Fig. 25.1
Anteroposterior view of needle placement in the case presented. Images from Dr. Anitescu Personal Library
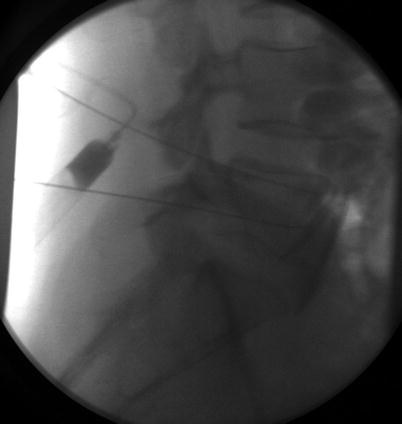
Fig. 25.2
Lateral view of the needle placement in the case presented. Images from Dr. Anitescu Personal Library
Following this procedure, her abdominal pain resolved completely. However, she complained of persistent weakness of hip flexion on the right side only. She was unable to tolerate magnetic resonance imaging (MRI), but a CT study with contrast did not reveal mass effect on lumbosacral nervous structures. She was discharged home with a cane for ambulation and underwent outpatient physical therapy. She experienced gradual improvement of her symptoms over the following month.
25.2 Background
The superior hypogastric plexus is formed by the coalescence of visceral afferent nerve fibers as well as autonomic fibers including lumbar sympathetic and sacral parasympathetic nerve fibers (themselves continuations of lumbar and pelvic splanchnic nerves). The superior hypogastric plexus continues as the inferior hypogastric plexus which is the source of the middle rectal plexus, the prostatic plexus, the vesical plexus, and the uterovaginal plexus. The nerve fibers coalescing at the superior hypogastric plexus have many functions including transmission of nociception from the pelvic viscera [1].
Superior hypogastric plexus blockade has been performed for many years as a treatment for chronic pelvic pain. The procedure has been successfully performed via landmark techniques; however most practitioners now utilize fluoroscopic or computed tomography (CT) guidance. Commonly employed techniques include the classic bilateral, two-needle posterior approach, the single-needle medial paraspinous approach, and the single-needle transdiscal approach as well as the single-needle anterior approach. In the classic bilateral two-needle posterior approach, needle tips are advanced to the anterior margin of either S1 or the L5/S1 intervertebral disc, distal to the bifurcation of the aorta into the common iliac arteries [2, 3]. Temporary blockade for diagnostic and therapeutic purposes may be performed with any number of local anesthetic agents. Chemical neurolysis with concentrated alcohol or phenol is often performed for pain related to pelvic malignancy [3, 4].
Generally, this procedure is considered a safe method for treating severe pain with a relatively low risk of complications when performed appropriately. Expected consequences of this procedure include interruption of the sympathetic innervation distal to the inferior hypogastric nerves. Although this has not been adequately studied, disruption of autonomic function at this level may have negative consequences on bowel, bladder, and sexual function [5]. Based on neural anatomy, physiologic theory, and extrapolation from surgical data, many texts warn of bilateral hypogastric block impairing sexual function in males [6, 7]. Owing in part to lack of adequate knowledge, female sexual function has likely been overlooked on this issue [8–10]. As with any interventional spine procedure, one must be cautious to avoid inadvertent intravascular injection. Should the segmental arteries supplying the spinal cord be disrupted, permanent neurologic deficits may be encountered [11]. Local anesthetic toxicity, infection/abscess formation, hematoma formation, as well as direct needle trauma to vascular, muscular, and neural structures are also possible.
The patient that we described had weakness of her hip flexors. The major hip flexor in the body is the iliopsoas muscle. The iliopsoas is formed by the joining of the iliacus muscle with the psoas muscle. The psoas major is present in all humans and is comprised of a deep part (originating from the transverse processes of L1–L5) and a superficial part (originating from lateral portions of vertebral bodies T12–L4). It is innervated by L2–L4. In less than 50% of humans, the psoas major is joined by psoas minor which originates from the T12–T1 vertebral bodies and attaches to the iliopectineal eminence. It functions as a weak flexor of the lumbar spine [12, 13].
25.3 Case Discussion
In our case, the patient had excellent analgesia from a neurolytic superior hypogastric blockade. However, she suffered an unexpected complication of hip flexion weakness. The differential diagnosis for weakness following superior hypogastric plexus blockade includes: [2–4, 14]
- 1.
Anesthesia or neurolysis of the spinal nerve or its rami
- 2.
Intraneural injection and nerve trauma
- 3.
Abscess
- 4.
Hematoma
- 5.
Disruption of vascular supply to spinal cord (infarction)
- 6.
Musculoskeletal injury
- 1.
Inadvertent anesthesia and/or neurolysis of the spinal nerves are concerns during superior hypogastric blockade. Proper needle positioning as well as use of contrast agent to visualize spread of injectate should be employed. One aims to ensure appropriate spread of injectate in a cephalad-caudad plane immediately anterior to the vertebral column without dangerous spread posterior toward the neural foramen.
- 2.
Intraneural injection is typically characterized by severe pain felt by the patient, as well as relatively high resistance (i.e., low compliance) during the injection. This risk is minimized by avoiding deep sedation that may blunt the patient’s ability to communicate/sense severe pain. Compliance during sympathetic ganglia blocks varies depending on needle and syringe size. This element of feedback is optimized by using a standardized set of syringes and needles. In the event of damage from intraneural injection, treatment is often conservative. Outcomes are variable; pain and/or motorsensory disturbance may be self-limited or may be permanent.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






