Occupational Lung Disease
Pamela Sass MD
Primary care providers are in a key position to prevent, identify, and treat occupational illness. First, providers can identify persons at risk of occupational illness because of exposure to a known occupational hazard. Second, primary care providers who care for a multitude of undifferentiated illnesses are also in a position to link an illness and occupational exposure.
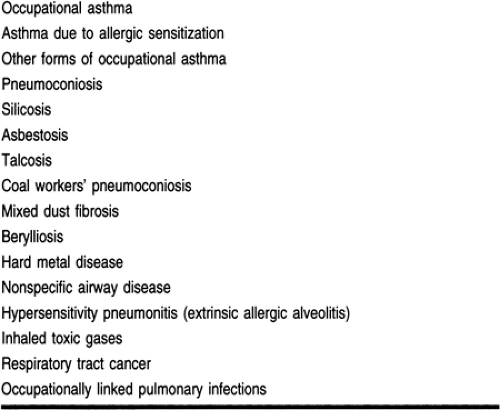
The types of occupational pulmonary disorders are listed in Table 76-1. Two of these diseases, occupational asthma and asbestosis, can be adequately diagnosed and treated only if the primary care provider suspects occupational pulmonary disease and elicits a history of a significant workplace exposure.
Occupational asthma is a relatively common medical condition, but the diagnosis could be easily missed without establishing a link between symptoms and the workplace. Asbestosis, an interstitial disease related to asbestos exposure, becomes symptomatic only after a long latency period. An exposure history and knowledge of the early signs and symptoms are essential to diagnose this disease.
The true incidence and prevalence of occupational illness and injury is not known. The annual cost of occupational disease in the United States has been estimated at more than $6 billion (Campos-Outcalt, 1994).
To identify occupationally related disease, primary care providers must maintain a high degree of suspicion and have the following:
Familiarity with the basic principles of occupational and environmental medicine
Ability to take an occupational and environmental history
Understanding of the worker’s compensation system
Awareness of the ethical, legal, and social implications of occupational and environmental-related conditions
Knowledge of when and how to report hazards to public health and regulatory authorities (Campos-Outcalt, 1994).
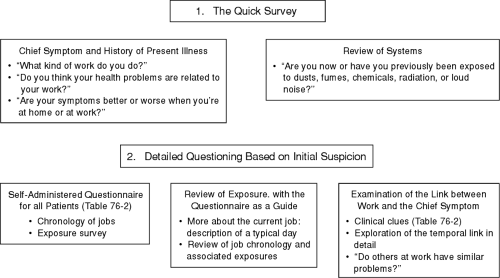
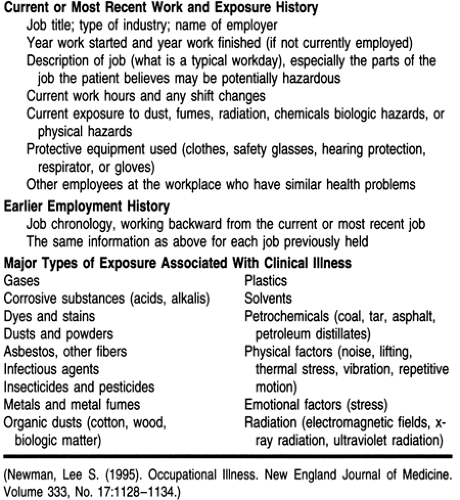
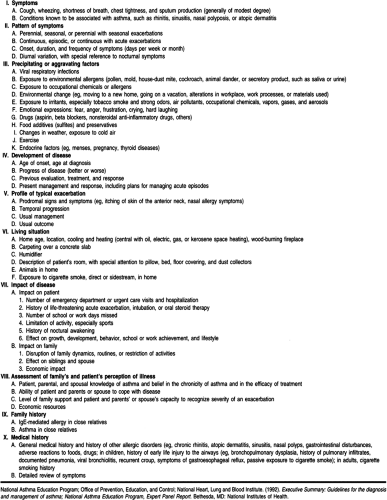
Figure 76-1 outlines an initial clinical approach to the recognition of illness caused by occupational exposure. Table 76-2 lists the essential elements of an occupational history.
Workers in small and medium-sized companies may be at higher risk for exposure to occupational hazards because their employers are less likely to know the characteristics of hazardous substances in use (Sattler, 1992). Immigrant workers and others paid lower wages may also be at higher risk for exposure to hazards; there is a relation between low pay and dangerous working conditions (Robinson, 1986).
OCCUPATIONAL ASTHMA
Anatomy, Physiology, and Pathology
Occupational asthma can be defined as a variable airflow limitation caused by a specific agent in the workplace. It can be caused by either allergic or nonallergic injury or inflammation and is manifested by specific or nonspecific airway hyperresponsiveness (Bates et al, 1992). Allergic occupational asthma develops after a period of allergic sensitization to a substance found at work over a period of months to years and is characterized by intermittent airflow limitation. Although the respiratory symptoms are variable, they always occur at work.
Nonallergic occupational asthma is usually the result of high-level exposures to an irritant gas, fume, aerosol, or vapor. It develops without a latency period and is distinguished by persistent nonspecific airway hyperresponsiveness. Although this nonallergic bronchospasm is referred to as reactive airway dysfunction syndrome, it is not true asthma, even though clinically it presents in a similar fashion (Chan-Yeung, 1990).
Epidemiology
Estimates of the prevalence of occupational asthma have ranged between 2% and 15% of all asthmatic adults. The prevalence within industries varies widely and is determined by the agents used in the workplace. The prevalence within a particular industry depends on the type, source, and concentration of the agent, as well as conditions at the workplace (Bates et al, 1992).
Diagnostic Criteria
The task of the primary care provider is twofold. The first is to diagnose asthma, which may present with varied, atypical symptoms such as chest discomfort, cough, or easy fatigability rather than wheezing and breathlessness (Cullen, 1990). The second task is to connect symptomatic episodes to the workplace.
A sound connection to the workplace can be made with serial peak flow measurements at home and work. Another strategy is to perform the “stop–resume” work test, in which the patient measures and records peak flow rates every 2 hours while awake both at home and work. The record should be kept for at least 2 to 3 weeks at work and then for 10 days off work. A graph of the daily maximum, minimum, and mean peak flows is inspected for deterioration at work and improvement away from work (Alberts & Brooks, 1992). If it is not possible to monitor peak flow rates in this detailed way, the patient should be removed from work for 1 to 2 weeks and then carefully monitored for symptoms on return.
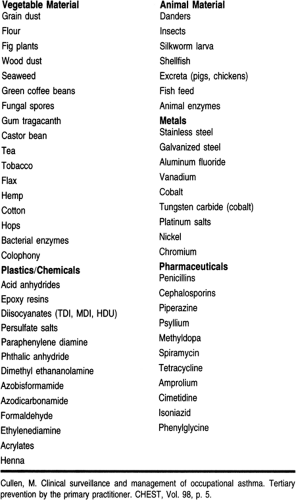
Materials in the workplace that are linked to asthma are listed in Table 76-3. There are many agents causing occupational asthma, and new agents are identified every year. If occupational asthma is suspected and a causative agent cannot be identified, an occupational medicine specialist may perform skin
testing, immunologic studies, and bronchial inhalation challenges.
testing, immunologic studies, and bronchial inhalation challenges.
History and Physical Exam
Any adult presenting with new-onset asthma should be evaluated for occupational asthma. The medical history for these patients is detailed in Table 76-4. The primary care provider should look for aggravating agents in the workplace and should attempt to elicit a relation between symptoms and work. Occupational factors that worsen the symptoms of a patient with stable pre-existing asthma should also be sought.
The physical exam should focus on the respiratory tract and skin (see Chap. 72). Rhinitis, nasal polyps, hyperinflation of the lungs, and a prolonged expiratory phase should be noted. Eczema may suggest the presence of atopy.
Diagnostic Studies
All patients with new onset of asthma-like symptoms should receive a chest radiograph and pulmonary function tests. Other testing was listed in Diagnostic Criteria section.
Treatment Options, Expected Outcomes, and Comprehensive Management
Occupational asthma is treated the same way as is asthma that is not related to the workplace. However, in occupational asthma, an additional goal is to eliminate exposure to the causative agent. If this is not possible, exposure should be minimized.
For patients with occupational asthma secondary to sensitization, removal from the work environment is strongly recommended because even minute exposures to the offending agent may cause fatal bronchospasm (Bates et al, 1992). Worsening asthma is an indication that immediate removal is necessary. Even after removal from the workplace, a patient may continue to be symptomatic from asthma for an indefinite period of time (Chan-Yeung & Malo, 1995).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree