CHAPTER 8 Peripheral nerve blockade for ambulatory surgery
Introduction
Over the last 15–20 years there has been a rapid increase worldwide in the numbers of surgical patients being treated in the ambulatory setting. While the main driving force has been a financial one, there are many benefits for patients including faster return home, greater access to treatment, and innovations in both anesthetic and surgical techniques to facilitate the rapid discharge of patients from hospital.1
Anesthesia provided in the ambulatory setting must be such that the patient is rapidly awake, has minimal postoperative cognitive dysfunction, mild or no pain, a very low risk (<15%) of postoperative nausea and/or vomiting (PONV), is able to commence oral diet within a few hours and is able to ambulate with minimal support (apart from an aid such as a crutch). The ability to void urine is not a requirement unless neuraxial anesthesia has been performed or the patient has undergone a surgical procedure likely to lead to urinary retention. These parameters are necessary in order to avoid unplanned hospital admissions (Box 8.1).
Setting up and running a peripheral nerve blockade service in an ambulatory setting
The starting up and running of a successful PNB service in an ambulatory setting requires consideration of a number of areas,2 which are described in the following paragraphs (Box 8.2).
Working environment
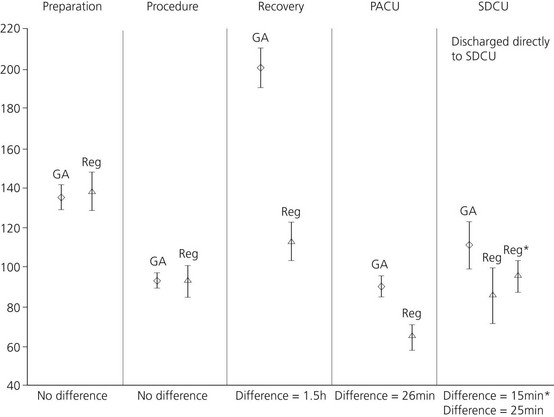
Compared with GA, the performance of PNB takes longer to achieve anesthesia, as the time to onset includes both the time to perform the block and for the LA to act. However, a number of studies3,4 have shown that less time is spent in the operating theatre (20 mins), the PACU (40 mins) and the hospital (40–100 mins), resulting in an overall time gain with PNB compared to GA (Fig. 8.1). There is a 20 minute increase in the amount of time the anesthesiologist spends with the patient.
The use of a dedicated block room has been advocated but this may not be cost effective unless it serves a number of operating theatres and has a regular patient load.4 A more practical solution is to perform the blocks in the PACU, hence utilizing the nursing staff and facilities already available.5
Performance of techniques
Proper preparation is vital for the safe provision of regional anesthesia and this is discussed in greater detail in another chapter of this book. Briefly, the following equipment and drugs are required (Box 8.3) and we would recommend that a dedicated regional anesthesia trolley be organized. Importantly, Intralipid must be stored as part of the emergency drugs.
Although the successful use of Intralipid for LA toxicity in humans has only been documented in case reports, the results have been so dramatic that its use is recommended. Intralipid has been effective in LA toxicity resulting from the long-acting amides bupivacaine, ropivacaine and levobupivacaine. While successful use has been described for the short-acting LA, mepivacaine, to date the only use for lidocaine has been in a pediatric patient who received both lidocaine and ropivacaine for psoas compartment block.6
Modern peripheral nerve blockade is performed using either a nerve-stimulation technique (NST) or ultrasound guidance (USG) to locate the relevant nerves. USG for PNB is generally accepted to result in a faster onset (about 5 minutes), higher success rates (3–10% greater when compared to multi-stimulation techniques) and possibly lower LA volumes compared to NST.7,8 However, whether these differences will result in benefit in the average ambulatory setting is debatable. The advantage of USG may be offset by its significantly increased capital cost.
Choice of local anesthetic
Long-acting LAs such as levobupivacaine and ropivacaine are generally not used because of the prolonged motor blockade. The use of a continuous technique allows lower doses to be used, providing a motor sparing effect, and is useful for more major ambulatory surgery such as shoulder arthroplasty.9 There are no studies in the ambulatory setting comparing the duration of analgesia of long- versus short-acting LAs, but it is reasonable to assume that the benefits seen with long-acting LAs for in patients would be similar. Performing selective analgesic blocks with a long-acting LA while using a short-acting LA for the main block and anesthesia, is an effective technique (for example, for a Dupuytren’s contracture, performing an axillary block with mepivacaine and an ulnar block at the elbow with levobupivacaine).
Postoperative care
Firstly, the anesthesiologist has to be prepared to accept the clinical situation. Even with short-acting LAs, 50% of patients will have residual block present when they are otherwise fit for discharge home.10 The discharge criteria normally used for patients undergoing GA, such as the modified Aldrete score, are inappropriate because they require the patient to move all four limbs.11 A scoring system not requiring limb movement, such as the Postanesthesia discharge scoring system (PADSS), may have to be incorporated into your practice12 (Table 8.1).
Table 8.1 Post-anesthesia discharge scoring system (PADSS) for determining home readiness
| Discharge criteria | Score |
|---|---|
| Vital signs: | |
| Vital signs must be stable and consistent with age and pre-operative baseline | |
| Blood pressure and pulse within 20% of pre-operative baseline | 2 |
| Blood pressure and pulse 20–40% of pre-operative baseline | 1 |
| Blood pressure and pulse >40% of pre-operative baseline | 0 |
| Activity level: | |
| Patient must be able to ambulate at pre-operative level | |
| Steady gait, no dizziness, or meets pre-operative level | 2 |
| Requires assistance | 1 |
| Unable to ambulate | 0 |
| Nausea and vomiting: | |
| Patient should have minimal nausea and vomiting before discharge | |
| Minimal: successfully treated | 2 |
| Moderate: successfully treated with intravenous medication | 1 |
| Severe: continues after repeated treatment | 0 |
| Pain: | |
| Patient should have minimal or no pain before discharge | |
| The level of pain that the patient has should be acceptable to the patient | |
| Pain should be controllable by oral analgesics | |
| The location, type and intensity of pain should be consistent with anticipated postoperative discomfort | |
| Pain acceptable | 2 |
| Pain controllable with oral analgesics | 1 |
| Pain not acceptable | 0 |
| Surgical bleeding: | |
| Postoperative bleeding should be consistent with expected blood loss for the procedure | |
| Minimal: does not require dressing change | 2 |
| Moderate: up to two dressing changes required | 1 |
| Severe: more than three dressing changes required | 0 |
| TOTAL |
Maximum score = 10.
Patients scoring ≥ 9 are fit for discharge.
Modified after Chung F, Chan VW, Ong D. J Clin Anesth 1995;7(6):500–6.
Secondly, discharging a patient home with a long-acting LA block is safe. A study of 1791 patients who underwent a total of 2382 blocks of both the upper and lower limb, with ropivacaine 0.5% in a day surgery setting, found an incidence of paresthesia of 0.25% at 7 days. All had resolved by 3 months. One patient fell getting out of a car following combined femoral and sciatic nerve blocks, with no sequelae.13 Another study found no difference in the incidence of paresthesia at 1 year when comparing axillary block with GA for hand surgery.14
Finally, the patient must be given both verbal and written instructions in the care of the insensate limb. An example information sheet is included (Box 8.4). It should be explained that the limb is numb and must be cared for and protected from injury and temperature extremes until the limb returns to the patient’s own normal sensation and motor function. The use of a sling (upper limb) or crutch (lower limb) is a useful visual reminder. Patients should also be given details of how long the block is expected to last, as well as a contact telephone number should the block persist outside defined parameters, which will depend on the type of LA and/or continuous technique used.
Box 8.4
Patient information sheet post upper limb block
Instructions to patients discharged home after upper limb regional anesthesia
You have received a nerve block of your hand and arm as anesthesia for surgery.
Patients normally experience return of some movement of the hand followed by ‘pins and needles’.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree