscalene groove at the level of the cricoid cartilage. The interscalene groove should not be confused with the groove between the sternocleidomastoid and the anterior scalene muscle, which lies further anterior. Having the patient lift and turn the head against resistance often helps delineate the anatomy. If surgical anesthesia is desired for the entire shoulder, the intercostobrachial nerve must usually be targeted separately with a field block since it originates from T2 and is not affected with an interscalene block. Interscalene perineural infusions provide potent analgesia following shoulder surgery.
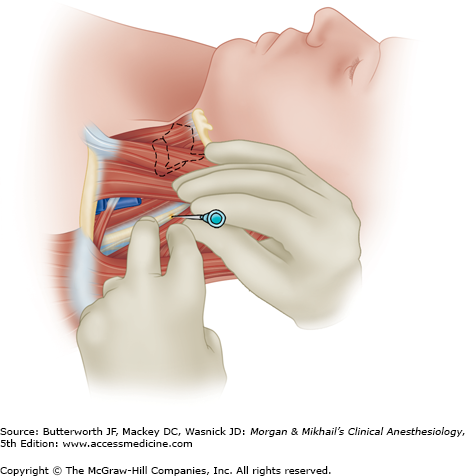
A relatively short (5-cm) insulated needle is usually employed. The interscalene groove is palpated using the nondominant hand, pressing firmly to stabilize the skin against the underlying structures (Figure 46-10). After the skin is anesthetized, the block needle is inserted at a slightly medial and caudad angle and advanced to optimally elicit a motor response of the deltoid or biceps muscles (suggesting stimulation of the superior trunk). A motor response of the diaphragm indicates that the needle is placed in too anterior a direction; a motor response of the trapezius or serratus anterior muscles indicates that the needle is placed in too posterior a direction. If bone (transverse process) is contacted, the needle should be redirected more anteriorly. Aspiration of arterial blood should raise concern for vertebral or carotid artery puncture; the needle should be withdrawn, pressure held for 3-5 min, and landmarks reassessed.
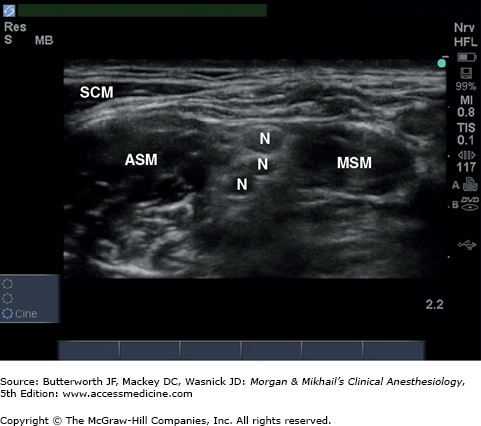
A needle in-plane or out-of-plane technique may be used, and an insulated needle attached to a nerve stimulator can be used to confirm the accuracy of the targeted structure. For both techniques, after identification of the sternocleidomastoid muscle and interscalene groove at the approximate level of C6, a high-frequency linear transducer is placed perpendicular to the course of the interscalene muscles (short axis; Figure 46-11). The brachial plexus and anterior and middle scalene muscles should be visualized in cross-section (Figure 46-12). The brachial plexus at this level appears as three to five hypoechoic circles. The carotid artery and internal jugular vein may be seen lying anterior to the anterior scalene muscle; the sternocleidomastoid is visible superficially as it tapers to form its lateral edge.
For an out-of-plane technique, the block needle is inserted just cephalad to the transducer and advanced in a caudal direction toward the visualized plexus. After careful aspiration for nonappearance of blood, local anesthetic (hypoechoic) spread should occur adjacent to (sometimes surrounding) the plexus.
For an in-plane technique, the needle is inserted just posterior to the ultrasound transducer in a direction exactly parallel to the ultrasound beam. A longer block needle (8 cm) is usually necessary. It may be helpful to have the patient turn slightly laterally with the affected side up to facilitate manipulation of the needle. The needle is advanced through the middle scalene muscle until it has passed through the fascia anteriorly into the interscalene groove. The needle tip and shaft should be visualized during the entire block performance. Depending on visualized spread relative to the target nerve(s), a lower volume (10 mL) may be employed for postoperative analgesia, whereas a larger volume (20-30 mL) is commonly used for surgical anesthesia.
Once described as the “spinal of the arm,” a supraclavicular block offers dense anesthesia of the brachial plexus for surgical procedures at or distal to the elbow (Figure 46-13). Historically, the supraclavicular block fell out of favor due to the high incidence of complications (namely, pneumothorax) that occurred with paresthesia and nerve stimulator techniques. It has seen a resurgence in recent years as the use of ultrasound guidance has theoretically improved safety. The supraclavicular block does not reliably anesthetize the axillary and suprascapular nerves, and thus is not ideal for shoulder surgery. Sparing of distal branches, particularly the ulnar nerve, may occur. Supraclavicular perineural catheters provide inferior analgesia compared with infraclavicular infusion and are often displaced due to a lack of muscle mass to aid catheter retention.
