Infections
Aymarah M. Robles MD
Linda S. Efferen MD, FACP, FCCP
LOWER RESPIRATORY TRACT INFECTIONS
Aymarah M. Robles MD
Bacterial and viral lower respiratory tract infections are categorized into four groups:
Acute bronchitis, an acute inflammation of the tracheobronchial tree, is diagnosed by exclusion. Clinically it is characterized by the presence of either a productive or nonproductive cough of 4 to 6 weeks’ duration. Chronic bronchitis is part of the spectrum of chronic obstructive pulmonary disease (see Chap. 74).
Bronchiectasis is the permanent dilatation and subsequent destruction of subsegmental bronchi or bronchioles.
Lung abscess is the parenchymal destruction caused by an indolent suppurative process.
Pneumonia is an infection of the distal portion of the lungs, involving the respiratory bronchioles, alveolar ducts, sacs, and alveoli.
Primary care providers frequently evaluate patients with cough, which is the single most common symptom of respiratory illness. All segments of the population will at one time or another be faced with a respiratory infection. Familiarity with the categories of lower respiratory infection and their management is crucial to providing good primary care.
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
The trachea and bronchi are made of a rich epithelial cell surface composed of ciliated cells, secretory goblet cells, subepithelial cells (containing cartilage for structural support of the airways), and inflammatory mediator cells and glands. The amount of cartilage decreases as the respiratory tree branches distally and disappears altogether in the small airways (<2 mm in diameter). Tracheobronchial glands, which secrete mucus, are bigger and more numerous in the proximal airways.
Cells dedicated to airway defense are found scattered within the epithelium and submucosa. Lymphocytes may appear singly or in clusters, especially at branching points or airway bifurcations, and are called bronchus-associated lymphoid tissue. Plasma cells, especially IgA, mast cells, and macrophages, are also found at airway bifurcations. Mast cells increase in the transition zone leading to the distal airway, where gas conduction occurs. Marked branching of the airways continues as surface area is maximized for gas exchange. This architecture helps to keep the area below the main carina sterile.
The lower respiratory tract is uniquely equipped to protect against invading organisms. Aspiration of upper airway flora is the most important risk for infection. Defense mechanisms include a good cough reflex, effective mucociliary clearance (continual upward beating of cilia) to remove bacteria and debris, and angulation of airways, which traps and impinges bacteria at bifurcations. For infection to occur, the following sequential steps are required, especially at oropharyngeal colonization; aspiration of organisms; bacterial attachment to epithelial cell surfaces, preventing normal epithelial cell desquamation; and subsequent removal by expectoration.
The risk of lower airway infection is further increased by both the type of oral microflora present in the airways and host susceptibility. Severely ill patients lose their normal flora and become increasingly susceptible to enteric gram-negative bacilli. Clearance mechanisms progressively malfunction and are associated with abnormalities in mucosal surfaces. A recent viral infection may effectively strip the normal mucosa, causing intense cellular desquamation and loss of mucociliary function and local phagocytic function.
Within the terminal airway, the alveolar macrophage is the primary cellular defense. Alveolar macrophages are capable of overwhelming a challenge of low virulence—for instance, a normal, nocturnal, small-volume aspiration of oropharyngeal secretions. Activated alveolar macrophages also are capable of activating the immune system by recruiting polymorphonuclear leukocytes, found in pulmonary microvasculature reserves.
In addition, alveolar macrophages secrete cytokines, which trigger the intercellular communication systems of the immunologic response. Important lung cytokines include tumor necrosis factor, interleukin 1, and interleukin 8. They are produced in response to alveolar macrophages that activate mononuclear cells to release gamma colony stimulating factor (G-CSF). G-CSF increases myeloid progenitor cells, which trigger polymorphonuclear leukocytes to promote adhesion, chemotaxis, phagocytosis, and phosphorylation at local sites to combat infection.
EPIDEMIOLOGY
Pneumonia ranks as the sixth leading cause of death in the United States and is the leading cause of death attributable to an infectious disease. Current estimates for the United States are 4 million cases annually, with a morbidity rate of 12 per 1000 adults per year. Hospitalizations approach 600,000 per year, at an annual cost of $23 billion (MMWR, 1995a, b).
All humans are susceptible to lower respiratory tract infections. Symptoms of acute bronchitis in a previously healthy person implicate common cold viruses: rhinovirus, respiratory syncytial virus, parainfluenza, coronavirus, or adenovirus. Influenza
A or B may also be a cause. Nonviral agents include Mycoplasma pneumoniae, Chlamydia pneumoniae (originally described as TWAR), and Bordetella pertussis, an increasingly common pathogen in susceptible adults with persistent cough.
A or B may also be a cause. Nonviral agents include Mycoplasma pneumoniae, Chlamydia pneumoniae (originally described as TWAR), and Bordetella pertussis, an increasingly common pathogen in susceptible adults with persistent cough.
Patients with comorbid medical problems, underlying cardiorespiratory illness, immunocompromised status, or impaired cough reflex are at higher risk for infection with the usual respiratory flora and pathogenic bacteria such as Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus, Moraxella catarrhalis, and Legionella.
Chronic bronchitis is more common in tobacco users and those exposed to passive smoke. Inhaled irritants in tobacco smoke may decrease ciliary mucosal transport and decrease the phagocytic function of the pulmonary immunologic response. These increase the risk for both colonization and infection, especially by S. pneumoniae, H. influenzae, and M. catarrhalis.
Primary bronchiectasis is associated with multiple insults to the lung and is divided into the following main categories:
Postinfectious, occurring predominantly in infants and young children or occasionally in adults after upper lobe tuberculous or fungal infection
Bronchiectasis after aspiration of upper airway flora or gastric contents as a result of impaired consciousness (ie, seizure disorders), neuromuscular disorders, esophageal motility disorders, or general anesthesia or after alcohol or illicit drug use
Occupational hazards may also predispose to bronchiectasis—for example, inhalation of toxic gases (ammonia, nitrogen or sulfur oxides, and hydrocarbons)
Foreign body aspiration (eg, nails, tacks, beads, berries, seeds, coins), causing distal obstruction and subsequently leading to bronchiectasis
Mineral-based oil preparations, such as camphorated oil, are sometimes used inside the nostrils to relieve nasal congestion. The oil may be aspirated, leading to destruction and dilatation of the bronchi.
Anatomic abnormalities in the airway predispose to bronchiectasis.
Secondary bronchiectasis is associated with inherited or congenital diseases. Cystic fibrosis is the most common; others include immunoglobulin deficiencies and ciliary dyskinetic syndromes.
Predisposing epidemiologic factors leading to lung abscess include events related to impaired consciousness or sensorium, as well as esophageal motility disorders, history of seizures, or the use of alcohol or illicit drugs. These become even more significant in the presence of poor oral hygiene or gingivitis. Anaerobes account for 80% to 90% of all pulmonary suppurative lung abscesses. This is not surprising, given that inflamed gingival surfaces and crevices harbor a large volume of anaerobes (as high as 1012 organisms/g).
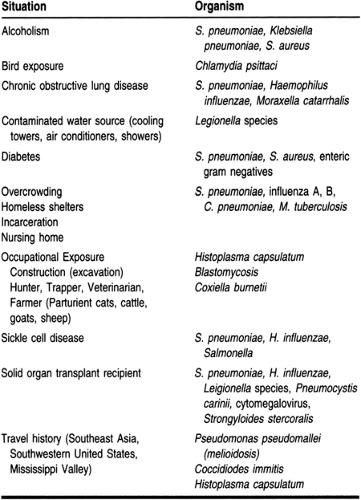
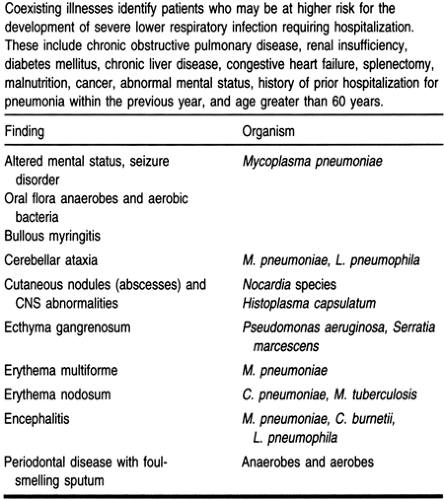
Evaluation of the epidemiologic setting and the physical exam can yield clues suggesting the most likely pathogen causing pneumonia (Tables 75-1 and 75-2).
DIAGNOSTIC CRITERIA
The diagnosis of both acute and chronic bronchis is based on a constellation of clinical symptoms and findings.
Patients with bronchiectasis present with a prolonged history of recurrent sinopulmonary infections and chronic cough productive of copious amounts of purulent sputum intermittently streaked with blood. The chest radiograph shows hyperlucent cystic areas and peribronchial fibrosis demonstrated by “tram tracks,” clearly delineated vertical or parallel lines of a descending bronchus. Thin-section chest computed tomography confirms the diagnosis. When contrast is administered, the so-called “signet ring” sign is seen, showing the diameter of the involved bronchus larger than its accompanying pulmonary artery.
The chest film in lung abscess reveals single or multiple thick-walled cavitary lesions with air-fluid levels. These lesions are generally located at dependent areas of the lungs, especially the superior segments of the lower lobes. Microbiologic diagnosis can be made by Gram stain and culture of sputum specimens.
The clinical spectrum in pneumonia varies, depending on whether the infection is community-acquired. Typical pneumonia presents with fever, productive cough, pleuritic chest pain, and clinical signs of consolidation. In atypical pneumonia, systemic symptoms predominate (eg, fever, headache, myalgias, dry or minimally productive cough, and lack of clinical signs of consolidation).
The chest radiograph demonstrating an infiltrate is the gold standard for the diagnosis of pneumonia. Radiographic abnormalities cannot distinguish bacterial from atypical pneumonia. Chest films can, however, help assess the extent and severity of illness; evaluate complications such as atelectasis, pleural effusion, or multilobar involvement; and assist in planning further diagnostic studies. Difficulties may arise in the interpretation of pneumonia in the presence of coexistent lung diseases or congestive heart failure, as well as in patients who cannot participate in taking standard posteroanterior/lateral films. Suboptimal films must be evaluated within the context of both the clinical presentation and findings. A repeat chest x-ray for diagnostic accuracy may be necessary once the patient can fully participate.
The etiologic diagnosis of pneumonia is based on microbiologic criteria. A definitive diagnosis is made when a pathogenic organism is recovered from a normally sterile site, i.e. blood or pleural fluid, or when an organism that is not a known colonizer is found in respiratory secretions, for example: viral organisms Influenza A or B; respiratory syncytial virus (RSV); herpesvirus (HSV); cytomegalovirus (CMV); Pneumocystis carinii Pneumonia (PCP); any fungi; Legionella; Mycoplasma pneumoniae; Chlamydia pneumoniae (TWAR); Bordetella pertussis; acid fast bacilli: Mycobacterium tuberculosis (MYB) or any atypical pathogenic acid fast bacillus.
Sputum Gram stains are an important diagnostic tool, provided that they are collected appropriately. The specimen must be collected before the initiation of antimicrobial therapy and must contain greater than 25 polymorphonuclear leukocytes and less than 10 epithelial cells per high-power field, demonstrating a true distal airway specimen not contaminated by saliva.
Failure to detect gram-positive clusters or gram-negative bacilli in the initial specimen virtually excludes these organisms from diagnostic consideration. In addition, the Gram stain may allow the detection of penicillin-resistant strains of S. pneumoniae. The inability to identify a predominant organism on Gram stain despite the presence of 25 polymorphonuclear leukocytes and less than 10 epithelial cells suggests the possibility of atypical pathogens, such as Legionella, Mycoplasma, Chlamydia, or a viral etiology or the use of antimicrobial therapy before obtaining the sputum for diagnostic studies.
HISTORY AND PHYSICAL EXAM
In acute bronchitis, a complete history should be taken, with careful attention to epidemiologic considerations (eg, occupation, recent community outbreak of influenza, overcrowded living conditions, a history of concurrent infections of close contacts). A thorough physical exam focused on the eyes, ears, nose, sinuses, throat, and cardiorespiratory system is crucial. Productive or nonproductive cough, together with retrosternal discomfort with or without wheezing, localizes symptoms to the lower airways. The physical exam is otherwise generally within normal limits. Fever is absent in most viral syndromes responsible for the common cold, most commonly rhinovirus, respiratory syncytial virus, or coronavirus. Fever is a component of influenza A and B, adenovirus, M. pneumoniae, C. pneumoniae, and B. pertussis infections. Lung auscultation reveals basilar rhonchi or rales that may change or clear with cough. Wheezing is also a nonspecific finding; it may persist long after other symptoms and signs have resolved.
Chronic bronchitis is present in cigarette smokers or persons exposed to chemical or environmental irritants, including passive smoke inhalation. There is a history of progressive exercise intolerance and episodic cough with increased expectoration of mucopurulent sputum. Prolonged recurrences may lead to arterial blood gas derangements, severe hypoxemia, and hypercarbia. In later stages this may lead to pulmonary artery hypertension and right-sided heart failure. The physical exam may reveal coughing and an increased respiratory rate associated with respiratory distress and abnormal breathing patterns. On auscultation, rhonchi and decreased air entry may be heard. Wheezing may be intermittent, especially if associated with acute mucus plugging of a bronchus. In later stages, if pulmonary hypertension ensues, a parasternal right ventricular heave and loud S2 may be noted. Lower extremity edema may be present if right-sided heart failure occurs.
Bronchiectasis produces copious mucopurulent, often blood-streaked sputum of many years’ duration and recurrent sinopulmonary infections. The physical exam reveals a chronically ill-appearing patient and possibly muscle wasting, malnutrition, and failure to thrive. Clubbing of the fingers from chronic hypoxemia may occur. On auscultation, coarse rales with variations in pitch and volume at both inspiration and expiration are often heard, as well as coarse rhonchi representing secretions in large airways.
Patients with lung abscess typically present with an insidious course of a 2- to 4-week duration of fever, purulent fetid blood-streaked sputum, generalized malaise, anorexia, and weight loss. Chest pain is common. On the physical exam, low-grade fever is present. The patient appears chronically ill and pale. The oral exam reveals poor dentition or gingivitis and overall poor dental hygiene. Signs of consolidation may be heard on auscultation, accompanied by amphoric or tubular breath sounds over the site of the lung abscess. When empyema invades the pleural space, pleuritic chest pain may be prominent, and dullness to percussion is encountered.
Symptoms suggestive of pneumonia are nonspecific and include fever, cough, sputum production, shortness of breath, and chest pain. The mean duration of illness before seeking medical attention is usually 5 to 6 days. Fever occurs in approximately 80% of patients. Another 30% have signs of consolidation with egophony. Most patients have at least one of these symptoms.
Those at highest risk for complications of pneumonia are persons with comorbid illness such as chronic obstructive pulmonary disease, congestive heart failure, immunosuppression (including chronic steroid use), diabetes mellitus, renal insufficiency, chronic liver disease, postsplenectomy, or chronic alcohol or illicit drug use and malnutrition, or those older than 60 years.
DIAGNOSTIC STUDIES
The definitive laboratory diagnosis of an upper respiratory viral infection causing acute bronchitis is unnecessary. Chest x-rays should be obtained in all patients who appear ill to exclude a more serious lower respiratory infection.
Chronic bronchitis is also diagnosed primarily on symptoms. Recurrent episodes of clinical deterioration can occur, especially when complicated by upper respiratory infection and fever or increased volume or purulence of sputum. Patients may appear cyanotic and the arterial blood gas analysis may reveal hypoxemia and hypercapnea. Repeated recurrences may lead to permanent blood gas derangements and chronic ventilatory failure characterized by well-compensated respiratory acidosis. This is evidenced by elevated serum bicarbonate levels, confirming renal compensation for the chronic hypercarbia. Erythrocytosis and elevations of hemoglobin and hematocrit are seen on a routine complete blood count as evidence of the compensatory response to chronic hypoxemia. Leukocytosis may be a feature of bacterial infection. An appropriately collected and rapidly processed Gram stain of the sputum with culture will identify the primary bacterial pathogen, or a superinfection after an episode of viral, mycoplasmal, or chlamydial infection. The usual bacterial pathogens include S. pneumoniae, H. influenzae, and M. catarrhalis. Enteric gram-negative organisms, especially Klebsiella and Pseudomonas, should also be excluded. Electrocardiography may show supraventricular arrhythmias, intraventricular conduction defects, right ventricular strain, right ventricular hypertrophy, right bundle branch block, and morphologic P-wave abnormalities, all related to hypoxemia. Chest radiography is nonspecific and may suggest hyperinflation, bronchial prominence, or other signs of dilatation. If pulmonary hypertension is present, enlarged pulmonary arteries may be seen. In cor pulmonale, an enlarged right ventricle may be seen on chest films. Spirometry indicates signs of airflow obstruction with a decrease in forced expiratory volume in 1 sec (FEV1) and in the ratio of FEV1 to forced vital capacity.
In bronchiectasis, hypercarbia with ensuing chronic ventilatory failure is seen in late-stage disease. Additional diagnostic options are tailored to the patient. When an appropriate clinical or family history suggests cystic fibrosis as the etiology for bronchiectasis, a sweat chloride determination with pilocarpine iontophoresis should be performed. Serum protein electrophoresis and IgG subsets may be obtained to evaluate for immunologic abnormalities. If fever and recurrent wheezing are present and central bronchiectasis is found on the chest radiograph, an evaluation for allergic bronchopulmonary aspergillosis should be performed. Sputum Gram stain and culture will identify bacterial pathogens.
Bronchoscopy, percutaneous transthoracic needle aspiration, or diagnostic thoracentesis of pleural fluid have replaced transtracheal aspiration for the diagnosis of a lung abscess. In addition to examining the aspirate, blood cultures are essential. Anemia of chronic disease is usually present. When other conditions coexist, such as alcoholism or malnutrition, an iron or folate deficiency anemia may also be present. A moderate leukocytosis is often found. A computed tomography scan of the chest is often performed to evaluate the parenchyma and distinguish pleural involvement. Additional studies should be tailored to the patient and are used primarily in rapidly worsening disease.
The etiologic diagnosis of pneumonia is based on microbiologic criteria. Accurate identification of a pathogen necessitates that it be present in a normally sterile site, i.e., blood or pleural fluid, and that it not be a known colonizer in respiratory secretions. The most common pathogens for pneumonia include: any fungi, Histoplasma capsulatum, Coccidiodes immitis, Blastomyces dermatitis, Pneumocystis carinii pneumonia (PCP); parasites: Toxoplasma gondii, strongyloides; viral organisms such as Influenza A or B, respiratory syncytial virus (RSV), Herpesvirus (HSV); Legionella, Mycoplasma pneumoniae, Chlamydia pneumoniae (TWAR), and Bordetella pertussis.
In summary, all patients with an increased risk for morbidity or mortality from pneumonia require hospitalization and careful observation. Required studies include chest radiography; arterial blood gas analysis; complete blood count; chemistry profile, including electrolytes and renal and liver function tests; and microbiologic studies (blood cultures, Gram stain and culture of sputum), with additional special studies such as staining and culture for acid-fast bacilli. When Legionella is suspected, sputum for both culture and direct fluorescent antibody test (DFA), should be obtained. In addition, a urine sample for Legionella pneumonia serogroup 1 radioimmune assay is 80% to 99% sensitive and 99% specific.
Pleural fluid, if present, requires early, aggressive diagnostic thoracentesis and pleural fluid analysis with cell count and differential; pH collected anaerobically and on ice, chemistries, including: glucose, protein, and lactate dehydrogenase; Gram stain and bacterial culture; acid-fast stain; mycobacterial and fungal cultures; and cytology.
TREATMENT OPTIONS, EXPECTED OUTCOMES, AND COMPREHENSIVE MANAGEMENT
Prevention
Annual immunizations with influenza vaccine for susceptible groups, as recommended by the Centers for Disease Control & Prevention, is mandatory to prevent life-threatening illness or death. The influenza vaccine also prevents the secondary development of bacterial pneumonia from S. pneumoniae, H. influenzae, and S. aureus in patients originally infected with influenza. Each year, the influenza vaccine is estimated to be 70% effective in preventing influenza-related pneumonia, hospital admissions, and death. Influenza vaccinations are also recommended for health care workers who care for susceptible patients.
Chemoprophylaxis with antiviral agents such as amantadine or rimantadine is also effective against influenza A when used at the initiation of symptoms.
Chemoprophylaxis with antiviral agents such as amantadine or rimantadine is also effective against influenza A when used at the initiation of symptoms.
The CDC also recommends vaccination with the polyvalent 23 antigen pneumococcal vaccine. This vaccine is 50% to 70% efficacious, especially against serotypes most likely to cause bacteremic pneumococcal infections. Titers should be checked periodically; if waning, repeat immunization is recommended every 5 to 7 years.
The avoidance of tobacco is crucial for respiratory and cardiac well-being. Good oral hygiene and the avoidance of habits leading to an altered state of consciousness (ie, alcohol and illicit drug use) are important to prevent aspiration syndromes that may lead to severe lower airway respiratory infections.
Age and Economic Considerations
Infection of the lower respiratory tract remains the leading cause of death in persons older than 65 years. As the population ages, the magnitude of this problem will become more acute. Pneumonia in the elderly is a serious clinical dilemma and diagnostic challenge. Atypical presentations with subtle latent symptoms and signs such as confusion, low-grade fever, anorexia, dehydration, mild tachypnea, and worsening of the patient’s underlying disease process may confound the clinical presentation and course. Rates of pneumococcal pneumonia in persons older than 65 years are three- to fivefold greater than in young adults and requires hospitalization in approximately 90% of patients.
Morbidity and mortality rates are often higher in persons without adequate medical insurance, who tend to seek assistance late in their course, or those who have no regular access to medical care and who utilize inner-city emergency departments for primary care. Malnourished patients are at increased risk because of the derangements in host defense systems that delay and impair the healing process.
Treatment Options, Expected Outcomes, and Comprehensive Management
Treatment for acute bronchitis is symptomatic: acetaminophen, oral liquids, and bed rest are encouraged when malaise and fever are prominent. Dextromethorphan (15 mg orally every 4 to 6 hours) will suppress a nonproductive cough. Inhaled selective beta-2 agonists (two puffs every 6 hours) may be prescribed when wheezing is present. Antibiotics should be reserved for specific instances where a nonviral etiology is suspected. A trial of oral erythromycin or the newer macrolide antibiotics is useful as first-line therapy for M. pneumoniae or C. pneumoniae.
Patients with chronic bronchitis should be encouraged to enter a program for smoking cessation. Airflow obstruction is best managed with inhaled ipratropium bromide, with or without inhaled selective beta-2 agonists. Oral theophylline, with careful attention to serum levels, may be considered in selected patients to enhance both diaphragmatic function and mucociliary clearance. The efficacy of inhaled or systemic steroids remains controversial, but they are often used in patients who remain symptomatic despite maximal and appropriate use of inhaled bronchodilator therapy.
Bacterial exacerbations require the use of antibiotic therapy, and a sputum Gram stain should guide the choice of antimicrobial therapy. Common antibiotics used to treat exacerbations include ampicillin, amoxicillin, amoxicillin–clavulanate, trimethoprim–sulfamethoxazole, quinolones, oral second- or third-generation cephalosporins, and erythromycin or other newer macrolides. Home oxygen therapy is required when baseline PaO2 is less than 55 mmHg. It should be used at least 18 hours per day to ameliorate pulmonary hypertension. Patients with known polycythemia, pulmonary hypertension, or cor pulmonale whose baseline PaO2 is 56 to 59 mmHg also require supplemental oxygen therapy. Chronic ventilatory failure may be treated by the use of nocturnal noninvasive continuous positive airway pressure.
Antimicrobial therapy of lung abscess is based on the microbiology. Penicillin is acceptable as initial therapy, although high intravenous doses (10 to 20 million U/day) are required. Oral metronidazole added to intravenous penicillin adds efficacy to the regimen (Hammond et al, 1995). In seriously ill patients, intravenous clindamycin is highly efficacious, and a rapid early clinical response is often seen. Once clinically improved, patients require a prolonged course of oral antibiotic therapy until complete resolution of the infiltrate and cavity has occurred. This may necessitate as much as 6 to 12 weeks of therapy.
Chest physiotherapy to promote abscess drainage is an adjunctive therapeutic measure. Bronchoscopic evaluation of the airways may be required to evaluate for foreign body aspiration. Rarely, surgical intervention is required, although it is often related to complications arising from cavity wall vessel erosion that produces massive hemoptysis.
Ideally, therapy for pneumonia should be directed at the causative pathogen. In more than 50% of cases, the etiology is unknown, and empiric, well-informed therapy decisions must be made. The therapy for community-acquired pneumonia is based on the patient’s age, the presence or lack of comorbid conditions, and the clinical severity at presentation. Eighty percent of those who develop pneumonia may be treated as outpatients. The most common organisms are S. pneumoniae, C. pneumoniae, M. pneumoniae, and respiratory viruses, especially influenza A or B and H. influenzae. Initial antimicrobial therapy with a macrolide antibiotic such as erythromycin, clarithromycin, or azithromycin is appropriate. An oral second-generation cephalosporin or trimethoprim–sulfamethoxazole or levofloxacin, the newer extended-spectrum quinolone, may also be used as first-line therapy. Tetracycline may be used if allergy or intolerance to other medications should occur.
Patients older than 60 years or those who have comorbidity are infected with the same organisms as the uncomplicated population. Aerobic gram-negative bacilli, S. aureus, M. catarrhalis, and Legionella also infect the high-risk group. Initial therapy should reflect the sputum Gram stain results or should empirically cover all the above organisms. Either a second-generation cephalosporin or trimethoprim–sulfamethoxazole or a combination beta-lactamase inhibitor is appropriate for first-line oral therapy. A macrolide antibiotic may be added if infection with Legionella is suspected.
Patients who require hospital admission may be infected with any organism, although S. pneumoniae, aerobic gram-negative bacilli, and Legionella are especially suspect. These pathogens account for a large percentage of severe cases of community-acquired pneumonia. Intravenous second- or third-generation
cephalosporins or a β-lactam-inhibitor and the addition of a macrolide is recommended as initial therapy. An alternative regimen combines intravenous therapy with a macrolide antibiotic to cover both Pneumococcus and Legionella and a third-generation cephalosporin with Pseudomonas activity, plus an aminoglycoside or another antipseudomonal antimicrobial, plus an aminoglycoside. All antimicrobial therapy requires re-evaluation and must be individualized once microbiologic confirmation and susceptibilities are available.
cephalosporins or a β-lactam-inhibitor and the addition of a macrolide is recommended as initial therapy. An alternative regimen combines intravenous therapy with a macrolide antibiotic to cover both Pneumococcus and Legionella and a third-generation cephalosporin with Pseudomonas activity, plus an aminoglycoside or another antipseudomonal antimicrobial, plus an aminoglycoside. All antimicrobial therapy requires re-evaluation and must be individualized once microbiologic confirmation and susceptibilities are available.
In severe pneumonia requiring hospitalization, mortality rates nearing 50% continue to be reported despite effective and appropriate antimicrobial therapy. The high fatality rates may be related to inadequate host defense mechanisms that lead to irreversible physiologic derangements.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree