Fibromyalgia and Diffuse Illnesses
Karen Anderson Keith PhD, RN,CS, FNP
Robert Keith PA-C
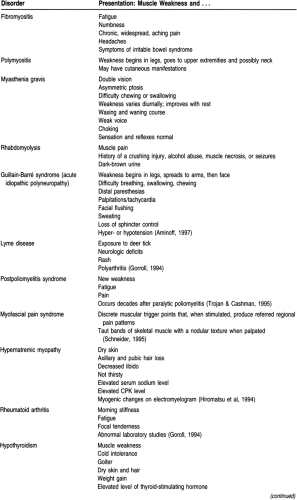
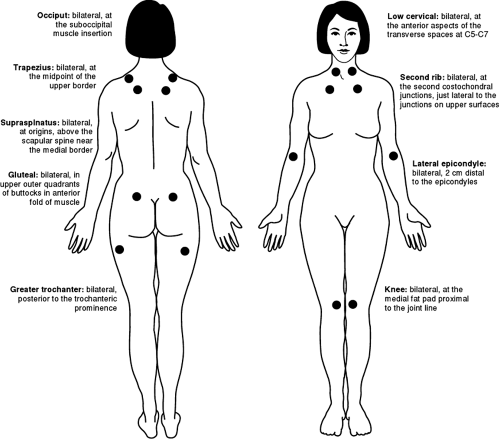
One of the most puzzling and frustrating problems confronting primary care providers is the evaluation of vague symptoms such as weakness, fatigue, or widespread pain. Often these complaints are self-limiting, and because a complete evaluation would require an in-depth workup, patients may be given a preliminary evaluation and asked to come back if the problems persist. If the problem does persist, patients are frequently referred to specialists for evaluation, with variable results. This chapter provides a framework for the initial assessment and evaluation of fibromyalgia, polymyositis, and myasthenia gravis, three conditions in which the chief complaints are weakness, fatigue, and widespread pain. Table 45-1 lists these and other diseases that can present with weakness. Primary care providers, through a relationship-centered approach to care, play an important role in the initial workup, ongoing management, and when indicated comanagement of patients with diffuse illnesses.
FIBROMYALGIA
Anatomy, Physiology, and Pathology
Although there is no clearly identified pathophysiologic process related to the development of fibromyalgia (FM) (Bennett, 1995), some believe that the syndrome is partially the result of aberrant central pain mechanisms (Bendtsen et al, 1997). FM has been identified as a systemic disease process associated with a dysfunctional limbic system or neuroendocrine axis (Schneider, 1995). Focal blood flow decreases, and low cerebral blood flow has been found in patients with FM (Johansson et al, 1995; Mountz et al, 1995). This has led to the conclusion that abnormal pain perception (a low pain threshold) in women with FM may be the result of central nervous system dysfunction. Patients with FM exhibit disturbances in three areas: their stress response systems (low basal cortisol levels), their hypothalamic–pituitary–adrenal axis (increased release of corticotropin [adrenocorticotropic hormone, or ACTH] to endogenous or exogenous corticotropin-releasing hormone with blunted cortisol response to ACTH and exercise), and their sympathetic nervous systems (lowered activity, particularly related to norepinephrine and serotonin), reflecting a possible stress-related pathophysiologic response (Crofford et al, 1996). FM can be a sequela to trauma (Waylonis & Perkins, 1994), resulting in typical facet joint inflammation (Bassan et al, 1995). The prevalence of carpal tunnel syndrome is higher in women diagnosed with FM than in the general population, along with a higher level of undiagnosed carpal tunnel syndrome in those with FM. Although traditional wisdom suggests that there is no weakness associated with FM, reduced quadriceps muscle strength in patients with FM has been reported (Norregaard et al, 1995a).
FM can be a complication of hypothyroidism, rheumatoid arthritis, or (in men) sleep apnea (Hellmann, 1997); phenobarbital use has been noted as a reversible cause of FM (Goldman & Krings, 1995). A sport-induced FM with facet joint irritation has also been identified as a cause (Bassan et al, 1995). In the final analysis, the etiology of FM is unknown; hypotheses include hypothyroidism, sleep disorders, depression, viral infection, or an abnormal perception of stimuli.
Epidemiology
FM is seen mostly in women (66% to 90% of those diagnosed with FM are women), aged 20 to 50. The disease affects 3% to 10% of the population (Hellmann, 1997). Of the 6 million Americans diagnosed with FM, 4 million are women (Bennett, 1995). FM is seen in the elderly but may present without specific complaints beyond physical decline or confusion (Michet et al, 1995); this seriously complicates the diagnostic challenge.
Diagnostic Criteria
The American College of Rheumatology (Wolfe et al, 1990) has developed classification criteria for FM based on a history of widespread pain for at least 3 months and pain in 11 of 18 identified points. Both criteria must be satisfied for the patient to be diagnosed with FM.
The history of diffuse pain must include:
Pain in the left side of the body
Pain in the right side of the body
Pain above the waist
Pain below the waist
Axial skeletal pain (cervical spine or anterior chest, or thoracic spine, or low back).
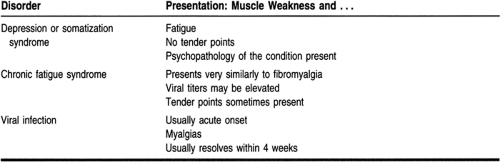
Pain in 11 of the 18 tender points must be bilateral and must be described as painful, not simply tender. Tender points (Fig. 45-1) are identified as:
Occiput at the suboccipital muscle insertion
Low cervical at the anterior aspect of the intertransverse spaces of C5 to C7
Trapezius at the midpoint of the upper border
Supraspinatus above the spine of the scapula near the medial border
Second rib at the second costochondral junctions, just lateral to the junctions on the upper surface
Lateral epicondyle 2 cm distal to the epicondyle
Gluteus in the upper outer quadrants of the buttocks in the anterior fold of the muscle
Greater trochanter posterior to the trochanteric prominence
Knee at the medial fat pad proximal to the joint line.
These are consensus criteria until more definitive findings are set out (Wolfe et al, 1990).
History and Physical Exam
A comprehensive approach to the history is essential in the evaluation of FM because of the diffuse nature of the symptoms. A detailed review of systems should be conducted. Complaints of fatigue, numbness, stiffness, chronic widespread aching pain (usually without perceived weakness), headaches, and symptoms of irritable bowel syndrome predominate. A sleep history, with particular attention to the quality, not just the amount, of sleep, should be elicited (Schaefer, 1995). Many patients with FM complain of waking from sleep unrefreshed. Symptoms of depression (feelings of sadness, change in sleeping or eating patterns, difficulty falling asleep, early morning awakening, difficulty completing normal daily activities, decreased libido, suicidal ideation, as well as weakness and fatigue) should be explored, as should those of hypothyroidism (cold intolerance, constipation, weight change, hoarseness, dry skin, menorrhagia, as well as weakness, fatigue, and depression). The impact of the symptoms on the patient’s relationships, employment, and social life and current stressors and coping methods should be assessed. Any history of fever, muscle injury, rash, or symptoms of arthritis must be elicited.
Ascertaining the location of the pain is very important; the pain of FM is located by applying pressure to the tender points (see Fig. 45-1) until the provider’s fingers blanch slightly. The pain or tenderness elicited is diffuse as opposed to the localized, regional pain of myofascitis. Symptoms of FM wax and wane and may be exacerbated by weather changes as well as poor sleep and other stressors.
The patient is usually afebrile and exhibits no weight loss. A complete physical exam should include in-depth musculoskeletal and neurologic exams. On the general exam, the skin, nails, mucous membranes, and fundi should be carefully evaluated for rheumatoid disease, myopathy, osteoarthropathy, thyroid disease, and focal pathology (Goroll, 1994). The findings on the physical exam are typically normal, except for the usually symmetrical tenderness elicited by pressure on the tender points.
Diagnostic Studies
The results of laboratory studies are usually normal, but these studies are important to eliminate other conditions as the cause of symptoms. Customary laboratory studies include a complete blood count (CBC) and erythrocyte sedimentation rate (ESR) (may show an elevated ESR in arthritis or lupus), thyroid function tests (because FM may be a result of hypothyroidism) (Hellmann, 1997), and creatine phosphokinase level (usually elevated in polymyositis). Further testing becomes costly and is usually noncontributory. Lyme titers can be useful if the patient has symptoms of Lyme disease (rash, fever, neurologic symptoms, arthritis symptoms, exposure to deer ticks). If fatigue is the outstanding complaint and the history and physical exam do not point to a diagnosis, a more extensive workup is necessary.
The diagnosis of FM is one of exclusion. The differential includes rheumatoid arthritis (early morning stiffness that may improve during the day and worsens after exercise; symmetrically erythematous, edematous joints, particularly of the fingers and toes; elevated ESR, rheumatoid factor), systemic lupus erythematosus (rash over exposed areas; decreased hemoglobin, platelets, and white cells; positive antinuclear antibody preparation), polymyositis (weakness, not pain), and polymyalgia rheumatica (patient usually older than 50; shoulder and hip girdle pain; elevated ESR; frequently associated with temporal arteritis) (Hellmann, 1997).
Treatment Options, Expected Outcomes, and Comprehensive Management
Because patients frequently seek many opinions before they are diagnosed with FM, feelings of shame and embarrassment may predominate. These feelings can be increased when health care providers have expressed frustration, impatience, or suspicions of malingering in reaction to the patient’s symptoms. An atmosphere of support must be provided for patients diagnosed with FM. Often just the knowledge that they have a recognizable syndrome shared with others produces comfort (Hellmann, 1997). Patients with FM are often depressed and frustrated because of the difference between their symptoms and their perception of illness and the objective findings (Henriksson, 1995a). This can prevent a patient from taking an active part in the treatment of FM. Patients must be assured that the duration of symptoms does not predict the long-term outcome (Wigers, 1996) and that FM is not a progressive disease. Patients must be made aware that there is not one, single treatment option that works in all cases (Hellmann, 1997). Any approach to treatment must be holistic and empathetic (Bennett, 1995); the goal of any therapeutic regimen is the resumption of normal or near-normal activity levels.
Pharmacologic treatment of FM is generally unsatisfactory. Nonsteroidal anti-inflammatories and other pain relievers are generally not effective, but individual patients may report feeling better when taking them. The possible benefits of over-the-counter or prescription pain relievers should be discussed with the patient in the context of the therapeutic benefits versus the effects of prolonged use and the risk of side effects. Amitriptyline has been used with some success; the dose is titrated beginning at 10 mg at bedtime and gradually building to 40 or 50 mg at bedtime (Hellmann, 1997). Tricyclic antidepressants can cause heart conduction problems, and an electrocardiogram should be obtained before the tricyclic is begun (Retfalvi et al, 1997). Tricyclics and nonsteroidal anti-inflammatories have been shown to work synergistically in relieving pain (Goldenberg, 1989). Although some advocate the use of selective serotonin reuptake inhibitors, their efficacy is still in question (Norregaard et al, 1995b). Lidocaine injection, although recommended by some (Bassan et al, 1995), is not always effective (Scudds et al, 1995). For patients with severe, debilitating pain, a pain management consultation may be required.
Patients frequently request antibiotics, with the notion that there must be something “going on” that causes their symptoms. Providers should work with patients to explain the use
and efficacy of antibiotic treatment and the toxicities that can result from antibiotic treatment. Some patients may also question the role of magnesium and selenium in their condition, but at this time there is no conclusive information on their effectiveness (Eisinger et al, 1994).
and efficacy of antibiotic treatment and the toxicities that can result from antibiotic treatment. Some patients may also question the role of magnesium and selenium in their condition, but at this time there is no conclusive information on their effectiveness (Eisinger et al, 1994).
Most useful to patients with FM is a gradually progressive exercise regimen. The exact mechanism by which this helps is not clear, but many patients report feeling better when engaged in a regular exercise program. Contradictory results, however, have been noted, and general feelings of fatigue, exercise-induced extremity pain, and exertion were found to be significantly higher for women with FM than for normal controls, although there was no difference in their pre-existing cardiovascular fitness (Mengshoel et al, 1995b). Stress reduction is an important aspect of the treatment of FM. Some useful methods include a regular exercise regimen (as noted previously), yoga (although stretching has not been shown to benefit FM, the relaxation of yoga can be useful), biofeedback, acupuncture, acupressure, transcutaneous electrical nerve stimulation, scheduled recreational activities, and other individualized activities. To identify these activities, patients must be questioned about their favorite recreational activities, which may include active participation in social events or quiet activities such as crossword puzzles, sewing, or reading.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree