Fig. 20.1
Intraoperative image of incision and instrumentation used for MIVAT
Robotic assisted thyroid surgery through either a transaxillary or axillo-breast approach avoids a cervical incision altogether (Fig. 20.2a, b). The ideal patients for this approach have a small body habitus, low body mass index (BMI), and a normal-sized thyroid with small tumors. The vast majority of studies evaluating these techniques are from South Korea. The largest study to date [27] included 3,000 patients with thyroid cancer (99.3 % papillary, 0.4 % follicular, and 0.3 % medullary) who had robotic assisted thyroidectomy through an axillary approach. The average patient BMI was 22.2 ± 3.1, and the average tumor size was 0.7 cm ± 0.6 cm. A total thyroidectomy was performed on 1,090 patients (36 %) and less than total thyroidectomy on 1,910 patients (64 %). The mean operative time was 125 ± 33 min. The most common complications observed were transient hypoparathyroidism (37.4 %), permanent hypoparathyroidism (1.1 %), transient RLN injury (1.2 %), and permanent RLN injury (0.3 %). The technique-specific complications were axillary skin flap perforation in three patients and brachial plexus traction injuries in four patients. Post-operative chest wall numbness was also reported. Other studies have reported additional complications, such as esophageal perforation and higher risks of hematoma formation. A meta-analysis by Sun et al. [28] comparing robotically assisted to conventional thyroidectomy included 11 studies with 726 patients undergoing robotic surgery, and 1,205 undergoing conventional thyroidectomy for either thyroid cancer or thyroid nodules. The robotic group was younger (40.5 vs. 49.2 years, respectively), had a lower BMI (23.1 vs. 24.2), and was less likely to undergo total thyroidectomy (58.1 % vs. 75.1 %). The tumors were small, with a mean size of 8 mm. None of the studies evaluated cost. The mean operative time was 77 min longer for the robotic group (p < 0.001). There was no significant difference between the groups in the frequency of RLN injury, hypoparathyroidism, postoperative hematoma, or seroma. The robotic group had higher cosmetic satisfaction scores, but follow up was only 3 months, and validated patient questionnaires were not used.
Fig. 20.2
(a) Port site location for robotic thyroidectomy: transaxillary approach. (b) Port site location for robotic thyroidectomy: axillo-breast approach
Although there was initial enthusiasm for minimally invasive techniques for thyroidectomy in the USA, the technology has not been embraced except in select centers. Critics of MIVAT and the robotically assisted thyroidectomy have identified the limited applicability of these techniques to a select group of patients [29]. Furthermore, these techniques are associated with longer operative times, novel possible complications, and increased resource utilization without long-term oncological follow-up, and a small cosmetic benefit.
Outpatient Thyroidectomy
In recent years, outpatient thyroidectomy has become increasingly frequent. Several studies, comprised of more than 4,500 patients, have reported the safe implementation of ambulatory thyroidectomy [30]. The frequency of postoperative hematoma in these studies ranged from 0 to 2 %, with no fatalities. Hypocalcemia occurred in 0–10 % of patients, and hospital readmission was required in 0–3.9 % of patients. In 2013, the American Thyroid Association published a statement on outpatient thyroidectomy to identify eligibility criteria and factors that should be considered in order to safely and efficiently perform thyroidectomy in an ambulatory setting. The statement stressed the importance of careful preoperative patient selection, postoperative evaluation prior to discharge, patient education regarding the early identification and treatment of postoperative complications, and communication between patient and the care team. Suggested eligibility criteria for outpatient thyroidectomy included: no major comorbidities, an understanding of preoperative education, a social setting conducive to safe postoperative care, an available primary care giver, and proximity to a skilled facility. Factors identified that were felt to be relative contraindications to outpatient thyroidectomy included massive goiter, extensive substernal goiter, locally advanced cancer, challenging hemostasis, Graves’ disease, severe thyroiditis, significant medical comorbidities, and social barriers to care. After outpatient thyroid surgery, patients should be observed for at least 2 h and should meet discharge criteria. These included: ability to take liquids, adequate pain control, ability to void, adequate oxygenation and blood pressure, and satisfactory postoperative evaluation without concern for hematoma, dysphonia, dysphagia, or dyspnea. While experienced surgeons can safely perform outpatient thyroidectomy, it is essential that patients are carefully selected and a mechanism is set in place to rapidly and safely identify and treat postoperative complications. This requires an experienced, multidisciplinary care team as well as an experienced surgeon.
Parathyroid
Preoperative Imaging
Traditionally, parathyroidectomy was performed with a bilateral neck exploration and excision of the abnormal parathyroid gland(s). Advances in radiological imaging have allowed improved preoperative localization of the hyperfunctioning parathyroid gland(s), thus permitting a focused minimally invasive parathyroidectomy. The most well established imaging modalities are ultrasound (US) and sestamibi imaging. US is widely available (Fig. 20.3), inexpensive, evaluates the thyroid for concomitant pathology, and does not expose patients to ionizing radiation. However, it is user dependent, cannot evaluate ectopic locations, and performs poorly for patients with enlarged nodular goiters or challenging body habitus. Sestamibi is a radiocolloid that is retained in parathyroid adenomas, but not in the thyroid gland or other surrounding tissue. Sestamibi scanning with the addition of single photon emission computed tomography (SPECT) has been used to allow for more precise localization of the abnormal parathyroid gland(s) in a three-dimensional approach (Fig. 20.4). Sestamibi/SPECT imaging is widely available, operator independent, and can evaluate for ectopic locations. Nonetheless, expert radiologists are needed to accurately read the scans, and the technique is expensive, time consuming, and exposes patients to ionizing radiation.
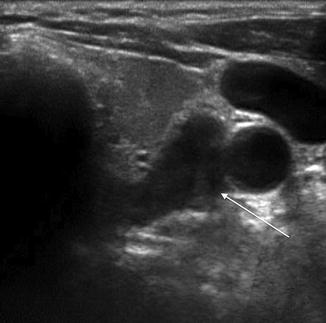

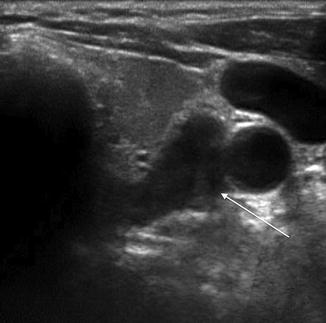
Fig. 20.3
Ultrasound of left superior parathyroid adenoma (arrow) with typical hypoechoic appearance

Fig. 20.4
Sestamibi SPECT-CT demonstrating a right superior parathyroid adenoma (arrow) in the tracheoesophageal groove
Historically, standard computed tomography (CT) has played little role in localization of hyperfunctioning parathyroid glands because of low sensitivity for parathyroid adenomas. Recent modifications of the conventional 3-dimensional anatomic protocol, termed four-dimensional computed tomography (4D-CT), have been developed. The term 4D-CT originates from the added “dimension” of timing of the scanning protocol based on the intravenous contrast phases. Hyperfunctioning parathyroid glands rapidly take up and wash out contrast in comparison to the surrounding thyroid tissue and lymph nodes, thus enabling accurate localization (Fig. 20.5). The images obtained can precisely locate hyperfunctioning glands. In a study by Rodgers et al. [31], 75 patients with primary hyperparathyroidism underwent US, Sestamibi/SPECT, and 4D-CT. The sensitivity for localization of the abnormal parathyroid glands for 4D-CT (88 %) was superior to SPECT (65 %) and US (57 %). Also, 4D-CT identified 45 % of patients who ultimately had multigland disease in contrast to US or SPECT, which identified none of these patients. Advantages of 4D-CT are that it is operator independent, intermediate in cost, and evaluates ectopic locations. However, it is not widely available, requires expert radiologist interpretation, should not be used in patients with renal insufficiency due to the intravenous contrast load, and exposes patients to relatively higher doses of ionizing radiation.
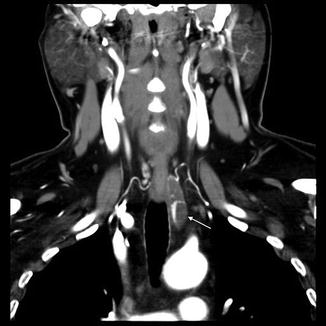
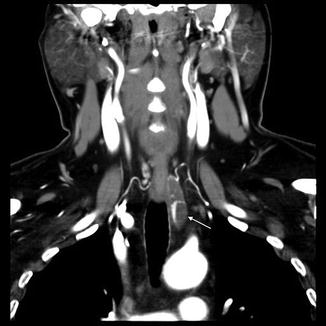
Fig. 20.5
4-Dimensional CT scan of cystic parathyroid (arrow) with internal septations located in the upper mediastinum
There is considerable debate among surgeons regarding which of these imaging modalities is the best for preoperative localization for patients with primary hyperparathyroidism. A meta-analysis by Cheung et al. [32] of 43 studies evaluated preoperative localization techniques for primary hyperparathyroidism comparing US, SPECT, and 4D-CT. US and SPECT had similar pooled sensitivities of 76 % and 79 %, respectively. Although there was an insufficient number of 4D-CT studies (only 2), the weighted sensitivity was 89 %. The authors cautiously concluded that 4D-CT shows great promise and may allow better localization, but more studies need to be performed to confirm these results. Cost-effectiveness studies have also been done to determine which preoperative imaging techniques or combination of techniques is most effective. A study by Wang et al. [33] determined that US + SPECT, and, if discordant, followed by 4D-CT was the most cost-effective algorithm because it reduced the need for bilateral neck exploration and increased the possibility of undergoing minimally invasive parathyroidectomy, which was always associated with lower costs. However, the results were dependent on the sensitivity of each imaging technique, and this varies among institutions. Accordingly, each institution should evaluate their own data to determine the optimal imaging algorithm at that institution for patients with primary hyperparathyroidism.
Minimally Invasive Parathyroidectomy
The advent of preoperative imaging techniques and intraoperative parathyroid hormone (ioPTH) monitoring has permitted experienced surgeons to perform focused minimally invasive parathyroidectomy (MIP) for the majority of their patients. Patients with preoperative localization identifying a hyperfunctioning parathyroid gland are candidates for a focused, minimally invasive procedure. The surgery is performed using regional anesthesia with a surgeon-performed superficial cervical plexus block and mild sedation, using rapid, intraoperative PTH monitoring to assure adequate parathyroidectomy in an ambulatory setting. If needed or based on patient preference, general anesthesia can be used.
This technique involves the following general protocol: prior to the surgical incision, a baseline rapid, intraoperative PTH level is obtained. A 2–4 cm cervical incision is created, and the abnormal parathyroid gland identified and excised. Intraoperative PTH levels are obtained at the time of gland excision and at 5, 10, and 15 min post-excision. Intraoperative criteria for a successful parathyroidectomy are a drop of the intraoperative PTH level by greater than 50–65 % of baseline (typically at 10 min, but this can vary based on a number of factors, including the starting level, amount of gland manipulation during the dissection, and renal clearance), and in to the normal range. If the criteria are met, the procedure is terminated. If the 15 min sample fails to decrease sufficiently, additional cervical exploration is performed to evaluate for multigland disease. In circumstances where PTH may be metabolized more slowly (such as elderly patients or those with renal or hepatic insufficiency), additional intraoperative PTH levels can be obtained after 10–15 min prior to undertaking additional exploration. The success of the minimally invasive parathyroidectomy has been confirmed by several studies, with cure and recurrence rates that are similar to standard bilateral neck exploration [34]. In a study by Udelsman et al. [35], 1,650 patients underwent parathyroidectomy by a single surgeon. Bilateral neck exploration was performed in 613 patients and minimally invasive parathyroidectomy in 1,037 cases. The cure rate for the minimally invasive technique was superior to bilateral neck exploration (99.4 % vs. 97.1 %, respectively; p < 0.001), and the complication rate was lower (1.5 % vs. 3.1 %, p = 0.02). In addition, minimally invasive parathyroidectomy was associated with a shorter mean hospital length of stay compared to bilateral neck dissection patients (0.2 vs. 1.3 days, p < 0.0001), and the total hospital charges were less by $1,471 per case.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








