CHAPTER 35
Intradiscal Electrothermal Therapy
INTRODUCTION
Discogenic pain has been implicated as the etiology of low back pain in approximately 45% of patients with axial low back pain.1–3 Despite this relatively large incidence, discogenic pain diagnosis and treatment remains controversial, as many patients are relegated to surgery secondary to an antiquated treatment algorithm and lack of a clear minimally invasive alternative.
IDET was introduced by Saal and Saal in 1996 with data suggesting:4,5
• Improved outcomes
• Significant reductions in VAS
• Less disability
• Enhance functionality
• Analgesic medication reduction
Numerous studies supported its use, and although promising, critics questioned the scientific validity of the study, noting nonrandomization, uncontrolled study design and potential observer bias.5–25 Mekhail and Kapural demonstrated a 78% decrease in VAS as well as significant improvement in activities of daily living in properly selected patients.20 Pauza et al performed a randomized, placebo controlled trial with a sham control arm.5 Forty percent of the treatment arm had at least 50% pain reduction, 21% experienced more than 80% pain reduction. The authors concluded that IDET was a viable therapy for an intractable discogenic pain.6 However, the technique has fallen out of favor due to a lack of reproducible outcomes, which is probably due to a poor patient selection, as well as inadequate and inconsistent reimbursement by third party payers. Although challenges remain, IDET is a viable therapy for selected patients.
ANATOMY AND PATHOGENESIS
• The intervertebral disc is composed of the nucleus pulposus (NP) encased by the annulus fibrosis (AF), sandwiched between the vertebral endplates.
• The disc is bound posterolaterally by the facet joints, anteriorly by the anterior longitudinal ligament (ALL), and posteriorly by the posterior longitudinal ligament (PLL).
• The NP is composed of proteoglycans, collagen, and water.
• The AF composed of concentric fibrocartilaginous fibers running obliquely and inserting into the vertebral end plates via the Sharpley fibers, with more reinforcement anteriorly.
• There is no direct vasculature to the intervertebral, and consequently, diffusion of nutrients is required.
• The segmental radicular arteries, entering near the anterior-cephalad portion of the neuroforamina, supplies the vertebra body and indirectly the disc.
The nerve supply of the disc is complex, as the sinuvertebral nerves (via the Luschka nerves) provide posterior coverage, while branches of the lumbar ventral rami, along with the gray ramus communicans, innervate ventral annulus as four separate ramus communicans nerves innervate each disc. Pain receptors have been identified in the outer third of the AP, the PLL, periosteum, paraspinal musculature, ligaments, and facet joints, as shown in Figure 35-1.
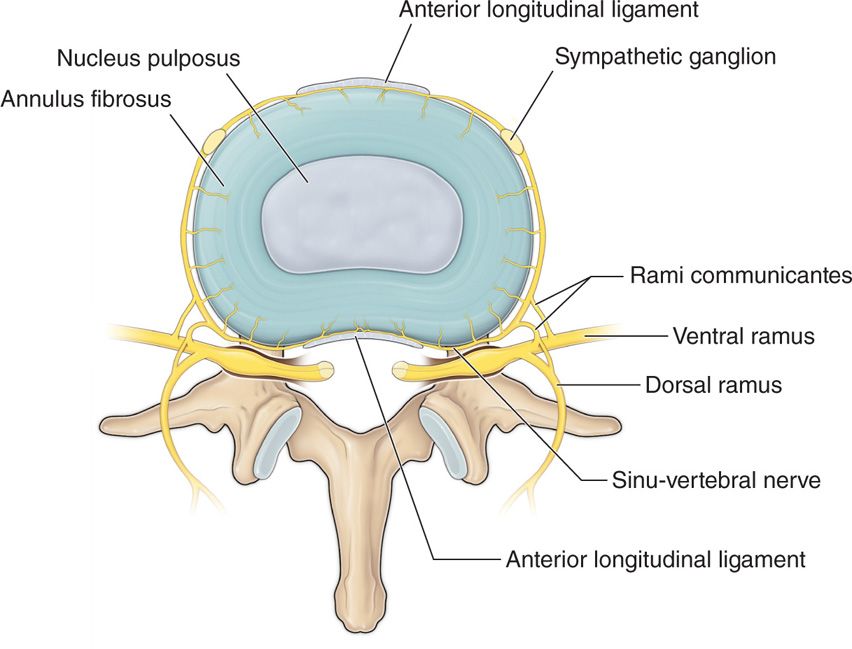
Figure 35-1. Anatomy and innervation of the intervertebral disc.
The pathogenesis of discogenic pain is multifactorial. It can be a result of mechanical or chemical irritation of the aforementioned nerves secondary to an internal disc disruption (IDD).
IDD is defined as:
• A disruption of the NP
• Commonly by fissures extending to the AF
• Creating chronic inflammation
• Neovascularization
• Neoinnervation of nociceptive origin, specifically A delta and C fibers, with a graded system of increasing severity, as shown in Figure 35-2.
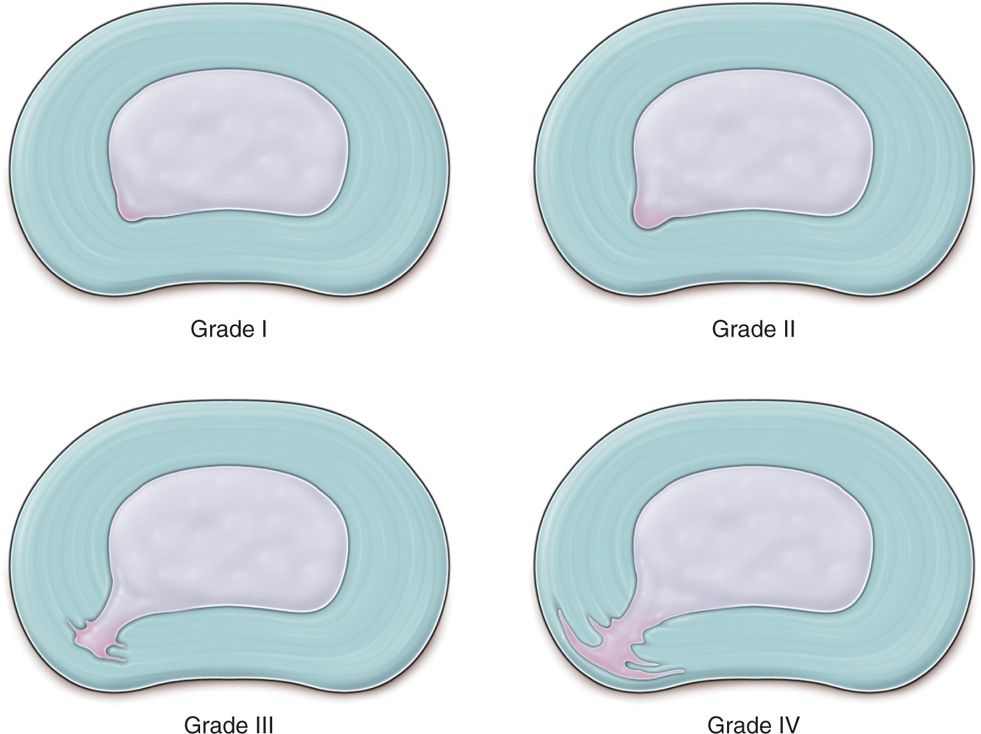
Figure 35-2. Dallas discogram scale grades of annular tissues.
Indications
• Discogenic pain secondary to internal disc disruption.
• Positive provocative discogram with concordant pain.
• Presence of high intensity zone on MRI suggestive of symptomatic disc.
• Pain should be of >3 months duration.
• Failed conservative measures, including medications and physical therapy.
• Less invasive causes ruled out (facetogenic or sacroiliac pain).
• MRI, x-ray, and reliable discogram should be within 1 year of proposed IDET procedure.
Detailed history and physical examination in patients with nonspecific back pain yields proper diagnosis in 30% of cases. Assimilation of the history, physical examination, and radiographic investigation including provocation tests, along with a skeptical suspicion, commonly yields an appropriate diagnosis. Patients typically have sitting intolerance and pain improves with recumbence. Straight leg raise is negative for radicular pain. The presence of high intensity zone (HIZ) on MRI may be suggestive of a symptomatic disc, although false positives have been reported to be near 15%.4 The gold standard for diagnosis is a provocative, concordant pain producing, appropriately performed discogram with mamometry, with two control levels spanning the suspected culprit painful disc. Discogram results amenable to discogenic procedures can be described as absolute, highly probable, or discogenic pain, based on IASP (International Association for the Study of Pain) and ISIS (International Spine Intervention Society) guideline statements. Briefly, the components of the discogram include concordant pain with a magnitude of at least 7 on a 0 to 10 scale, pressure testing, and presence of asymptomatic adjacent levels. Please refer to Table 35-1.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






