Junctional arrhythmias
Junctional arrhythmias originate in the atrioventricular (AV) junction—the area in and around the AV node and the bundle of His. The specialized pacemaker cells in the AV junction take over as the heart’s pacemaker if the sinoatrial (SA) node fails to function properly or if the electrical impulses originating in the SA node are blocked. These junctional pacemaker cells have an inherent firing rate of 40 to 60 beats/minute.
In normal impulse conduction, the AV node slows transmission of the impulse from the atria to the ventricles, which allows the ventricles to fill as much as possible before they contract. However, these impulses don’t always follow the normal conduction pathway. (See Conduction in Wolff-Parkinson-White syndrome, page 142.)
Because of the location of the AV junction within the conduction pathway, electrical impulses originating in this area cause abnormal depolarization of the heart. The impulse is conducted in a retrograde (backward) fashion to depolarize the atria, and antegrade (forward) to depolarize the ventricles.
Depolarization of the atria can precede depolarization of the ventricles, or the ventricles can be depolarized before the atria. Depolarization of the atria and ventricles can also occur simultaneously. Retrograde depolarization of the atria results in inverted P waves in leads II, III, and aVF, leads in which you would normally see upright P waves. (See Locating the P wave, page 143.)
Keep in mind that arrhythmias causing inverted P waves on an ECG may originate in the atria or AV junction. Atrial arrhythmias are sometimes mistaken for junctional arrhythmias because impulses are generated so low in the atria that they cause retrograde
depolarization and inverted P waves. Looking at the PR interval will help you determine whether an arrhythmia is atrial or junctional. An arrhythmia with an inverted P wave before the QRS complex and with a normal PR interval (0.12 to 0.20 second) originates in the atria. An arrhythmia with a PR interval less than 0.12 second originates in the AV junction.
depolarization and inverted P waves. Looking at the PR interval will help you determine whether an arrhythmia is atrial or junctional. An arrhythmia with an inverted P wave before the QRS complex and with a normal PR interval (0.12 to 0.20 second) originates in the atria. An arrhythmia with a PR interval less than 0.12 second originates in the AV junction.
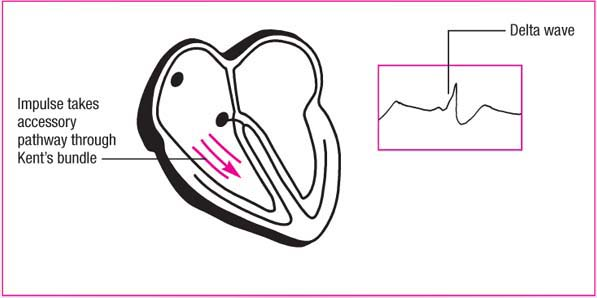
Conduction in Wolff-Parkinson-White syndrome
Electrical impulses in the heart don’t always follow normal conduction pathways. In preexcitation syndromes, electrical impulses enter the ventricles from the atria through an accessory pathway that bypasses the atrioventricular junction. Wolff-Parkinson-White (WPW) syndrome is a common type of preexcitation syndrome.
WPW syndrome commonly occurs in young children and in adults ages 20 to 35. The syndrome causes the PR interval to shorten and the QRS complex to lengthen as a result of a delta wave. Delta waves, which in WPW occur just before normal ventricular depolarization, are produced as a result of the premature depolarization or preexcitation of a portion of the ventricles.
WPW is clinically significant because the accessory pathway—in this case, Kent’s bundle—may result in paroxysmal tachyarrhythmias by reentry and rapid conduction mechanisms.
 |
Junctional arrhythmias include premature junctional contractions, junctional escape rhythm, accelerated junctional rhythm, and junctional tachycardia.
Premature junctional contractions
A premature junctional contraction (PJC) is a junctional beat
that comes from the AV junction before the next expected sinus beat; it interrupts the underlying rhythm and causes an irregular rhythm. These ectopic beats commonly occur as a result of enhanced automaticity in the junctional tissue or bundle of His. As with all impulses generated in the AV junction, the atria are depolarized in a retrograde fashion, causing an inverted P wave. The ventricles are depolarized normally. (See Recognizing a PJC, page 144.)
that comes from the AV junction before the next expected sinus beat; it interrupts the underlying rhythm and causes an irregular rhythm. These ectopic beats commonly occur as a result of enhanced automaticity in the junctional tissue or bundle of His. As with all impulses generated in the AV junction, the atria are depolarized in a retrograde fashion, causing an inverted P wave. The ventricles are depolarized normally. (See Recognizing a PJC, page 144.)
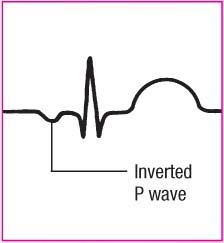
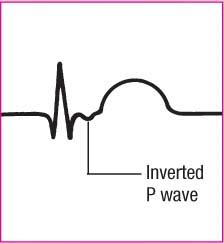
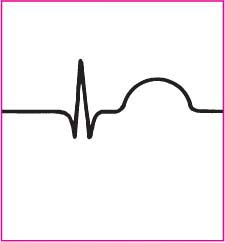
Locating the P wave
When the specialized pacemaker cells in the atrioventricular junction take over as the dominant pacemaker of the heart:
depolarization of the atria can precede depolarization of the ventricles
the ventricles can be depolarized before the atria
simultaneous depolarization of the atria and ventricles can occur.
The rhythm strips shown here demonstrate the various locations of the P waves in junctional arrhythmias, depending on the direction of depolarization.
Causes
PJCs may be caused by digoxin (Lanoxin) toxicity, excessive caffeine intake, amphetamine ingestion, excessive alcohol intake, excessive nicotine intake, stress, coronary artery disease, myocardial ischemia, valvular heart disease, pericarditis, heart failure, chronic obstructive pulmonary
disease, hyperthyroidism, electrolyte imbalances, or inflammatory changes in the AV junction after heart surgery.
disease, hyperthyroidism, electrolyte imbalances, or inflammatory changes in the AV junction after heart surgery.
Recognizing a PJC
To help you recognize a premature junctional contraction (PJC), review this sample rhythm strip.
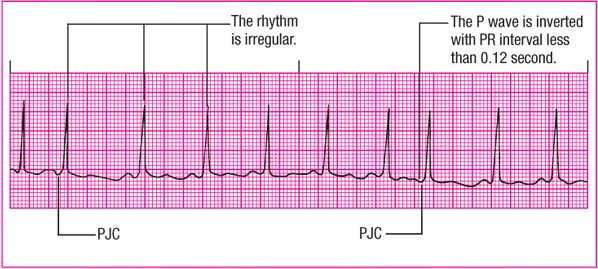 |
Rhythm: Atrial and ventricular—Irregular
Rate: 100 beats/minute
P wave: Inverted and precedes the QRS complex
PR interval: 0.14 second for the underlying rhythm and 0.06 second for the PJC
QRS complex: 0.06 second
T wave: Normal configuration
QT interval: 0.36 second
Other: Pause after PJC
Clinical significance
PJCs are generally considered harmless unless they occur frequently—typically defined as more than six per minute. Frequent PJCs indicate junctional irritability and can precipitate a more serious arrhythmia, such as junctional tachycardia. In patients taking digoxin, PJCs are a common early sign of toxicity.
ECG characteristics
Rhythm: Atrial and ventricular rhythms are irregular during PJCs; the underlying rhythm may be regular.
Rate: Atrial and ventricular rates reflect the underlying rhythm.
P wave: The P wave is usually inverted. It may occur before or after the QRS complex or may appear absent when hidden in the QRS complex. Look for an inverted P wave in leads II, III, and aVF. Depending on the initial direction of depolarization, the
P wave may fall before, during, or after the QRS complex.
PR interval: If the P wave precedes the QRS complex, the PR interval is shortened (less than 0.12 second); otherwise, it can’t be measured.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree