Key Concepts
 A well-functioning enhanced recovery program (ERP) uses evidence-based practices to decrease variation in clinical management, minimize organ dysfunction, and accelerate convalescence; it requires adjustments in multiple aspects of care, including surgical and anesthetic techniques, nursing care, physiotherapy, and nutrition support.
A well-functioning enhanced recovery program (ERP) uses evidence-based practices to decrease variation in clinical management, minimize organ dysfunction, and accelerate convalescence; it requires adjustments in multiple aspects of care, including surgical and anesthetic techniques, nursing care, physiotherapy, and nutrition support.
 Persistent postsurgical pain—chronic pain that continues beyond the typical healing period of 1-2 months following surgery, or well past the normal period for postoperative follow-up—is increasingly acknowledged as a common and significant problem following surgery.
Persistent postsurgical pain—chronic pain that continues beyond the typical healing period of 1-2 months following surgery, or well past the normal period for postoperative follow-up—is increasingly acknowledged as a common and significant problem following surgery.
 The magnitude of the surgical stress response is related to the intensity of the surgical stimulus, can be amplified by other factors, including hypothermia and psychological stress, and can be moderated by perioperative interventions, including deeper planes of general anesthesia, neural blockade, and reduction in the degree of surgical invasiveness.
The magnitude of the surgical stress response is related to the intensity of the surgical stimulus, can be amplified by other factors, including hypothermia and psychological stress, and can be moderated by perioperative interventions, including deeper planes of general anesthesia, neural blockade, and reduction in the degree of surgical invasiveness.
 Neuraxial blockade of nociceptive stimuli by epidural and spinal local anesthetics has been shown to blunt the metabolic and neuroendocrine stress response to surgery. In major open abdominal and thoracic procedures, thoracic epidural blockade with local anesthetic provides excellent analgesia, facilitates mobilization and physical therapy, and decreases the incidence and severity of ileus.
Neuraxial blockade of nociceptive stimuli by epidural and spinal local anesthetics has been shown to blunt the metabolic and neuroendocrine stress response to surgery. In major open abdominal and thoracic procedures, thoracic epidural blockade with local anesthetic provides excellent analgesia, facilitates mobilization and physical therapy, and decreases the incidence and severity of ileus.
 By sparing opioid use and minimizing the incidence of systemic opioid-related side effects, epidural analgesia facilitates earlier mobilization and earlier resumption of oral nutrition, expediting exercise activity and attenuating loss of body mass.
By sparing opioid use and minimizing the incidence of systemic opioid-related side effects, epidural analgesia facilitates earlier mobilization and earlier resumption of oral nutrition, expediting exercise activity and attenuating loss of body mass.
 Continuous peripheral nerve blocks with local anesthetics block afferent nociceptive pathways and are an excellent way to reduce the incidence of opioid-related side effects and facilitate recovery.
Continuous peripheral nerve blocks with local anesthetics block afferent nociceptive pathways and are an excellent way to reduce the incidence of opioid-related side effects and facilitate recovery.
 Lidocaine (intravenous bolus of 100 mg or 1.5-2 mg/kg, followed by continuous intravenous infusion of 1.5-3 mg/kg/h or 2-3 mg/min) has analgesic, antihyperalgesic, and antiinflammatory properties.
Lidocaine (intravenous bolus of 100 mg or 1.5-2 mg/kg, followed by continuous intravenous infusion of 1.5-3 mg/kg/h or 2-3 mg/min) has analgesic, antihyperalgesic, and antiinflammatory properties.
 Multimodal analgesia combines different classes of medications, having different (multimodal) pharmacological mechanisms of action and additive or synergistic effects, to control multiple perioperative pathophysiological factors that lead to postoperative pain and its sequelae.
Multimodal analgesia combines different classes of medications, having different (multimodal) pharmacological mechanisms of action and additive or synergistic effects, to control multiple perioperative pathophysiological factors that lead to postoperative pain and its sequelae.
 The addition of nonsteroidal antiinflammatory drugs (NSAIDs) to systemic opioids diminishes postoperative pain intensity, reduces the opioid requirement by approximately 30%, and decreases opioid-related side effects such as postoperative nausea and vomiting and sedation. However, NSAIDs may increase the risk of gastrointestinal and postoperative bleeding, decrease kidney function, and impair wound healing.
The addition of nonsteroidal antiinflammatory drugs (NSAIDs) to systemic opioids diminishes postoperative pain intensity, reduces the opioid requirement by approximately 30%, and decreases opioid-related side effects such as postoperative nausea and vomiting and sedation. However, NSAIDs may increase the risk of gastrointestinal and postoperative bleeding, decrease kidney function, and impair wound healing.
 Opioid administration by patient-controlled analgesia provides better pain control, greater patient satisfaction, and fewer opioid side effects when compared with on-request parenteral opioid administration.
Opioid administration by patient-controlled analgesia provides better pain control, greater patient satisfaction, and fewer opioid side effects when compared with on-request parenteral opioid administration.
 Single-shot and continuous peripheral nerve blockade is frequently utilized for fast-track ambulatory and inpatient orthopedic surgery, and can accelerate recovery from surgery and improve analgesia and patient satisfaction.
Single-shot and continuous peripheral nerve blockade is frequently utilized for fast-track ambulatory and inpatient orthopedic surgery, and can accelerate recovery from surgery and improve analgesia and patient satisfaction.
 Postoperative ileus delays enteral feeding, causes patient discomfort, and is one of the most common causes of prolonged postoperative hospital stay. Nasogastric tubes should be discouraged whenever possible or used for only a very short period of time, even in gastric and hepatic surgery. Multimodal analgesia and nonopioid analgesia techniques shorten the duration of postoperative ileus.
Postoperative ileus delays enteral feeding, causes patient discomfort, and is one of the most common causes of prolonged postoperative hospital stay. Nasogastric tubes should be discouraged whenever possible or used for only a very short period of time, even in gastric and hepatic surgery. Multimodal analgesia and nonopioid analgesia techniques shorten the duration of postoperative ileus.
 Because either excessive, or excessively restricted, perioperative fluid therapy may increase the incidence and severity of postoperative ileus, a goal-directed fluid strategy should be selected to decrease postoperative morbidities and enhance recovery.
Because either excessive, or excessively restricted, perioperative fluid therapy may increase the incidence and severity of postoperative ileus, a goal-directed fluid strategy should be selected to decrease postoperative morbidities and enhance recovery.
Evolution of Enhanced Recovery Programs
Despite increasing numbers of surgical patients who present with complex surgical problems and numerous medical comorbidities, major advances in surgical and anesthetic management have progressively decreased perioperative mortality and morbidity. Further improvement in perioperative outcomes, highlighted by accelerated postoperative convalescence and decreasing occurrence of perioperative complications, will depend on continued evolution of an integrated, multidisciplinary team approach to perioperative care that requires adjustments in multiple aspects of care, including surgical and anesthetic techniques, nursing care, physiotherapy, and nutrition support. The goal is to combine individual evidence-based elements of perioperative care, each of which may have modest benefits when used in isolation, into a tightly coordinated effort that has a synergistic, beneficial effect on surgical outcomes.
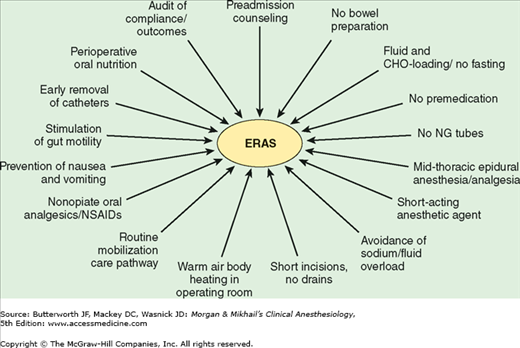
Such coordinated, multidisciplinary perioperative care programs are termed enhanced recovery programs (ERPs), fast-track surgery, or enhanced recovery after surgery (ERAS) (Figure 48-1).  A well-functioning ERP uses evidence-based practices to decrease variation in clinical management, minimize organ dysfunction, and accelerate convalescence (Figure 48-2). Although many publications in the surgical literature have highlighted the positive impact of such programs on surgical outcomes, reports documenting the role of anesthesia and analgesia in these programs are few. Another challenge is determining how to assess the impact of anesthetic management on outcomes in an ERP. Hospital length of stay is the most commonly used measure of success, but in many systems timing of hospital discharge is more directly related to administrative and organizational issues than to discrete milestones in the patient’s postoperative recovery. Little research has been undertaken to define the process of postoperative recovery, and few outcome measures are currently available to confirm that postoperative recovery has been accomplished for a given surgical disease. Other measures of successful implementation of ERPs are reduced readmission and complication rates.
A well-functioning ERP uses evidence-based practices to decrease variation in clinical management, minimize organ dysfunction, and accelerate convalescence (Figure 48-2). Although many publications in the surgical literature have highlighted the positive impact of such programs on surgical outcomes, reports documenting the role of anesthesia and analgesia in these programs are few. Another challenge is determining how to assess the impact of anesthetic management on outcomes in an ERP. Hospital length of stay is the most commonly used measure of success, but in many systems timing of hospital discharge is more directly related to administrative and organizational issues than to discrete milestones in the patient’s postoperative recovery. Little research has been undertaken to define the process of postoperative recovery, and few outcome measures are currently available to confirm that postoperative recovery has been accomplished for a given surgical disease. Other measures of successful implementation of ERPs are reduced readmission and complication rates.
Figure 48-1
Perioperative elements contributing to enhanced recovery after surgery (ERAS). CHO, carbohydrate; NG, nasogastric; NSAID, nonsteroidal antiinflammatory drug. (Reproduced, with permission, from Fearon KC, Ljungqvist O, Von Meyenfeldt M, et al: Enhanced recovery after surgery: A consensus review of clinical care for patients undergoing colonic resection. Clin Nut 2005;24:466.)
It is logical to assume that more effective anesthetic interventions will reduce pain, facilitate earlier postoperative mobilization, and allow earlier resumption of oral feeding. In this context, the role of the anesthesia provider must evolve from merely providing satisfactory anesthetic conditions throughout the operation to a focus on enhancing overall perioperative care through techniques that shorten postoperative convalescence and reduce the likelihood of perioperative complications. These goals can be achieved by optimizing the patient’s preoperative condition, by ablating the adverse effects of the intraoperative neuroendocrine stress response, and by providing pain and symptom control to facilitate the postoperative recovery. In endeavoring to do so, the anesthesiologist must become a perioperative physician and an active participant in the surgical team.
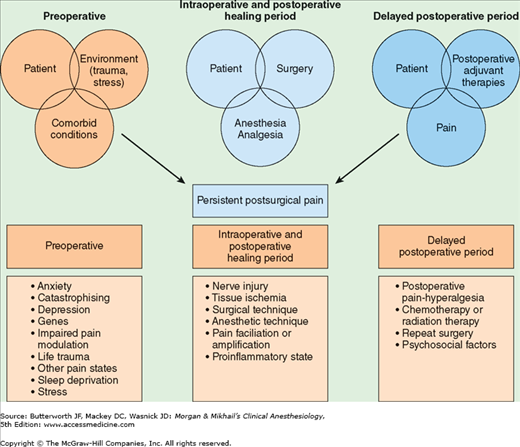
 The problem of persistent postsurgical pain, defined as chronic pain that continues beyond the typical healing period of 1-2 months following surgery—or well past the normal period for postoperative follow-up by anesthesia providers—is increasingly acknowledged as a common and significant issue following surgery. The incidence of persistent postsurgical pain may exceed 30% after some operations, especially amputations, thoracotomy, mastectomy, and inguinal herniorrhaphy. Although the cause is unclear, several risk factors have been identified (Figure 48-3), and aggressive, multimodal perioperative pain control is often suggested as a fundamental preemptive strategy.
The problem of persistent postsurgical pain, defined as chronic pain that continues beyond the typical healing period of 1-2 months following surgery—or well past the normal period for postoperative follow-up by anesthesia providers—is increasingly acknowledged as a common and significant issue following surgery. The incidence of persistent postsurgical pain may exceed 30% after some operations, especially amputations, thoracotomy, mastectomy, and inguinal herniorrhaphy. Although the cause is unclear, several risk factors have been identified (Figure 48-3), and aggressive, multimodal perioperative pain control is often suggested as a fundamental preemptive strategy.
Anesthetic Management-Related Factors Contributing to Enhanced Recovery
Cooperation from the patient and family is essential if an ERP is to be effectively implemented. Preoperative teaching must use plain language and avoid medical jargon. Well-designed printed materials, such as procedure-specific booklets can be given to patients and families with the advice to keep them at the bedside and utilize them during the hospitalization.
Identification of patients at risk for intraoperative and postoperative complications, along with preoperative efforts focusing on any comorbidities, can improve surgical recovery. Preoperative assessment is discussed in detail in Chapter 18. Although international guidelines evaluating the risk for developing cardiovascular, respiratory, or metabolic complications have been extensively reviewed and published, little attention has been given to assessment and optimization of preoperative functional and physiological status. Nonetheless, some recommendations can be made. For example, routine use of β blockers, especially in patients at low risk, has been associated with an increased risk of stroke; however, perioperative β blockers should be continued in patients already receiving this therapy. Perioperative statins appear to decrease postoperative cardiovascular complications and should not be abruptly discontinued perioperatively. Several procedure-specific scoring systems based on patient comorbidity, type of surgery, and biochemical data are being used to predict postoperative mortality and morbidity. In addition, risk-adjusted scoring systems, such as the American College of Surgeons’ National Surgical Quality Improvement Program (NSQIP) and the Society of Thoracic Surgeons’ National Database, can be used to compare outcomes among institutions.
The preoperative period provides not only a time to evaluate surgical risk and optimize medical conditions, but also an opportunity to modify habits that can significantly affect a patient’s short-term and long-term health and quality of life. Smoking, drug abuse, and excessive alcohol use are risk factors for the development of postoperative complications, and preoperative and postoperative interventions aimed at modifying these habits can improve surgical recovery. A recent meta-analysis found that preoperative smoking cessation, for any type of surgery, reduced postoperative complications by 41%, especially those related to wound healing and the lungs.
Many psychological and pharmacological strategies are available to help patients stop excessive alcohol consumption and reduce the risk of alcohol withdrawal. However, the optimal perioperative program has not been identified.
Preoperative fasting and surgical stress induce insulin resistance. Furthermore, patients who are not allowed to drink fluids after an overnight fast and patients who receive a bowel preparation experience dehydration, which may increase discomfort and cause drowsiness and orthostatic lightheadedness. Although fasting has been advocated as a preoperative strategy to minimize the risk of pulmonary aspiration during induction of anesthesia, this benefit must be weighed against the detrimental aspects of this practice.
For instance, research suggests that avoiding preoperative fasting and ensuring adequate hydration and energy supply may moderate postoperative insulin resistance. All international fasting guidelines allow clear fluids up to 2 h prior to induction of anesthesia in patients at low risk for pulmonary aspiration (see Chapter 18). This practice has proved to be safe even in morbidly obese patients. Furthermore, recent studies have shown that preoperative administration of carbohydrate drinks (one 100-g dose administered the night before surgery and a second 50-g dose 2-3 h before induction of anesthesia) is safe; can reduce insulin resistance, hunger, fatigue, and postoperative nausea and vomiting (PONV); and positively influences immune status. Moreover, postoperative nitrogen loss and the loss of skeletal muscle mass are attenuated.
Magnetic resonance imaging studies in healthy volunteers have shown that the residual gastric volume 2 h after 400 mL of oral carbohydrate (12.5% maltodextrins) is minimal and similar to the residual volume after an overnight fast (mean volume of 21 mL). The safety of this practice has been tested in patients with uncomplicated type 2 diabetes mellitus, none of whom showed evidence of worsened risk of aspiration. Further studies of preoperative oral fluid and carbohydrate administration are needed to elaborate their role in improving short- and long-term perioperative outcomes.
Antithrombotic prophylaxis reduces perioperative venous thromboembolism and related morbidity and mortality. Both pneumatic compression devices and anticoagulant medications are now commonly used. Because neuraxial anesthesia techniques are commonly employed for many patients during major abdominal, vascular, thoracic and orthopedic surgery, appropriate timing and administration of antithrombotic agents in these cases is of critical importance in order to avoid the risk of epidural hematoma. International recommendations on the management of anticoagulated patients receiving regional anesthesia have been recently revised and published and are discussed in other chapters.
Appropriate selection and timing of preoperative antibiotic prophylaxis reduces the risk of surgical site infections. Antibiotics should be administered within 1 h before skin incision and, based on their plasma half-life, should be repeated during prolonged surgeries to ensure adequate tissue concentrations. Antibiotic prophylaxis of surgical site infections should be discontinued within 24 h after surgery (current guidelines permit cardiothoracic patients to receive antibiotics for 48 h following surgery).
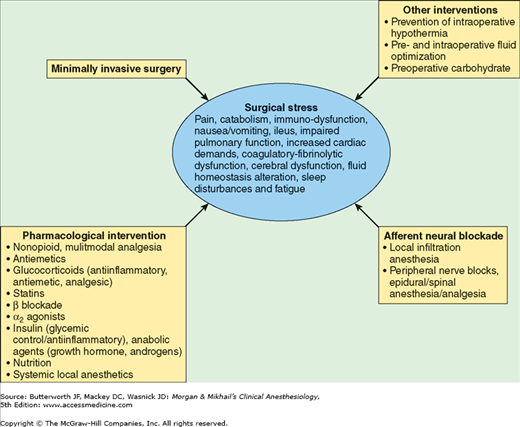
The surgical stress response is characterized by neuroendocrine, metabolic, and inflammatory changes initiated by the surgical incision and subsequent procedures that can adversely affect organ function and perioperative outcomes, especially in elderly and physiologically compromised patients. These responses include a transient but reversible state of insulin resistance, characterized by decreased peripheral glucose uptake and increased endogenous glucose production.  The magnitude of the surgical stress response is related to the intensity of the surgical stimulus; can be amplified by other factors, including hypothermia and psychological stress; and can be moderated by perioperative interventions, including deeper planes of general anesthesia, neural blockade, and reduction in the degree of surgical invasiveness. Much recent effort has focused on developing surgical and anesthetic techniques that reduce the surgical stress response, with the goal of lowering the risk of stress-related organ dysfunction and perioperative complications. An overview of several techniques that have proved effective in ERP protocols follows.
The magnitude of the surgical stress response is related to the intensity of the surgical stimulus; can be amplified by other factors, including hypothermia and psychological stress; and can be moderated by perioperative interventions, including deeper planes of general anesthesia, neural blockade, and reduction in the degree of surgical invasiveness. Much recent effort has focused on developing surgical and anesthetic techniques that reduce the surgical stress response, with the goal of lowering the risk of stress-related organ dysfunction and perioperative complications. An overview of several techniques that have proved effective in ERP protocols follows.
Laparoscopic procedures are associated with a reduced incidence of surgical complications, especially surgical site infections, compared with the same procedures performed in “open” fashion. Published data highlight the safety of minimally invasive procedures in the hands of adequately trained and experienced surgeons. Laparoscopic cholecystectomy results in shorter length of hospital stay and fewer complications compared with open cholecystectomy, and similar results have been reported for colorectal surgery. A longer term salutary impact is achieved when laparoscopic techniques are included in ERPs. A laparoscopic approach is also associated with less morbidity in elderly surgical patients.
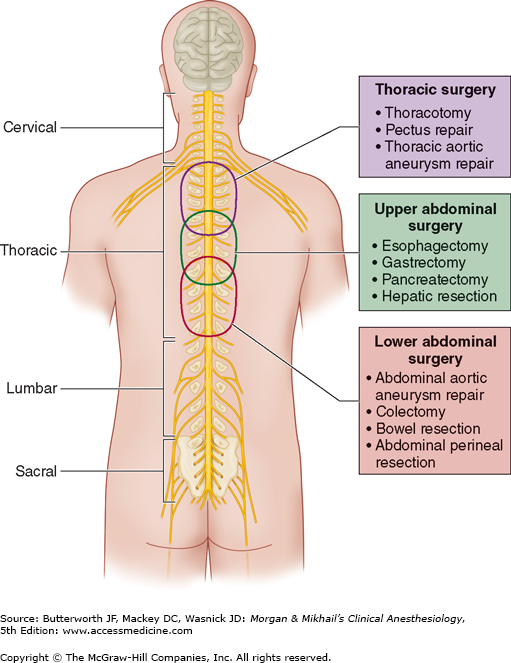
A variety of fast-track surgical procedures have taken advantage of the beneficial clinical and metabolic effects of regional anesthesia/analgesia techniques (Table 48-1).  Neuraxial blockade of nociceptive stimuli by epidural and spinal local anesthetics has been shown to blunt the metabolic and neuroendocrine stress response to surgery. To be effective, the blockade must be established before incision and continued postoperatively. In major open abdominal and thoracic procedures, thoracic epidural blockade with local anesthetic can be a recommended anesthetic component of a postoperative ERP, providing excellent analgesia, facilitating mobilization and physical therapy, and decreasing the incidence and severity of ileus. However, the advantages of neuraxial blockade are not as evident when minimally invasive surgical techniques are used. Lumbar epidural anesthesia/analgesia should be discouraged for abdominal surgery because it often does not provide adequate segmental analgesia for an abdominal incision. In addition, it frequently causes urinary retention and lower limb sensory and motor blockade, increasing the need for urinary drainage catheters (with accompanying increased risk of urinary tract infection), delaying mobilization and recovery, and increasing the risk of falls.
Neuraxial blockade of nociceptive stimuli by epidural and spinal local anesthetics has been shown to blunt the metabolic and neuroendocrine stress response to surgery. To be effective, the blockade must be established before incision and continued postoperatively. In major open abdominal and thoracic procedures, thoracic epidural blockade with local anesthetic can be a recommended anesthetic component of a postoperative ERP, providing excellent analgesia, facilitating mobilization and physical therapy, and decreasing the incidence and severity of ileus. However, the advantages of neuraxial blockade are not as evident when minimally invasive surgical techniques are used. Lumbar epidural anesthesia/analgesia should be discouraged for abdominal surgery because it often does not provide adequate segmental analgesia for an abdominal incision. In addition, it frequently causes urinary retention and lower limb sensory and motor blockade, increasing the need for urinary drainage catheters (with accompanying increased risk of urinary tract infection), delaying mobilization and recovery, and increasing the risk of falls.
| Type of Surgery | Incision | Regional Anesthesia /Analgesia Techniques | Length of Stay |
|---|---|---|---|
| Colorectal resection | Laparotomy, laparoscopy | TEA, wound infusion of ropivacaine, intraperitoneal local anesthetic, intravenous lidocaine | 2-4 d |
| Hernia repair | Open | Local infiltration, INB, TAP | 2-4 h |
| Thoracic surgery | Thoracotomy | TEA, ICB | 1-4 d |
| Esophageal surgery | Laparotomy | TEA | 3-5 d |
| Open aortic surgery | Laparotomy | TEA | 3-5 d |
| Nephrectomy | Laparotomy, laparoscopy | TEA | 2-4 d |
| Arthroplasty (hip, knee) | Open | CPNB (femoral and sciatic), periarticular infiltration | 1-3 d |
Epidural blockade using a solution of local anesthetic and low-dose opioid provides better postoperative analgesia at rest and with movement than systemic opioids (Figure 48-4 and Table 48-2).  By sparing opioid use and minimizing the incidence of systemic opioid-related side effects, epidural analgesia facilitates earlier mobilization and earlier resumption of oral nutrition, expediting exercise activity and attenuating loss of body mass. Neural blockade minimizes postoperative insulin resistance, attenuating the postoperative hyperglycemic response and facilitating utilization of exogenous glucose, thereby preventing postoperative loss of amino acids and conserving lean body mass.
By sparing opioid use and minimizing the incidence of systemic opioid-related side effects, epidural analgesia facilitates earlier mobilization and earlier resumption of oral nutrition, expediting exercise activity and attenuating loss of body mass. Neural blockade minimizes postoperative insulin resistance, attenuating the postoperative hyperglycemic response and facilitating utilization of exogenous glucose, thereby preventing postoperative loss of amino acids and conserving lean body mass.
Figure 48-4
Optimal regions for placing an epidural catheter in the adult spine when administering epidural anesthesia/analgesia for thoracic and abdominal procedures. (Reproduced, with permission, from Manion SC, Brennan TJ: Thoracic epidural analgesia and acute pain management. Anesthesiology 2011;115:181.)