Many of the same precautions that are taken with patient selection for an interscalene block should be exercised with a supraclavicular block. Nearly half of patients undergoing supraclavicular block will experience ipsilateral phrenic nerve palsy, although this incidence may be decreased by using ultrasound guidance, allowing use of a minimal volume of local anesthetic. Horner’s syndrome and recurrent laryngeal nerve palsy may also occur. Pneumothorax and subclavian artery puncture, although theoretically less likely under ultrasound guidance, remain potential risks.
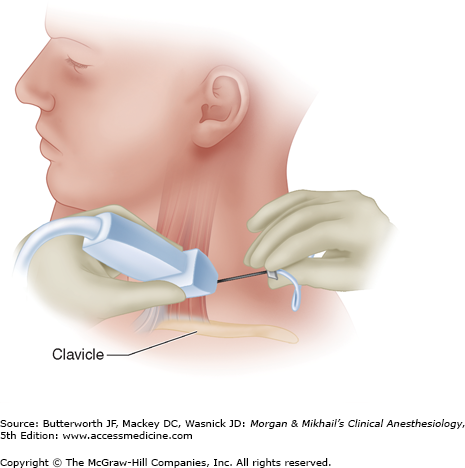
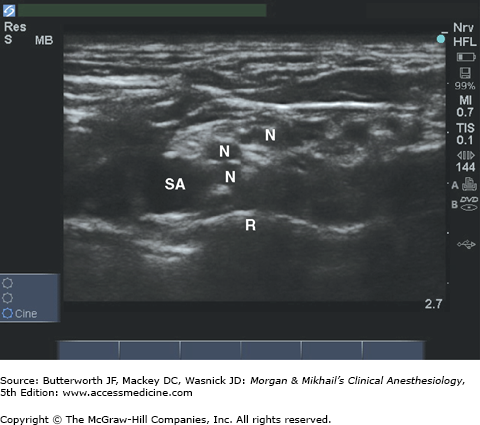
The patient should be supine with the head turned 30o toward the contralateral side. A linear, high-frequency transducer is placed in the supraclavicular fossa superior to the clavicle and angled slightly toward the thorax (Figure 46-14). The subclavian artery should be easily identified. The brachial plexus appears as multiple hypoechoic disks just superficial and lateral to the subclavian artery (Figure 46-15). The first rib should also be identified as a hyperechoic line just deep to the artery. Pleura may be identified adjacent to the rib, and can be distinguished from bone by its movement with breathing.
For an out-of-plane technique, a short, 22-gauge blunt-tipped needle is used. The skin is anesthetized, and the needle inserted just cephalad to the ultrasound transducer in a posterior and caudad direction. After careful aspiration for the nonappearance of blood, 30-40 mL of local anesthetic s injected in 5-mL increments while visualizing local anesthetic spread around the brachial plexus.
For an in-plane technique, a longer needle may be necessary. The needle is inserted lateral to the transducer in a direction parallel to the ultrasound beam. The needle is advanced medially toward the subclavian artery until the tip is visualized near the brachial plexus just lateral and superficial to the artery. Local anesthetic spread should be visualized surrounding the plexus after careful aspiration and incremental injection, which often requires injections in multiple locations and a highly variable volume (20-30 mL).
 Brachial plexus block at the level of the cords provides excellent anesthesia for procedures at or distal to the elbow (Figure 46-16). The upper arm and shoulder are not anesthetized with this approach. As with other brachial plexus blocks, the intercostobrachial nerve (T2 dermatome) is spared. Site-specific risks of the infraclavicular approach include vascular puncture and pneumothorax (although less common than with supraclavicular block). It is often prudent to avoid this approach in patients with vascular catheters in the subclavian region, or patients with an ipsilateral pacemaker.
Brachial plexus block at the level of the cords provides excellent anesthesia for procedures at or distal to the elbow (Figure 46-16). The upper arm and shoulder are not anesthetized with this approach. As with other brachial plexus blocks, the intercostobrachial nerve (T2 dermatome) is spared. Site-specific risks of the infraclavicular approach include vascular puncture and pneumothorax (although less common than with supraclavicular block). It is often prudent to avoid this approach in patients with vascular catheters in the subclavian region, or patients with an ipsilateral pacemaker.
As the brachial plexus traverses beyond the first rib and into the axilla, the cords are arranged around the axillary artery according to their anatomic position: medial, lateral, and posterior.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree