Key Concepts
 Clinical trials have shown that inhaled nitric oxide is a selective pulmonary vasodilator that is beneficial in the treatment of reversible pulmonary hypertension. By improving perfusion only in ventilated areas of the lung, inhaled nitric oxide may improve oxygenation in patients with acute respiratory distress syndrome or during one-lung ventilation.
Clinical trials have shown that inhaled nitric oxide is a selective pulmonary vasodilator that is beneficial in the treatment of reversible pulmonary hypertension. By improving perfusion only in ventilated areas of the lung, inhaled nitric oxide may improve oxygenation in patients with acute respiratory distress syndrome or during one-lung ventilation.
 Acute cyanide toxicity is characterized by metabolic acidosis, cardiac arrhythmias, and increased venous oxygen content (as a result of the inability to utilize oxygen). Another early sign of cyanide toxicity is the acute resistance to the hypotensive effects of increasing doses of sodium nitroprusside (tachyphylaxis).
Acute cyanide toxicity is characterized by metabolic acidosis, cardiac arrhythmias, and increased venous oxygen content (as a result of the inability to utilize oxygen). Another early sign of cyanide toxicity is the acute resistance to the hypotensive effects of increasing doses of sodium nitroprusside (tachyphylaxis).
 By dilating pulmonary vessels, sodium nitroprusside may prevent the normal vasoconstrictive response of the pulmonary vasculature to hypoxia (hypoxic pulmonary vasoconstriction).
By dilating pulmonary vessels, sodium nitroprusside may prevent the normal vasoconstrictive response of the pulmonary vasculature to hypoxia (hypoxic pulmonary vasoconstriction).
 Preload reduction makes nitroglycerin an excellent drug for the relief of cardiogenic pulmonary edema.
Preload reduction makes nitroglycerin an excellent drug for the relief of cardiogenic pulmonary edema.
 Hydralazine relaxes arteriolar smooth muscle, causing dilatation of precapillary resistance vessels via increased cyclic guanosine 3’,5’-monophosphate.
Hydralazine relaxes arteriolar smooth muscle, causing dilatation of precapillary resistance vessels via increased cyclic guanosine 3’,5’-monophosphate.
 The body reacts to a hydralazine-induced fall in blood pressure by increasing heart rate, myocardial contractility, and cardiac output. These compensatory responses can be detrimental to patients with coronary artery disease and are minimized by the concurrent administration of a β-adrenergic antagonist.
The body reacts to a hydralazine-induced fall in blood pressure by increasing heart rate, myocardial contractility, and cardiac output. These compensatory responses can be detrimental to patients with coronary artery disease and are minimized by the concurrent administration of a β-adrenergic antagonist.
 Fenoldopam mesylate (infusion rates studied in clinical trials range from 0.01-1.6 mcg/kg/min) reduces systolic and diastolic blood pressure in patients with malignant hypertension to an extent comparable to nitroprusside.
Fenoldopam mesylate (infusion rates studied in clinical trials range from 0.01-1.6 mcg/kg/min) reduces systolic and diastolic blood pressure in patients with malignant hypertension to an extent comparable to nitroprusside.
 Dihydropyridine calcium channel blockers preferentially dilate arterial vessels, often preserving or increasing cardiac output.
Dihydropyridine calcium channel blockers preferentially dilate arterial vessels, often preserving or increasing cardiac output.
Hypotensive Agents: Introduction
A multitude of drugs are capable of lowering blood pressure, including volatile anesthetics, sympathetic antagonists and agonists, calcium channel blockers, β-blockers, and angiotensin-converting enzyme inhibitors. This chapter examines agents that may be useful to the anesthesiologist for intraoperative control of arterial blood pressure.
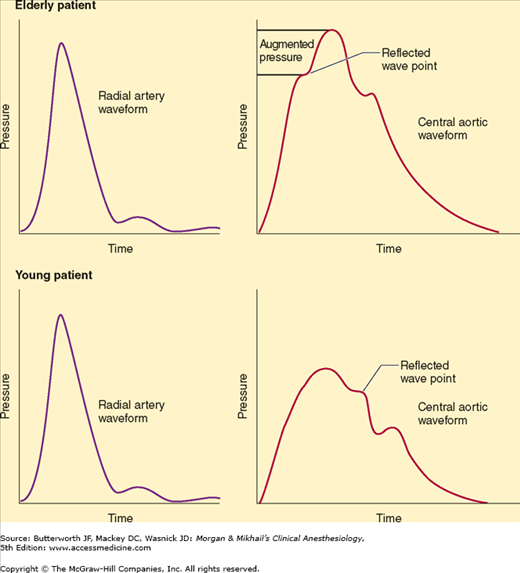
Patients with an increasing “vascular age” routinely present for anesthesia and surgery. As patients chronologically age, so too does their vasculature. When a pulse wave is generated by ventricular contraction, it is propagated through the arterial system. At branch points of the aorta, the wave is reflected back toward the heart. In patients of young vascular age, the reflected wave tends to augment diastole, improving diastolic pressure. In patients with “older” vasculature, the wave arrives sooner, being conducted back by the noncompliant vasculature during late systole, which causes an increase in cardiac workload and a decrease in diastolic pressure (Figure 15-1). Thus, older patients develop increased systolic pressure and decreased diastolic pressure.
Figure 15-1
Illustration of the influence of increased vascular stiffness on peripheral (radial) and central (aortic) pressures. Note the similarity of peripheral radial pressures in individuals with normal (lower left panel) and increased (upper left panel) vascular stiffness. In young individuals with normal vascular stiffness, central aortic pressures are lower than radial pressures (lower panels). In contrast, in older individuals with increased vascular stiffness, central aortic pressures are increased and can approach or equal peripheral pressures as a result of wave reflection and central wave augmentation during systole (top panels). (Reproduced, with permission, from Barodka V, Joshi B, Berkowitz D, Hogue CW Jr, Nyhan D: Implications of vascular aging. Anesth Analg 2011;112:1048.)
Widened pulse pressures (the difference between systolic and diastolic pressures) have been associated with both increased incidence of postoperative renal dysfunction and increased risk of cerebral events in patients undergoing coronary bypass surgery. Consequently, control of blood pressure is essential to mitigate postoperative morbidity, especially as patients of advanced vascular age present for surgery.
β-Blocker therapy should be maintained perioperatively in patients who are being treated with β-blockers as a part of their routine medical regimen. Furthermore, according to the American College of Cardiology, β-blockers are also of potential benefit to patients with more than one cardiac risk factor, especially those who are undergoing vascular surgery. However, the routine administration of high-dose β-blocker therapy may, in the absence of dose titration, be harmful in patients not taking β-blockers. The American College of Cardiology/American Heart Association guidelines for β-blocker use perioperatively should be closely followed. Adherence to such guidelines is used by third parties as a “quality” performance indicator for anesthesia delivery. Thus, anesthesia providers should periodically review recommendations regarding β-blocker therapy, as guidelines evolve as new evidence becomes available and older evidence is refuted. β-Blockers (esmolol, metoprolol, and others) were previously discussed for the treatment of transient perioperative hypertension and are routinely used by anesthesia providers. This chapter discusses antihypertensive agents other than β-blockers that are used perioperatively.
Along with increased vascular age, diastolic dysfunction is often underestimated in patients, as it can present in individuals with preserved systolic function. Acute diastolic heart failure can develop in the perioperative period secondary to hypertensive crisis. Diastolic dysfunction occurs due to the inability of the heart to relax effectively. Failure to actively sequester calcium ion into the sarcoplasmic reticulum (an energy-dependent process) impedes relaxation. Acute hypertension can produce diastolic dysfunction perioperatively, leading to elevated left ventricular end-diastolic pressures, myocardial ischemia, and pulmonary edema. Consequently, as increasing numbers of patients have diastolic dysfunction, tight control of blood pressure perioperatively is essential for safe anesthetic practice.
Blood pressure is essentially the product of cardiac output and systemic vascular resistance. Agents that lower blood pressure either reduce the force of myocardial contraction and/or produce vasodilatation of the arterial and venous capacitance vessels. Agents used to lower blood pressure include nitrovasodilators, calcium antagonists, dopamine agonists, anesthetic agents, and angiotensin-converting enzyme inhibitors. β-Blockers have been previously discussed.
Nitrovasodilators
Sodium nitroprusside and other nitrovasodilators relax both arteriolar and venous smooth muscle. Its primary mechanism of action is shared with other nitrates (eg, hydralazine and nitroglycerin). As these drugs are metabolized, they release nitric oxide, which activates guanylyl cyclase. This enzyme is responsible for the synthesis of cyclic guanosine 3′,5′-monophosphate (cGMP), which controls the phosphorylation of several proteins, including some involved in the control of free intracellular calcium and smooth muscle contraction.
Nitric oxide, a naturally occurring potent vasodilator released by endothelial cells (endothelium-derived relaxing factor), plays an important role in regulating vascular tone throughout the body. Its ultrashort half-life (<5 s) provides sensitive endogenous control of regional blood flow.  Inhaled nitric oxide is a selective pulmonary vasodilator that is beneficial and routinely used in the treatment of reversible pulmonary hypertension.
Inhaled nitric oxide is a selective pulmonary vasodilator that is beneficial and routinely used in the treatment of reversible pulmonary hypertension.
Sodium nitroprusside is a potent and reliable antihypertensive. It is usually diluted to a concentration of 100 mcg/mL and administered as a continuous intravenous infusion (0.5-10 mcg/kg/min). Its extremely rapid onset of action (1-2 min) and fleeting duration of action allow precise titration of arterial blood pressure. A bolus of 1-2 mcg/kg minimizes blood pressure elevation during laryngoscopy but can cause transient hypotension in some patients. The potency of this drug requires frequent blood pressure measurements—or, preferably, intraarterial monitoring—and the use of mechanical infusion pumps. Solutions of sodium nitroprusside must be protected from light because of photodegradation.
After parenteral injection, sodium nitroprusside enters red blood cells, where it receives an electron from the iron (Fe2+) of oxyhemoglobin. This nonenzymatic electron transfer results in an unstable nitroprusside radical and methemoglobin (Hgb Fe3+). The former moiety spontaneously decomposes into five cyanide ions and the active nitroso (N=O) group.
The cyanide ions can be involved in one of three possible reactions: binding to methemoglobin to form cyanmethemoglobin; undergoing a reaction in the liver and kidney catalyzed by the enzyme rhodanase (thiosulfate + cyanide → thiocyanate); or binding to tissue cytochrome oxidase, which interferes with normal oxygen utilization (Figure 15-2).  The last of these reactions is responsible for the development of acute cyanide toxicity
The last of these reactions is responsible for the development of acute cyanide toxicity
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree