Menopause
Elena M. Umland PharmD
Menopause is the cessation of ovarian function and the consequent ending of menstruation. Estrogen previously produced by the ovaries is absent. This may occur naturally as part of the female life process or by surgical removal of the ovaries. The number and severity of symptoms experienced vary from woman to woman. Therapy is determined only after close examination of menopausal symptoms, risk factors for the long-term effects of menopause, side effects of the therapeutic agents, and patient preferences. Therapeutic management specific to menopause can be augmented and sometimes replaced by other preventive and health management strategies.
Because women are living longer, the long-term consequences of estrogen depletion in menopause have been identified, along with the short-term menopausal symptoms. Shorter-term symptoms include vasomotor hot flashes and urogenital atrophy. These symptoms occur in up to 85% of menopausal women in the United States (Bonk, 1996; Greendale & Judd, 1993). Long-term complications, which may not occur until years after menopause, include osteoporosis and coronary heart disease (CHD). Understanding which patients are at risk for developing these complications is important in undertaking the management of menopause in primary care.
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
Besides cessation of menstruation and ovarian function, menopause also includes cessation of production of the potent estrogen estradiol. The total production of estrogen, however, does not cease entirely: estrogen production continues in the form of estrone, a weaker form of estrogen. Estrone is produced from the conversion of androstenedione in extraglandular tissue, particularly fat tissue (Wilson & Foster, 1992).
Before menopause, the ovary is very responsive to the two pituitary gonadotropins, follicle-stimulating hormone (FSH) and luteinizing hormone (LH). In high enough concentrations, estrogen produced by the ovary signals the pituitary not to release FSH and LH through negative feedback. As the ovaries age and the follicles produced diminish, estrogen concentrations decline, and the release of FSH and LH is no longer blocked. The concentrations of these hormones rise in an attempt to stimulate the ovary. This period of reduced estrogen production and increased concentrations of FSH and LH may occur 10 years or more before the woman’s final menses (Greendale & Judd, 1993). This period is referred to as the perimenopause (Wilson & Foster, 1992).
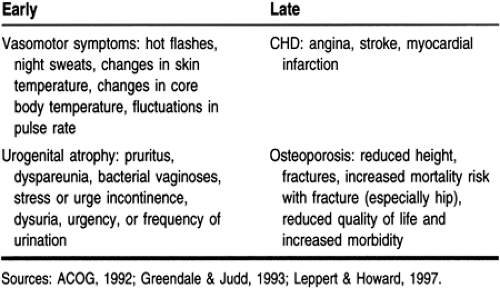
In understanding the consequences of menopausal estrogen depletion, it is important to know the location of estrogen receptors. Estrogen receptors can be found in the urogenital system, cardiovascular system, and bone. Therefore, the lack of stimulation of these receptors results in certain sequelae. Table 67-1 presents the manifestations of menopause and its relative estrogen deficit.
SIGNS AND SYMPTOMS
Early manifestations of menopause may begin in the perimenopausal period. Among the most common are vasomotor symptoms. These symptoms may extend for years; urogenital atrophy, another sequela of estrogen depletion, may last an indefinite period of time.
Vasomotor Symptoms
Vasomotor symptoms result from vasomotor instability caused by estrogen depletion and occur in the majority of menopausal women. Eighty percent experience these symptoms for more than 1 year, whereas 25% to 50% continue to experience them for 5 years or more (American College of Obstetrics and Gynecology [ACOG], 1992; Bonk, 1996). Symptoms range in frequency and severity from mild annoyances to true disruptions of everyday life. Some women experience occasional symptoms; others are affected more than three times daily. Difficulty sleeping and concentrating are not uncommon (Leppert & Howard, 1997). This may occur through mood changes and perceived changes in energy level. As may be expected, all of this has the potential to affect a woman’s personal life, affecting her relationships with family and close friends.
Urogenital Atrophy
Although not all women experience vasomotor symptoms, urogenital atrophy is a sequela of menopause that is difficult to avoid. Such atrophy normally occurs within 2 or 3 years after menopause (Lemcke et al, 1995). Estrogen receptors are located throughout the urogenital system in the vagina, urethra, and bladder. Urogenital atrophy occurs in the absence of estrogen stimulation. However, not all women will report to the provider the related symptoms, which include thinning and drying of the vaginal epithelium and loss of its elasticity, resulting in pruritus and dyspareunia (Leppert & Howard, 1997). Urinary incontinence is a symptom that is more likely to be reported. Each of these symptoms may hinder the woman’s sexual functioning.
Hypoestrogenism also contributes to a decrease in cellular glycogen, with a resultant increase in vaginal pH. This predisposes women to bacterial vaginoses after menopause (Greendale & Judd, 1993).
CLINICAL PEARL
Some of the indications of bacterial vaginosis are the absence of lactobacilli on vaginal microscopy, or the presence of a very low number, and an elevated pH (>4.5). The provider should encourage hygiene that helps to keep the vaginal pH in the normal range (<4.5 [3.8 to 4.2]). Refer to Chapter 69 for more information.
The late sequelae of menopause are identified in Table 67-1. They include CHD and osteoporosis.
Coronary Heart Disease
CHD is the leading cause of death among women in the United States (ACOG, 1992; Carson, 1994; Lemcke et al, 1995). Forty-six percent of deaths in women were secondary to cardiovascular disease, defined as heart disease, stroke, and atherosclerosis (Greendale & Judd, 1993); this figure is 40% in men. Studies have reported a clear association between the loss of ovarian function and CHD. Because menopause is a gradual process, this increased CHD risk is generally not abrupt. It commonly takes several years for the ovary to cease functioning completely. Women who have undergone bilateral oophorectomy are at risk of developing CHD earlier (Greendale & Judd, 1993).
Several mechanisms of cardioprotection afforded by estrogen include improved lipid metabolism, vasodilation, and positive effects on platelet function, endothelial-derived relaxing factor, prostacyclin, and others (Carson, 1994). Some of these functions are related to estrogen receptor stimulation. Estrogen receptors are located throughout the cardiovascular system. Estrogen receptor stimulation may contribute to vasodilation. In the absence of estrogen and estrogen receptor stimulation, vasodilation may not occur to the greatest extent possible.
Osteoporosis
Osteoporosis is a late manifestation of menopause. Its incidence clearly rises after menopause, when bone loss accelerates to 2% to 3% per year. This loss rate continues for 6 to 10 years, exceeding the premenopausal loss rate of 0.3% to 1.2% (Leppert & Howard, 1997). Increased bone loss and the subsequent development of symptomatic osteoporosis are directly related to reduced estrogen production. The effect of estrogen on bone is direct. Estrogen receptors are located throughout bone tissue. When stimulated, they inhibit osteoclastic activity (ie, bone resorption) (Carson, 1994). In the absence of estrogen, osteoclastic activity increases, contributing to enhanced bone breakdown and increased fracture risk.
EPIDEMIOLOGY
The average age of menopause in the United States is 52 years. Because the average female life expectancy is 78 years or more, a woman can expect to spend one third of her life in the postmenopausal stage (Greendale & Judd, 1993). The baby-boomers are now entering their fifth decade of life, with 1.2 million women becoming menopausal annually (Ojeda, 1995). Among the factors found to contribute to early menopause (before the average age of 50 to 52 years) are undernourishment and living at high altitudes. Cigarette smoking and the duration of smoking have also been found to correlate with early menopause (Leppert & Howard, 1997; Wilson & Foster, 1992). Some evidence suggests that the age of maternal menopause may correlate with the age of menopause in the daughter (Torgerson et al, 1987). An exhaustive review of the literature indicated that there is little evidence to suggest that race or socioeconomic status affects the age of menopause.
DIAGNOSTIC CRITERIA
The diagnosis of menopause is based on multiple components. The occurrence of irregular cycles, followed by amenorrhea for 1 year, is a hallmark symptom. Within an age-related context, the presence of perimenopausal or menopausal symptoms of estrogen deficiency is classic. Age, however, is not always indicative of menopause: menopause may occur before 40 or as late as 60 (Speroff, 1994). In addition to symptoms and age, laboratory evaluations may also be performed to help confirm the diagnosis.
HISTORY AND PHYSICAL EXAM
The history is important in the diagnosis of menopause. Questions to be asked are listed in Table 67-2. The physical exam includes a Pap smear and pelvic exam. These can assist in the
evaluation of the physiologic changes that occur secondary to menopause.
evaluation of the physiologic changes that occur secondary to menopause.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree