Oxygen Administration and Supraglottic Airways
Michael Shuster
A first priority in treating any critical patient is assessment of the airway and the establishment of a patent airway if one is not already present. Endotracheal intubation requires skill, competence, and recurrent training. Bag- mask ventilation (BMV) is a fundamental skill of emergency airway management that has been taught to health care providers for more than 40 years, but effective BMV is difficult to perform. Supraglottic airways have been adopted both in and out of hospital because they are associated with ease of training, ease of skill maintenance, effectiveness, and paucity of serious complications.
Indications and methods of administering supplementary oxygen
Proper use and technique for supraglottic airways
Bag-mask versus supraglottic airway versus endotracheal intubation
Supplementary Oxygen
Cardiac Arrest
Ventilation using exhaled air, whether mouth-to-mouth or mouth-to-mask rescue breathing, can deliver only about 16% to 17% inspired oxygen concentration to the patient. Under ideal conditions, this can produce an alveolar oxygen tension of only about 80 mm Hg. In cardiac arrest, metabolic requirements may be reduced, but many factors such as low cardiac output, reduced peripheral oxygen delivery, and a wide arteriovenous oxygen difference or underlying respiratory disease and ventilation–perfusion mismatch can contribute to decreased tissue perfusion. Untreated tissue hypoxia leads to anaerobic metabolism, lactate production, and metabolic acidosis, which will blunt the beneficial effects of chemical and electrical therapy. Continued use of expired air will lead to lower and lower blood oxygen concentrations; therefore health care providers should give supplementary 100% inspired oxygen (FiO2 = 1.0) as soon as it is available.
Myocardial Ischemia
Supplementary oxygen is frequently administered in the care of patients encountered in emergency cardiovascular care. For patients with chest discomfort of possible ischemic origin, the administration of oxygen has become routine practice. There is, however, no evidence that supplemental oxygen has beneficial effect on myocardial ischemia in patients with normal oxygen saturation, and some evidence suggests that supplemental oxygen may potentially cause harm. Hence, administration of oxygen for short periods during assessment of chest discomfort and other life-threatening conditions is prudent, but continuing or long-term administration should be based on clear indications.
A series of studies in the 1960s showed that, in both normal patients and patients with myocardial infarction, high-flow oxygen increased arterial pressure, increased systemic vascular resistance, and when oxygen saturation was >90%, reduced cardiac output.1,2,3,4,5,6 In contrast, when arterial oxygen saturations were <90%, oxygen administration increased both oxygen content and cardiac output.7 In another study, in patients with coronary artery disease, a fall in oxygen saturation to between 70% and 85% produced anaerobic metabolism indicative of myocardial ischemia.8 In this same study, there was no evidence that hyperoxia relieved myocardial ischemia in patients with coronary artery disease.
From the acc AHA Guidelines
No evidence is available to support the (routine continuing) administration of oxygen to all patients with acute coronary syndromes in the absence of signs of respiratory distress or arterial hypoxemia. Its use based on the evidence base can be limited to those with questionable respiratory status and documented hypoxemia. Nevertheless, it is the opinion of the Writing Committee that a short period of initial routine oxygen supplementation is reasonable during initial stabilization of the patient, given its safety and the potential for underrecognition of hypoxemia.
In 1976, Madias et al. performed precordial ST-segment mapping in a controlled trial of 17 patients and concluded that oxygen administration may reduce ischemic injury; they demonstrated that administration of oxygen to patients experiencing a myocardial infarction may reduce the sum of ST-segment elevations as well as their number.9,10,11
Also in 1976, a randomized, double-blind, controlled trial of oxygen therapy in the first 24 hours of uncomplicated myocardial infarction found that the group of 80 patients receiving 6 L/min of oxygen by mask for the initial 24-hour period had indications of greater myocardial damage than the group of 77 patients receiving room air. There was a greater proportion of deaths in the group receiving oxygen, 9 of 80 (11.3%) versus 3 of 77 (3.9%), but the difference did not reach statistical significance.12
A systematic review of the evidence for the use of oxygen to treat acute myocardial ischemia found only nine clinical trials in human subjects (randomized and nonrandomized) and concluded that “any effect of oxygen is likely to be marginal so a suitably powered trial is necessary.”13
Current guidelines recommend that supplemental oxygen be provided to patients during an initial period of stabilization and evaluation. Oxygen should be continued when oxygen saturation is <90%, but there is little evidence that oxygen is beneficial beyond this period. There is general consensus that, in patients with ongoing myocardial ischemia or signs of respiratory insufficiency or congestive heart failure, oxygen should be continued and oxygen saturation estimated by pulse oximetry or determined by direct arterial measurement.14,15
Indications for the method and administration of oxygen are general recommendations and require consideration of patient comfort and ongoing or anticipated patient requirements such as the work of breathing and comorbidity. Pulse oximetry can estimate oxygen saturation and methods of administration can be guided by the degree of hypoxia.
Devices Used to Deliver Supplementary Oxygen
Several devices can be used to deliver supplementary oxygen to patients. Beyond the first minutes of cardiac arrest, tissue hypoxia develops. Additional factors that contribute to hypoxia include intrapulmonary shunting with microcirculatory dysfunction and attendant ventilation–perfusion abnormalities. Some patients may also have underlying respiratory disease. Tissue hypoxia leads to anaerobic metabolism and metabolic acidosis. To improve oxygenation, health care providers should give 100% inspired oxygen (FiO2 = 1.0) during basic life support and advanced cardiovascular life support as soon as it becomes available. High inspired oxygen tension will tend to maximize arterial oxygen saturation and, in turn, arterial oxygen content. This will help support oxygen delivery (cardiac output × arterial oxygen content) when cardiac output is limited. This short-term oxygen therapy does not produce oxygen toxicity.
In other patients, supplementary oxygen is given to improve arterial oxygenation and tissue delivery. The amount of oxygen delivered and the method of delivery will depend on several variables. These will include the degree of arterial hypoxemia, underlying condition and airway jeopardy and compromise, respiratory effort, and patient comfort, cooperation, and preference.
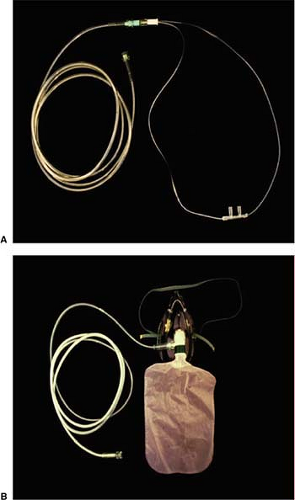
Nasal Cannula
The nasal cannula is a simple, comfortable, inexpensive low-flow oxygen administration device which adds oxygen to room air as the patient inspires (Fig. 17-1A). The inspired oxygen concentration will vary widely depending on the oxygen flow rate through the cannula, the patient’s tidal volume, and the amount of mouth-breathing. For every 1 L/min increase in the oxygen flow rate, the inspired oxygen concentration increases by approximately 4%, to a maximum flow rate of about 6 L/min. Use of a nasal cannula with rates >4 L/min or for prolonged periods may cause local irritation and drying of mucous membranes.
Face Mask
A simple oxygen face mask delivers oxygen to the patient’s nose and mouth. It can deliver a higher concentration of oxygen than is possible with nasal prongs and must be used with a minimum oxygen flow rate of 6 L/min to prevent rebreathing of exhaled carbon dioxide and to maintain increased inspired oxygen concentration. Exhalation ports on either side of the mask allow exhaled air to escape and also allow the patient to entrain room air during inspiration. A flow rate of 6 to 10 L/min is required to deliver an inspired oxygen concentration of 35% to 60%, but the actual concentration delivered is highly dependent on the fit of the mask and the patient’s spontaneous rate of breathing and tidal volume.
Face Mask with Oxygen Reservoir
Adding an oxygen reservoir bag (200 mL) to the face mask makes available higher oxygen concentrations at lower flow rates than are possible with a simple face mask (Fig. 17-1B). A mask with an oxygen reservoir can be either a partial rebreathing mask or a nonrebreathing mask. With a partial rebreathing mask, the first 200 mL of exhaled air flows into the reservoir bag and combines with fresh oxygen flowing into the reservoir, while the remainder of the exhaled gas is expelled through the exhalation ports. Since the initial portion of exhaled gas comes from the upper airway and is not involved in gas exchange, the oxygen concentration in the reservoir remains high. During inspiration, the inspired air will initially come from the bag and
the fresh oxygen inflow. If the oxygen flow rate is maintained above the patient’s minute ventilation and the mask fits securely, an oxygen concentration of 60% to 80% can be achieved. To assess the adequacy of oxygen flow, water mist may be added to the oxygen with a humidifier; thus the mist can be watched to escape from the exhalation ports of the mask during both inspiration and expiration. If mist does not escape during inspiration, room air is being entrained by the patient, effectively reducing the inspired oxygen concentration.
the fresh oxygen inflow. If the oxygen flow rate is maintained above the patient’s minute ventilation and the mask fits securely, an oxygen concentration of 60% to 80% can be achieved. To assess the adequacy of oxygen flow, water mist may be added to the oxygen with a humidifier; thus the mist can be watched to escape from the exhalation ports of the mask during both inspiration and expiration. If mist does not escape during inspiration, room air is being entrained by the patient, effectively reducing the inspired oxygen concentration.
A nonrebreathing mask incorporates a valve into one or both exhalation ports to prevent room air from being entrained during inspiration. In addition, a valve between the reservoir bag and the mask prevents flow of exhaled gas into the reservoir. During inspiration, the patient draws air from the reservoir bag being filled by oxygen inflow. Each 1 L/min of increase in oxygen flow >6 L/min will increase the inspired oxygen concentration by 10%. If oxygen inflow is adjusted to prevent collapse of the reservoir bag (flow rates of 10–15 L/min), inspired oxygen concentrations of 90% to 95% can be achieved provided that the mask is well sealed.
Venturi Mask
The Venturi mask system entrains air into the mask at a specific ratio by passing oxygen through a calibrated opening under pressure. By varying the calibration of the opening, the Venturi mask delivers a reliable oxygen concentration of 24% to 50% as long as the flow rate specified for each caliber of opening is maintained.
Airway Adjuncts
Assessing and Establishing a Patent Airway
The first priority in treating any critical patient is assessment of the airway and the establishment of a patent airway if one is not already present.
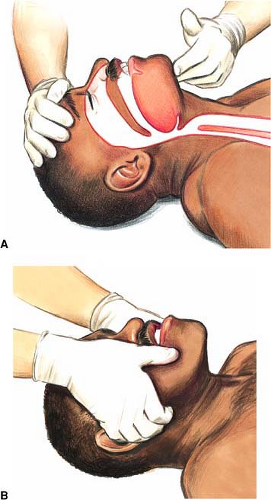
The first priority in treating any critically ill patient is assessment of the airway and the establishment of a patent airway if one is not already present. Without adequate ventilation and oxygenation, circulation cannot be sustained. In the conscious patient, upper airway patency can be compromised by obstruction from a swollen tongue or the soft tissues surrounding the airway, from dentures or other foreign body, or by excessive bleeding or secretions (Fig. 17-2). Obtundation, cyanosis, agitation, retractions, and stridorous or snoring respirations may all be signs of airway or ventilatory compromise. In the unconscious patient, upper airway obstruction results from loss of tone in the submandibular muscles which provide direct support to the tongue and indirect support to the epiglottis. Airway patency is often established simply by repositioning the head and neck but the maneuver may also require chin lift or jaw thrust and insertion of an oropharyngeal or nasopharyngeal airway.
Once airway patency and ventilations are established, consideration must be given to the patient’s ability to protect against aspiration of gastric contents, which can produce significant morbidity and mortality. There is no evidence that the presence of the gag reflex corresponds to airway protective reflexes.17 A gag reflex is an unreliable indicator of the ability to protect the airway as it may be absent in as many as 22% to 37% of normal adults.16,17 The ability of the patient to swallow may be a more reliable indicator, but this is untested. In general, if a maneuver is needed to establish a patent airway, intubation should be considered.
Suspected Cervical Spine or Facial Injury
Airway control and breathing remain top priorities in caring for patients with facial trauma or with suspected cervical spine injury, but the approach to airway management must be altered to minimize the potential for causing inadvertent harm through treatment. Although there is no published case of a spinal cord injury as a result of airway management, the potential for serious cord injury exists. Spine injury should be suspected on the basis of the type and mechanism of injury, and in the presence of any suggestive injury (face, head, neck, multiple trauma) that is apparent. Airway control should be established with in-line stabilization of the neck without a head tilt, using a jaw thrust or chin lift. With the head maintained in the neutral position by one rescuer and protected from excessive flexion, extension, or lateral movement, a second rescuer should perform whatever interventions are required to open the airway and ensure adequate ventilation (Fig. 17-3).
General Considerations
The patient who is immobilized on his or her back, even if airway reflexes are intact, may not be able to cope with excessive salivation or oral bleeding. Suction should be immediately available if required and consideration should be given to how the patient might be safely turned to the side if necessary.
If the patient is breathing spontaneously but unable to protect the airway or if ventilation must be controlled, an advanced airway should be established. Endotracheal or nasotracheal intubation were formerly the only options for advanced airway control short of cricothyrotomy, but excellent options now exist with the availability of supraglottic airways. Endotracheal intubation requires enough space behind the head for the rescuer to work and a sufficient view of the glottis to be able to direct the tube. Endotracheal intubation may be extremely difficult in a patient where limited movement of the head and neck is possible and where bleeding or secretions may obscure the visual field. “Blind” nasotracheal intubation, once recommended only for expert providers, is rarely considered any longer: the failed insertion rate is high and the complications are frequent and significant. Nasotracheal intubation can shear off turbinates, cause major nasal bleeding, or be misdirected into the brain or the retropharyngeal tissues.
Supraglottic airways such as the Combitube or the laryngeal tube are considered to provide excellent protection from aspiration because of the dual cuffs sealing the airway from contamination from above and protecting the airway from regurgitated stomach contents from below. The laryngeal mask airway (LMA), once thought not to provide protection from regurgitation, has not been shown to increase the risk of aspiration compared with face-mask ventilation. The supraglottic airways may be inserted with the rescuer in any position relative to the patient, and insertion requires little or no movement of the head and neck.
Maintaining a Patent Airway with an Airway Adjunct
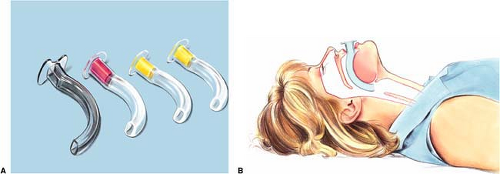
Oropharyngeal Airway
When submandibular muscles relax while a person is in a recumbent position, the tongue falls against the posterior pharyngeal wall and may obstruct the pharynx. The oropharyngeal airway (OPA) is designed to create a conduit through the oropharynx and posterior pharynx, keeping the airway open. The OPA is a rigid, comma-shaped device that has either a hollow inner channel or a solid core and hollow side channels (Fig. 17-4). Because the placement of the OPA stimulates the posterior pharynx, its use should be reserved for the unconscious and unresponsive patient with no cough or gag reflex. There are three methods for placing the OPA: (1) invert the device and rotate it into place when it reaches the posterior pharynx, or (2) turn the device 90 degrees and rotate it into place when it reaches the posterior pharynx, or (3) insert it directly by following the curve of the tongue, with or without the help of a tongue depressor. Whichever technique is chosen, care must be taken not to push the tongue into the posterior pharynx, thus causing airway obstruction. If there are problems ventilating the patient after insertion of the OPA, the device should be removed and reinserted. Although studies have not specifically addressed use of the OPA in cardiac arrest, clinical experience shows that it may aid ventilation with a bag-mask device by preventing the tongue from occluding the airway.
Nasopharyngeal Airway
The nasopharyngeal airway (NPA) is a soft rubber, Silastic, or plastic hollow tube that is inserted through the nose to the posterior pharynx, creating an opening
between the tongue and posterior pharyngeal wall (Fig. 17-5). NPAs are particularly useful when conditions such as a clenched jaw prevent placement of an OPA. NPAs are less likely than OPAs to stimulate the gag reflex, so are a better choice in patients who are not deeply unconscious. In studies of anesthetized patients, 5% to 30% have bleeding with insertion of an NPA.18,19 To minimize or prevent bleeding, care must be taken to first lubricate the NPA well, then insert the airway with the beveled edge facing the septum pushing it into the nares while rotating the airway once it has passed the cartilaginous area of the septum, and directing it along the floor of the nose until the flared end of the NPA is against the nasal orifice. If available, a vasoconstricting nasal spray administered before placement may be helpful. Particular care must be taken when placing the NPA in patients with craniofacial injury: inadvertent intracranial placement of an NPA in patients with basilar skull fracture has been described in four case reports.20,21,22,23
between the tongue and posterior pharyngeal wall (Fig. 17-5). NPAs are particularly useful when conditions such as a clenched jaw prevent placement of an OPA. NPAs are less likely than OPAs to stimulate the gag reflex, so are a better choice in patients who are not deeply unconscious. In studies of anesthetized patients, 5% to 30% have bleeding with insertion of an NPA.18,19 To minimize or prevent bleeding, care must be taken to first lubricate the NPA well, then insert the airway with the beveled edge facing the septum pushing it into the nares while rotating the airway once it has passed the cartilaginous area of the septum, and directing it along the floor of the nose until the flared end of the NPA is against the nasal orifice. If available, a vasoconstricting nasal spray administered before placement may be helpful. Particular care must be taken when placing the NPA in patients with craniofacial injury: inadvertent intracranial placement of an NPA in patients with basilar skull fracture has been described in four case reports.20,21,22,23
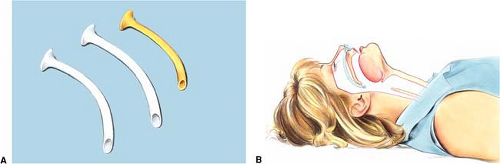 Figure 17-5 • Nasopharyngeal airways. A. Three nasopharyngeal airway devices. B. One nasopharyngeal airway device inserted. |
As with all adjunctive equipment, safe use of the NPA requires adequate training, practice, and retraining. Although studies have not specifically addressed the use of the NPA in cardiac arrest, clinical experience shows that it may aid ventilation with a bag-mask device by preventing the tongue from occluding the airway.
Suctioning
Regurgitation is a frequent occurrence in cardiac arrest, and survival to hospital discharge after aspiration of regurgitated materials is very low.24 Suctioning is thus an essential aspect of airway management. Either a portable or installed suction device should be immediately available for resuscitation emergencies. An installed suction unit should be powerful enough to provide an airflow of >40 L/min at the end of the delivery tube and a vacuum of >300 mm Hg when the tube is clamped. The amount of suction should be adjustable to allow for use in children and intubated patients.
Portable units should provide vacuum pressure and flow that is adequate for pharyngeal suction. The suction device should be fitted with large-bore, nonkinking suction tubing and semirigid pharyngeal tips of sufficient size to suction thick fluids and large particulate matter. Also, suction units must be checked regularly and maintained. When 51 paramedics from nine paramedic units were anonymously surveyed, 26 paramedics (51%) reported difficulties with the portable suction equipment. The difficulty most commonly cited (21 times) was clogging of the tubing as a result of thick emesis. Poor suction power and battery problems were cited 13 times. As a result of frequent problems with portable suction units, some emergency medical services (EMS) systems may choose to carry both a battery-operated device and a manual hand-operated suction pump.25
Both soft flexible and rigid suctioning catheters are available. Rigid catheters (e.g., Yankauer) are used to suction the oropharynx. These are better for suctioning thick secretions and particulate matter (Fig. 17-6). Soft, flexible catheters may be used in the mouth or nose. They can also be used for deep suctioning with an endotra-cheal (ET) tube. Soft, flexible catheters come in sterile wrappers.
Several methods can be used to suction the upper airway and trachea. Central to each of these is the prevention both of hypoxia during the procedure and stimulation of reflexes leading to bradycardia and hypotension. Care must
be taken to prevent damage to the airway structures. During the procedure, the patient’s heart rate, pulse, oxygen saturation, and clinical appearance during suctioning should be monitored. If bradycardia develops, oxygen saturation drops, or the patient’s clinical appearance deteriorates, suctioning must be interrupted at once. High-flow oxygen is then administered until the heart rate returns to normal and the patient’s clinical condition improves. Ventilation is assisted as needed.
be taken to prevent damage to the airway structures. During the procedure, the patient’s heart rate, pulse, oxygen saturation, and clinical appearance during suctioning should be monitored. If bradycardia develops, oxygen saturation drops, or the patient’s clinical appearance deteriorates, suctioning must be interrupted at once. High-flow oxygen is then administered until the heart rate returns to normal and the patient’s clinical condition improves. Ventilation is assisted as needed.
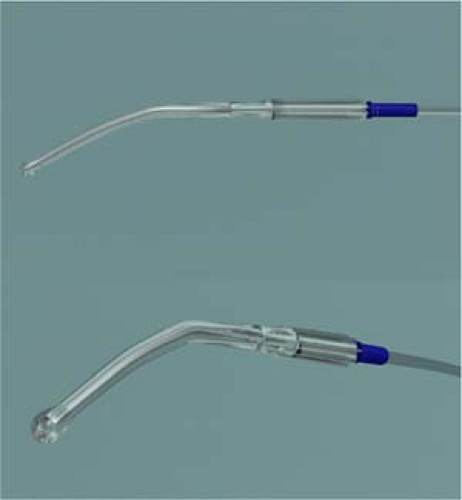 Figure 17-6 • Rigid catheter. Rigid catheters (e.g., Yankauer) are used to suction the oropharynx. These are better for suctioning thick secretions and particulate matter. |
One method for suctioning the oropharynx and trachea through an endotracheal tube is given in Tables 17-1 and 17-2.
Table 17-1 • Oropharyngeal Suctioning Procedure | ||||||
|---|---|---|---|---|---|---|
|
Table 17-2 • Endotracheal Tube Suctioning Procedure | ||||||||
|---|---|---|---|---|---|---|---|---|
|
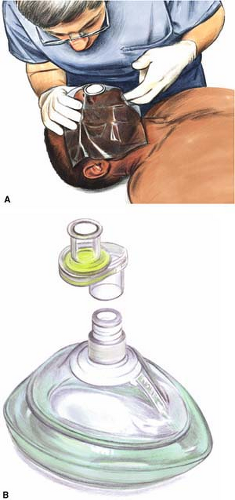
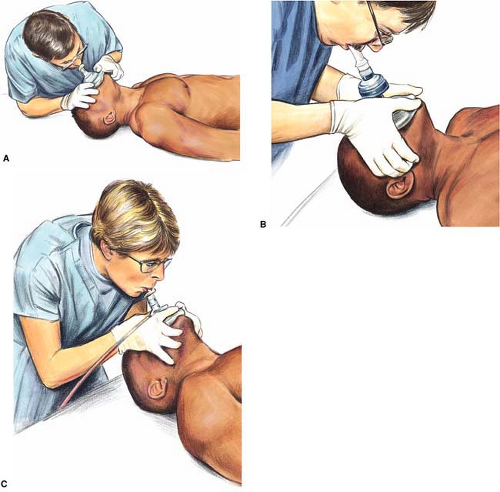
Mouth-to-Barrier Device (Face Shield, Tube, or Mask)
For many years, mouth-to-mouth ventilation has been taught as the basic rescue ventilation technique. Mouth-to-barrier-device has now superseded mouth-to-mouth as the basic ventilation technique recommended for training and for resuscitation, because the interposition of a protective barrier between rescuer and patient addresses a concern that rescuers may have about disease transmission. Although the risk of contagion is very low—there are only 15 reported cases of possible disease transmission during CPR and none during CPR training—surveys of both health care providers and the lay public have repeatedly cited the concern of contagion as a factor affecting the respondent’s expressed willingness to perform mouth-to-mouth ventilation.26,27,28,29,30,31,32,33,34 While the interposition of a barrier device is likely to be more aesthetically pleasing to potential rescuers and will perhaps reduce their fears of contagion, whether rescuers actually undertake CPR more often when the device is available is unknown. Clearly, though, a barrier device can increase the likelihood of CPR performance only if health care providers and other potential rescuers carry such a device with them at all times.
The three types of barrier devices are face shields, tubes, and masks (Fig. 17-7). The devices are typically plastic, they may be disposable or reusable, and they often incorporate a unidirectional valve that will direct the victim’s expired air away from the rescuer. In addition, a one-way valve is available that fits to the inlet of a regular face mask,
so that the mask may be used for mouth-to-mask or bag-mask ventilation. Each of the devices has its own performance characteristics, and effectiveness in protecting against infection transmission varies from device to device. Drawbacks associated with some devices include the creation of inspiratory or expiratory resistance and valve leakage. One study that tested a variety of barrier devices found that few of them had low inspiratory and expiratory resistances and that some of the one-way valves failed.35 In another study, where cultures were performed after mock CPR, none of the masks with one-way valves were culture-positive but one of three face shields that incorporated a one-way valve was culture positive and five of five face shields that did not have a one-way valve were contaminated with the victim’s oral aerobic flora.36 It has not been proven that a barrier device will prevent disease transmission in real-world use, and, given the very low rate of disease transmission that has been reported, it is unlikely that effectiveness will be established.
so that the mask may be used for mouth-to-mask or bag-mask ventilation. Each of the devices has its own performance characteristics, and effectiveness in protecting against infection transmission varies from device to device. Drawbacks associated with some devices include the creation of inspiratory or expiratory resistance and valve leakage. One study that tested a variety of barrier devices found that few of them had low inspiratory and expiratory resistances and that some of the one-way valves failed.35 In another study, where cultures were performed after mock CPR, none of the masks with one-way valves were culture-positive but one of three face shields that incorporated a one-way valve was culture positive and five of five face shields that did not have a one-way valve were contaminated with the victim’s oral aerobic flora.36 It has not been proven that a barrier device will prevent disease transmission in real-world use, and, given the very low rate of disease transmission that has been reported, it is unlikely that effectiveness will be established.
Mouth-to-barrier ventilation, like mouth-to-mouth ventilation, relies on the rescuer’s expired air to ventilate the victim. Most rescuers will have the vital capacity necessary to provide the 5 to 6 L/min of air required for lung inflation but will be able to provide only 17% oxygen, which is the approximate concentration of oxygen in expired air. If an oxygen source is available, the rescuer should wear a nasal cannula or should breathe from the oxygen source between rescue breaths. As soon as possible, the rescuer should switch to a barrier device that has an oxygen inlet, a bag-mask device with attached oxygen, or some other airway adjunct that will allow for the administration supplementary oxygen.
Both tube and face-shield devices fit adults of all sizes, but any given mask fits people only within a particular size range, so the rescuer must have masks of different sizes available. If a mask is too big or too small for the given patient, an air leak will occur, which may reduce the effectiveness of ventilation. A leak can often be tolerated, however, since a full breath often provides more air than is required. The mouth-to-mask technique is easier than bag-mask ventilation, since the rescuer is able to use two hands to correctly elevate the mandible, position the head, and seal the mask to the face. Studies on manikins have found that mouth-to-mask ventilation is capable of delivering significantly larger tidal volumes than bag-mask ventilation, and a similar study on patients after induction of anesthesia endorsed mouth-to-mask ventilation for its ease of use by inexperienced operators.37,38,39,40 No matter which barrier device is used, adequate training is important to ensure effective ventilation.41
Pocket face masks can be used effectively by a provider who is trained in their use and effectively maintains an open airway. Most have side ports for the administration of oxygen. (Fig. 17-8).
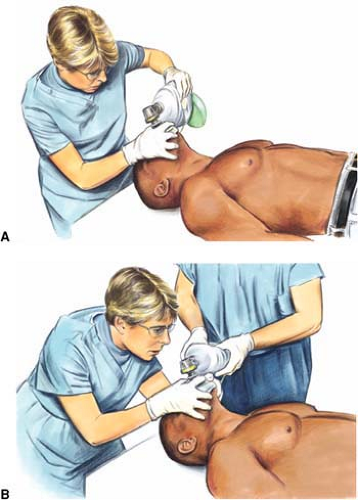
Bag-Mask Devices
Bag-mask ventilation (BMV) is a fundamental skill of emergency airway management that has been taught to health care providers as part of both basic and advanced airway management for more than 40 years. Effective BMV is difficult to perform: in several studies, both inexperienced and experienced providers delivered inadequate tidal volumes
when tested on manikins.42,43,44,45,46,47,48 When tested on anesthetized subjects, where the face is more malleable and the lungs are more compliant than in a manikin, ventilation with a bag-mask is still frequently inadequate: in a study of BMV use by 30 inexperienced nurses, the tidal volume averaged only 239 mL.49 In another study, 10 nurses were able to adequately ventilate 100 patients only 43% of the time.50 Ventilation is unlikely to be performed any better under resuscitation conditions than it is under the controlled conditions of a study.
when tested on manikins.42,43,44,45,46,47,48 When tested on anesthetized subjects, where the face is more malleable and the lungs are more compliant than in a manikin, ventilation with a bag-mask is still frequently inadequate: in a study of BMV use by 30 inexperienced nurses, the tidal volume averaged only 239 mL.49 In another study, 10 nurses were able to adequately ventilate 100 patients only 43% of the time.50 Ventilation is unlikely to be performed any better under resuscitation conditions than it is under the controlled conditions of a study.
In order to provide effective ventilation with a bag-mask, the head, neck, and mandible must be positioned so that the tongue does not obstruct the airway and a correctly sized mask must then be chosen so that a tight seal of the mask to the face can be achieved (Fig. 17-9). Next, the bag must be squeezed in a deliberate, consistent manner over 1 second so as to avoid high inspiratory pressures and thus prevent gastric inflation. Each of these steps may pose difficulty. The head must be tilted back and maintained in neutral or slightly extended position while pulling the jaw forward and pressing the mask down, all with one hand, while the second hand must hold and squeeze the bag (Fig. 17-9A, Table 17-3A). If the patient is edentulous or bearded, the mask seal will be more difficult to achieve. Maintaining a seal in the back of a moving ambulance can be especially challenging.
To improve the mask seal and ensure that the hand squeezing the bag is large enough to hold and compress a sufficient volume of air from the bag, an effective strategy
is for one rescuer to open the airway and seal the mask using both hands, while a second rescuer uses both hands to squeeze the bag. Two rescuers may provide more effective ventilation than one rescuer. When two rescuers use the bag-mask system, one rescuer opens the airway with a head tilt and jaw lift and holds the mask to the face while the other rescuer squeezes the bag (Fig. 17-9B, Table 17-3B). Squeezing the bag requires minimal explanation and can typically be performed even by untrained assistants.
is for one rescuer to open the airway and seal the mask using both hands, while a second rescuer uses both hands to squeeze the bag. Two rescuers may provide more effective ventilation than one rescuer. When two rescuers use the bag-mask system, one rescuer opens the airway with a head tilt and jaw lift and holds the mask to the face while the other rescuer squeezes the bag (Fig. 17-9B, Table 17-3B). Squeezing the bag requires minimal explanation and can typically be performed even by untrained assistants.
Techniques for holding the mask are the same as those for the mouth-to-mask devices described above.51,52,53,54,




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree