Fig. 52.1
Cervical spine x-ray with findings suggestive of gas density within the posterior soft tissues of the neck
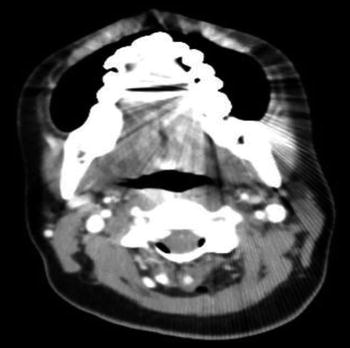
Fig. 52.2
Computed tomography scan with contrast of the head, neck, and soft tissue revealing cervical 1 through cervical 4 epidural air exiting into the right paraspinal and posterior subcutaneous tissue of the neck, tracking along fascial planes
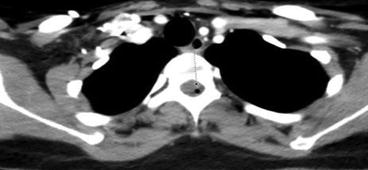
Fig. 52.3
Computed tomography scan with contrast of the thoracic spine revealing a small focus of epidural air is seen at thoracic 3 level
52.2 Case Discussion
Pneumorrhachis , also known as aerorachia , describes an uncommon phenomenon, the presence of gas in the spinal canal [1]. Pneumorrhachis is distinguished from pneumocephalus, the presence of intracranial gas [2]. Pneumorrhachis can be intradural or extradural. The extradural category also is known as epidural air , epidural pneumatosis , or epidural emphysema . Because of the lower resistance from loose connective tissue, as compared with the rich vascular network anteriorly, the epidural air usually collects in the posterior epidural space [3].
52.3 Etiology and Pathogenesis
Epidural emphysema has been described in association with the iatrogenic, traumatic, and nontraumatic clinical scenarios (Table 52.1) [3]. Iatrogenic causes of epidural emphysema are: (1) epidural anesthesia and using the widely applied loss of resistance to air technique, (2) inadvertent infusion of air through an epidural catheter, and (3) other surgical or diagnostic intervention invading the epidural space. Traumatic causes of epidural emphysema are penetrating spinal injury, skull fractures, or traumatic pneumothorax and pneumomediastinum. The air dissects through fascial planes into paraspinal connective tissue, along vascular and nerve root sheaths, and through the neural foramina into the epidural space [3]. The fascial plane in the mediastinum communicates with the fascial plane in the epidural space. Barotrauma increases pressure gradients and is the most common cause of clinically significant epidural emphysema [4]. Air can move through these tracts when a pressure gradient forms after high intrathoracic or intra-abdominal pressure is transduced to the epidural space. The air is then trapped when the skin and subcutaneous tissue act as a one-way valve. Nontraumatic epidural emphysema happens with epidural infections by a gas-forming organism or abscess formation, rupture of a vacuum disc, or spontaneous pneumothorax or pneumomediastinum. Degenerative discs may contain air. The presence of gas within an intervertebral disc is found in 2–3% of the population [5]. Herniation of the discs can lead to epidural emphysema. Similar to traumatic barotraumas, spontaneous pneumothorax and pneumomediastinum dissect air along fascial planes into neuroforamen to the epidural space.
Table 52.1
Causes of epidural emphysema
Iatrogenic: • Epidural anesthesia • Surgical and diagnostic interventions |
Traumatic: 1. Penetrating spinal injury 2. Skull fracture 3. Traumatic pneumothorax or pneumomediastinum Air pathways • Conditions producing high intrathoracic pressure and barotrauma • Dissecting through paraspinal soft tissues through neural foramina in nerve root sheaths |
Nontraumatic: • Infection by gas-producing organism • Vacuum disc phenomenon • Spontaneous pneumothorax or pneumomediastinum |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






