CHAPTER 9
Infection: Prevention, Diagnosis, and Management
INTRODUCTION
Prevention of infection in patients undergoing interventional procedures remains a top priority of the interventional pain physician. Proper techniques and standard precautions must be strictly adhered to prevent infectious complications in patients receiving interventional procedures ranging from peripheral joint injections to the implantation of devices such as spinal cord stimulators and intrathecal medication delivery systems. Infectious complications include, but are not limited to, epidural, spinal, or subdural abscess; paravertebral, paraspinous, or psoas abscess; meningitis; encephalitis; sepsis; bacteremia; viremia; fungemia; osteomyelitis; local subcutaneous infection; hardware infections causing removal of expensive equipment; or discitis. The risk of infection may be reduced by identifying patients who are at increased risk for infection, adhering to the standard of care for reducing the risks, and considering prompt interventions to improve outcomes after infectious complications.
HISTORY AND PHYSICAL EXAMINATION
A focused history and physical examination of the patient receiving an interventional procedure or implantable device can be helpful in identifying patients at risk for developing infectious complications.
• Coexisting medical conditions can impair the immune system and increase the risks of infections such as cancer, chemotherapy, radiation, AIDS, and diabetes.
• Preexisting infection, pancreatitis, drug, or alcohol abuse may be associated with a higher incidence of infectious complications.
• Bacteremia and septicemia are contraindications; however, distal localized infection without any indication of systemic disease are not contraindications.
• Close postoperative follow-up and a high index of suspicion for infection in the high-risk patients.
• Review of current lab values such as CBC to assess for leukocytosis can be helpful, although routine preprocedure measurement is not recommended.
IMPACT OF SURGICAL SITE INFECTIONS
The procedures that involve implantable devices are done in the operating rooms and follow the strict intraoperative discipline to prevent the infection to reduce the financial burden.
• In United States, more than 40 million inpatient surgical procedures each year; 2% to 5% complicated by surgical site infections (SSIs).
• The infection rate varies from 3% to 6%.
• SSIs are second most common nosocomial infection (24% of all nosocomial infections).
• Infection is responsible for prolonged hospital stay by 7.4 days.
• It costs $400 to $2600 per infection depending on the surgical site and type of device.
• The cost of treatment of infection from neurosurgic implants to vascular shunts can be as high as 50,000 per case.
INFECTION WITH IMPLANTABLE DEVICES
• It varies from 2.5% (clean cases) to 9% (immunocompromised patients).
Most Common Organisms
• Staphylococcus aureus: coagulase positive
• Staphylococcus epidermidis: coagulase negative
• Methicillin-resistant S aureus (MRSA)
• Vancomycin-resistant enterococci (VRE)
• Vancomycin-resistant S aureus (VRSA)
• Multidrug-resistant organisms (MDRO)
MRSA Infection
• Usually staphylococci are sensitive to β-lactam antibiotics (ampicillin, methicillin, and cephalosporin).
• Two strains exist: Less-resistant community-acquired MRSA (CA-MRSA) and highly resistant hospital-acquired MRSA (HA-MRSA).
• It carries high risk of toxic shock syndrome due to exotoxins.
• Usually treated with vancomycin, linezolid, or teicoplanin.
Patients at High Risks for Contracting MRSA Infection
• Frequent hospitalization
• Inappropriate use of antibiotics
• Patients with type I or type II diabetes
What is a Coagulase Test?
It is a test to identify coagulase enzyme that is produced by pathogenic strains of staphylococci. It causes fibrin clots of blood plasma and eventually fibrin clot makes organism resistant to:
• Phagocytosis
• Host’s immune response
• Penetration of antimicrobial agents
Pathophysiology of Implant Infection
The process of infection creates a “biofilm” around the implant composed of fibrinogen, fibronectin, and collagen. This biofilm:
• Enhances bacterial adherence
• Promotes multiplication of pathogens
• Enhances toxin liberation
• Decreases penetration of antibiotics
Surgical site infection is defined according to the site and depth of infection to help understand the seriousness of the issue and formulate a treatment plan.
• Superficial infection: Infection of skin and subcutaneous tissue, suture, or incisional infection
• Deep infection: Involves deeper soft tissue or pocket infection
• Organ/space infection: Infection spreads deeper layers to involve specific structures, for example, meninges
Sources of Infection
Exogenous:
• Contamination by patient
• Surgical personnel
• Operating room environment
• Instruments
• Materials
Endogenous
• Blood borne
• Seeding from distant site
• Implant provides nidus for the infection
Patient-Related Risk Factors
Following risk factors should be taken into account while doing any interventional spinal procedures, especially important while performing surgical procedures for implantable devices.
• Obesity
• Infection at remote site
• Systemic steroid use
• Nicotine use
• Immunocompromised patient
• Diabetes
• Malnutrition
• Prolonged hospitalization
As placement of implantable devices like spinal cord stimulators and intrathecal drug delivery reservoirs has become common practice by interventional pain physicians, it is of paramount importance to understand the intraoperative discipline to maintain sterility. Many implanters may not have formal surgical training, and need to be scrupulous and attentive to details required to maintain sterile condition. As our interventions are directly connected to spinal cord and central nervous system, an infection in this setting can lead to significant complications. The surgical risk factors include:
• Inappropriate use and/or lack of antimicrobial prophylaxis
• Poor surgical technique
• Longer duration of surgery
Prevention of Infection
The practice of aseptic techniques should be closely monitored and strictly adhered to without looking for any shortcuts when performing interventional procedures or surgery. Three target areas should be closely monitored. They are:
1. Preoperative or preprocedural considerations 1.
2. Intraoperative discipline 2.
3. Postoperative or postprocedural course 3.
Preprocedural or preoperative considerations:
• Routine interventions generally do not require antibiotic prophylaxis.
• Strict sugar control is recommended for diabetic patients.
• Wear appropriate surgical attire including scrub suits, masks, and caps; remove jewelry.
• For surgical procedures of implantable devices, the aseptic technique should include complete surgical scrub and gowning.
• Every steps of proper prepping and draping should be followed.
• Use either chlorhexadine with alcohol or an alcohol combined with povidone-iodine solution for hand scrubbing and skin antisepsis prior to performing procedures and injections.
Avagard Pump (Figure 9-1)
• The active ingredients of Avagard are 1% chlorhexidine gluconate in 61% ethyl alcohol.
• It is waterless, scrub-less, and brush-free hand antiseptic.
• It provides rapid antisepsis against broad spectrum of organisms without disrupting natural barrier of skin.

Figure 9-1. Avagard pump.
Prophylactic Antibiotics
Antimicrobial prophylaxis has been one of the most important advancements in reducing SSIs. Most SSIs are associated with skin microorganisms, especially the patient’s own bacteria. The decision to administer prophylactic antibiotics depends largely on the nature of the procedure being performed. In general, antibiotic prophylaxis is not indicated for neuraxial techniques such as epidurals, facet blocks, and medial branch blocks; radiofrequency ablation; peripheral joint injections; and nerve blocks and sympathetic blocks.
Provocative Discography
Discitis is a known and feared complication of provocative discography. It is recommended that some form of antibiotic be given prior to discography. A standard practice is to administer 1 g of an intravenous cephalosporin prior to the procedure. Staphylococcus epidermidis is the pathogen most likely to be responsible for discitis.1 To overcome this incomplete intradiscal penetrance, some believe to administer intradiscally in addition to intravenous antibiotics. In the case of cephalosporin allergy, clindamycin can be substituted.
Vertebral Augmentation
Infection involving the implanted polymethyl methacrylate (PMMA) in the spine is a disastrous complication. Common antibiotic prophylaxis practice measures include antibiotics to the PMMA mixture, giving preoperative IV antibiotics, both, or neither. The role of antibiotic prophylaxis in vertebral augmentation is not uniformly agreed upon. If the patient is debilitated or immunocompromised, antibiotic prophylaxis is recommended.
Implantable Devices
Infection remains the number one cause of nonequipment-related complication in SCS and reservoir implantation. Antimicrobial prophylaxis has been one of the most important advances in the reduction of SSIs.
• Routine antibiotic prophylaxis are warranted in all patients with implantable devices. (Evidence level I-a, Recommended grade A.)
• Antibiotic prophylaxis is associated with a 5-fold decrease in SSI rates.
• It decreases the bacterial infection–related mortality if used in neutropenic patients.
• Timing of antibiotics should be less than 2 hours, preferably within 30 minutes of incision.
• Cefazoline 1-2 g IV 30 minutes before incision.
• Clindamycin 600 mg IV in patients with β-lactam allergy.
• Vancomycin 1 g IV over 60 minutes for patients who are carriers of MRSA.
Though the use of antibiotics has drastically reduced postoperative infection rate, it is also of paramount importance to understand that improper use of antibiotics is not without potential risks.
• Hypersensitivity reaction: Ranging from skin rashes to anaphylactic shock
• Superinfection: Alteration of normal bacterial flora and overgrowth of opportunistic organisms, for example, fungi
• Emergence of resistant strain due to intermittent colonization as a result of overuse of antibiotics
Pseudomembranous colitis is a serious medical emergency condition that can occur secondary to overuse of antibiotics, mainly clindamycin.
• It promotes overgrowth of organism C defficile.
• It can occur with ampicillin, amoxicillin, ciprofloxacin, bactrim, and cephalosporins.
• It is a medical emergency and should be promptly treated as following:
1. Stop antibiotics.
2. Correct dehydration
and electrolyte imbalance.
3. Give flagyl and vancomycin orally for 10 days.
Prepping and Draping for Implant Placement (Figures 9-2 to 9-7):

Figure 9-2. Isolate the surgical area with plastic drapes.

Figure 9-3. Prep the area with betidine gel or chloropre. Prepare surgical site by antiseptic solution in “concentric” manner from incision site to periphery.
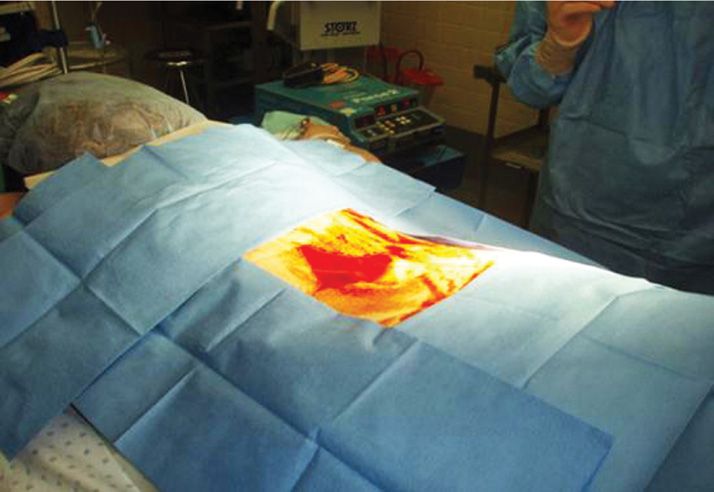
Figure 9-4. Isolate the prepped area with blue sticky sterile towels.
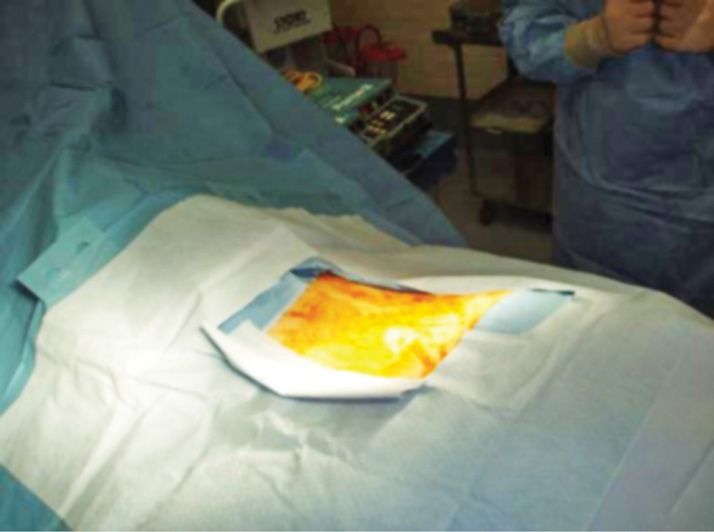
Figure 9-5. Full surgical drape placed.
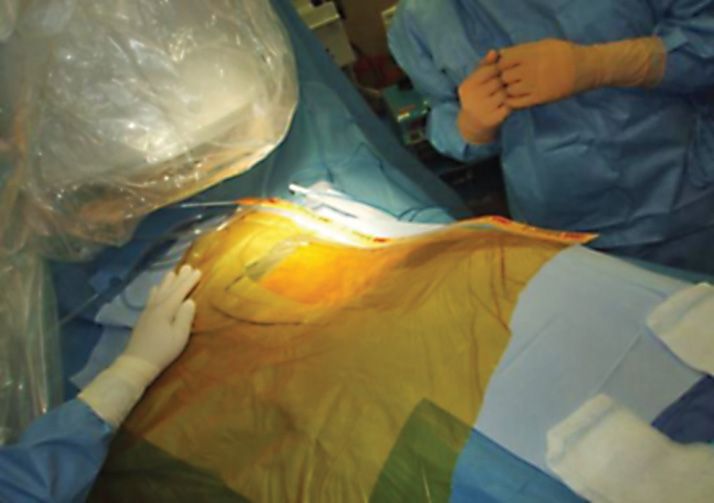
Figure 9-6. Place antimicrobial surgical drapes with an iodophor impregnated adhesive, which is designed to provide a sterile surface all the way to the wound edge and continuous antimicrobial activity throughout the procedure.

Figure 9-7. Don’t forget to drape the fluoroscope!
Intraoperative Considerations for Implantable Devices
Use double gloves, larger size in and smaller out. Select device or model suitable for patient’s size and habitus. Consider surgical scars, ostomies, waistline, and clothing in selection of pocket site for the device. Avoid placing device directly under suture line and consider subfascial placement in underweight patients.
• Remove devitalized tissue from the surgical wounds.
• Maintain adequate hemostasis.
• Consider gentle handling tissues to minimize surgical trauma.
• Eradicate dead space to reduce fluid collection and subsequent infection.
• Irrigate the wound with antibiotic solution to remove debris, foreign materials, and blood clots and to decrease contamination and infection.
• Close the incision in anatomical layers.
• Apply bio-occlusive, antiseptic wound dressing.
Postoperative Course
It is of paramount importance to closely monitor the wound for postoperative complications like bleeding and infection.
• Keep dressing dry and clean.
• Monitor for localized redness and tenderness.
• Monitor WBC, fever, and neurologic deficit.
• The dressing change must be with aseptic technique.
• No need to continue antibiotic unless warranted.
• Treat threatened incision aggressively.
Intrathecal Versus Epidural Infection
Due to direct connection of SCS leads and intrathecal catheter to the neuraxial structures, the disastrous complications with unfavorable outcome is a strong possibility.
• Epidural infection usually produces “space”-occupying lesion and creates pressure over dorsal surface of spinal cord eventually causing kink of anterior spinal artery and subsequent ischemia of two-thirds of spinal cord and motor deficit. Symptoms vary from sensory deficit to motor paralysis.
• Depending on the extent of injury and the time spent after first indication of infection, the outcome is usually unfavorable. Epidural infection may be treated with IV antibiotics, but abscess will need emergency surgical decompression. Neurologic functions usually recover completely if surgery is performed within 24 hours of first neurologic deficit. Partial recovery if decompression is done within 24 to 36 hours and “no” recovery after 36 hours.
• Intrathecal infection produces signs and symptoms of meningeal irritation, for example, stiff neck, photophobia, and headache. Patient may also show cerebral signs due to bacterial encephalitis, for example, irritability, lethargy, and mental status changes.
• Both conditions usually present with fever, increased WBC, increased ESR, and increased C-reactive protein (CRP) in CSF.
• Diagnosis is confirmed by imaging studies and positive CSF culture.
Diagnosis and Treatment of Infection
Proper screening, history and physical examination, sterile technique, and proper use of prophylactic antibiotics do not ensure 100% prevention of infectious complications. Close monitoring, high degree of suspicion, and early diagnosis are extremely important to prevent infectious complications and potential devastating sequela. Each patient is at risk for each procedure, and every patient should be closely monitored post procedurally for signs and symptoms of infection. Lack of external localized tenderness and erythema does not ensure neuraxial infection. Early indications to increase index of suspicion of infection include:
• Spiking temperature
• Increasing backache
• Headache
• Localized erythema and tenderness at the insertion site
• Changes in sensory and motor function should increase the index of suspicion for infection
More ominous signs include:
• Stiff neck
• Photophobia
• Changing mental status and confusion
• Increasing radiating pain
• Increasing motor deficit; in addition, specific attention should be focused on the neurologic examination
Laboratory Tests and Imaging
If signs and symptoms lead to suspicion of infection, laboratory and imaging studies can be used to confirm the diagnosis. Laboratory studies such as:
• Leukocyte count
• Erythrocyte sedimentation rate (ESR)
• C-reactive protein (CRP)
It should be noted that these studies are nonspecific and can be elevated in patients without infection. If the suspicion of infection is high and associated with neurologic signs, CT scan or MRI, with and without contrast should be obtained promptly to confirm the diagnosis.
Management of Infection
When the diagnosis of infection is suspected and confirmed, prompt treatment must be initiated. Proper treatment usually involves initiating appropriate antibiotic therapy, consultation with a physician specializing in the diagnosis, and treatment of infectious diseases should be considered.
Superficial infection is a salvageable condition and if the treatment started promptly.
• Individualize the treatment plan depending on the extent of infection.
• Involve Infectious Disease MD to appropriately manage infection.
• Obvious fluid/pus collection should be drained.
• Obtain culture and sensitivity (C&S) status of the wound discharge.
• Oral and/or parenteral antibiotics should be administered as per the C&S.
• Closely monitor WBC, fever, and neurologic examination.
In case of deep and neuraxial infection, it is critical to take appropriate and adequate steps to avoid disastrous outcome. If there is any evidence of deep organ infection, for example, meningitis, erythema, induration, or tenderness along the course of catheter
• Plan to explants the device as soon as possible.
• Hold antibiotics until specimen for culture and sensitivity is obtained from the wound.
• Remove the entire implant system including anchors.
• Postoperatively, leave the implant wound open or provide drain if you close.
• Provide proper postoperative wound care and aseptic dressing change.
• Place peripherally inserted central catheter (PICC) line and antibiotics as per infectious disease recommendations (4 weeks).
• Obtain negative surveillance cultures of blood and CSF before 2nd stage reimplantation surgery is planned.
Additionally, if epidural abscess is suspected, surgical evaluation should be obtained on whether to perform percutaneous drainage or laminectomy. It should be noted that treating a surgical site infection without removing the device poses high risk of deeper migration as SCS leads and intrathecal catheter form a conduit to the epidural or intrathecal space and can lead to epidural abscess or meningitis.
Wound Seroma
It is a small collection of aseptic fluid at the suture line or around the implant and is not an infrequent occurrence.
• It is a collection of sterile serosanguinous fluid in the pocket.
• Small amount usually spontaneously resolves.
• Abdominal binder may help reduce the primary collection and recollection after aspiration.
• Avoid repeated aspiration as it is a potential cause for infection.
• If aspiration is indicated for larger collections, culture the aspirate to rule out infection.
• Bacterial growth is confirmation of infection of the wound.
Postprocedural discitis is a rare complication after-intradiscal procedures. It is imperative for the treating physician to maintain a high index of suspicion. Appropriate laboratory and imaging studies are invaluable in establishing a timely diagnosis. In the majority of patients, antibiotic treatment along with spinal immobilization has been shown to produce good long-term outcomes. Operative intervention is rarely necessary in patients failing conservative treatment.
CONCLUSION
Interventional pain management specialists perform a variety of techniques ranging from neuraxial injections, neuroablative procedures, diagnostic and therapeutic intradiscal procedures, and the implantation of spinal cord stimulators and intrathecal pumps. Core knowledge of the risks of infections for each technique in every patient and systematic approach to prevention, diagnosis, and management of these complications is extremely vital.
• Appropriate prophylactic antibiotics as and where indicated.
• Strict sugar control in diabetic patients.
• Strict intraoperative discipline.
• Employ proper surgical techniques and provide adequate hemostasis.
• Intraoperative antibiotic irrigation is important to clean devitalized tissue before closure.
• Provide close postprocedural and postoperative monitoring of surgical site.
• Keep high index of suspicion and provide individualized treatment plan for infections.
• Ask for help from infectious disease (ID) experts sooner than later.
• Understand the resistant microorganism.
• Avoid improper and overuse of antibiotics.
Develop a surgical conscience that allows for no compromise in the principles of aseptic techniques, since anything less could increase the potential risk of infection, resulting in harm to the patient. As a physician proving care to our patients, we have greater responsibility of monitoring and maintaining aseptic environment during periprocedural and perioperative period, thus preventing harm to our patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






