Fig. 44.1
Distal forearm level upper limb transplant (hand transplant) (used with permission. Copyright © The Johns Hopkins Health System and the authors)
Fig. 44.2
Above-elbow upper limb transplant (used with permission. Copyright © The Johns Hopkins Health System and the authors)
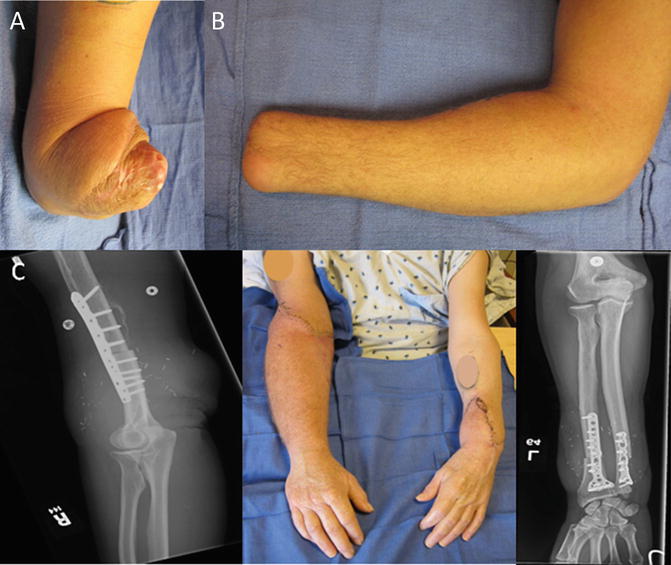
Fig. 44.3
(a) Right proximal forearm (just below elbow) amputation. (b) Left wrist amputation level. (c) Post right above elbow and left distal forearm upper limb transplantations with radiographs of osteosyntheses (a–c: Used with permission. Copyright © The Johns Hopkins Health System and the authors)
Theoretical Benefits and Obstacles to Limb Transplantation
The benefits and obstacles to limb transplantation while in theory are the same, in practice they have been different for upper and lower extremity applications. In theory, both upper and lower limb transplantation provide recipients with improved function by providing a missing limb that will have SOME level of function (certainly not the same level of function as a native limb), an improved or restored body image, likely improvement in phantom or stump pain, and a more comfortable limb replacement than prosthetic devices which are frequently rated to be heavy, painful, uncomfortable, and not as functional as desired by amputees. All transplants require some level of immunosuppression or immunotherapy, require significant amounts of rehabilitation, require nerve regeneration for function, are ultimately limited by nerve regeneration outcomes, and require large and potentially risk-filled surgeries for attachment of the transplanted limbs.
However, in practice, the application of these benefits and obstacles has been more supportive of upper limb than lower limb transplantation. This is partly due to the nature of the tasks required of the upper limb (fine and dexterous manipulation of the surrounding environment, physical sensing of the surrounding environment, communication, etc.) versus the lower limb (weight bearing, ambulation) [4]. For the lower limb, because fine and manipulative tasks are not typically required, the sensation requirement is much less important. Thus, an insensate prosthesis is less of an impediment than in the upper extremity, where the inability to feel objects being manipulated is a functional limitation. In addition, the lower extremity is not usually used in speech for both an aid to verbal communication and in nonverbal communication the way the hands are used. Because the hand is more visible to the patient and those surrounding the patient, there may be more psychological weight placed on upper than lower extremities in regard to body image and “wholeness.” For these reasons, the threshold for amputation of an injured, painful, or nonfunctional hand is very different than the threshold for amputation of an injured, painful, or nonfunctional lower limb [5]. Every possible effort is made to avoid amputation of hands and upper limbs in typical practice due to poorer functional outcomes with an amputation and prosthesis while as it is known that many patients will immediately do better with an amputated lower limb and prosthesis. Thus, prosthetic acceptance is higher in the lower limb amputee than in the upper limb amputee, likely due to a combination of all of the discussed factors [5].
Functional outcomes after reinnervation between upper and lower extremities may be different as well. The limits of motor recovery in nerve regeneration are partially limited by the amount of time necessary to achieve motor end-plate reinnervation before permanent motor end-plate degeneration and muscle loss occur. The distance a nerve must regenerate to achieve motor reinnervation in the foot is longer than that of the hand in most human upper and lower extremities. Thus, the reinnervation potential may be greater in the upper extremity. In addition, most lower extremities tend to carry more muscle mass than upper extremities. Theoretical concerns for ischemia-reperfusion injury to the transplanted limb translating to intra- and immediate postoperative risk to the recipient as well as discussions around the increased antigen load of a lower versus upper extremity also exist. However, the actual influence of these factors in outcome has not truly been compared in a controlled and elective scenario such as a transplant, like it has been observed in more emergent scenarios such as major limb replantation.
World Experience in Limb Transplantation
As previously stated, very little is known about lower limb transplantation in the world experience. The first and only long-term successful transplant currently known involved the transplant of a unilateral leg from a conjoined twin with a fatal cardiac anomaly to the twin that would survive separation [6]. A report of 6-year outcome demonstrated growth and survival of the leg and acceptable, albeit, significantly inferior motor and sensory recovery compared to the contralateral “normal” leg. The second known leg transplant (and the first bilateral leg transplant) was performed in Spain for a 21-year-old man with bilateral above-knee amputations [7]. He had reportedly recovered some active knee flexion and extension and ankle motion, and had begun ambulation training in rehabilitation utilizing parallel bars, but suffered major a setback. He has reportedly had them amputated to stop his immunosuppression due to development of a high-grade malignancy. Two further patients have had unsuccessful attempts at leg transplants combined with hand transplants and are discussed below.
The world experience in hand and upper extremity is much more robust, however. In total, 72 patients with 107 known upper limb transplants have been reported since the first successful hand transplant in 1998 was performed [3]. This includes 37 unilateral upper limb transplants and 35 bilateral upper limb transplants, of which 4 were also combined with either face or leg transplantation. Of these 107 transplants, 24 known losses have occurred, including 4 mortalities. Of these, eight of the transplant losses and three of the four mortalities all occurred in patients undergoing simultaneous hand and face (two patients) or simultaneous hand and leg (two patients transplantation). A single patient survived this surgery and the face transplant also survived, though both hands did not and required removal. The only mortality known involving only hand transplantation occurred in a bilateral transplant attempt which was the first performed in Mexico. The same center has subsequently performed a successful transplant [3]. Of the remaining hand transplant patients that underwent only isolated unilateral or bilateral hand transplantation, 3 of the remaining 14 lost limbs were acute losses (immediate perioperative period) and 7 occurred in a single group’s experience in China where access to immunosuppression was questionable and losses were blamed on noncompliance. The remaining losses come from three patients in the USA and France where non-compliance [3] and transplant vasculopathy [1], possibly, as a sign of chronic rejection, in a compliant patient, were the documented causes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








