CHAPTER 51 Emergency Dialysis and Ultrafiltration
MANAGEMENT OF critically ill patients with acute kidney injury (AKI) in the intensive care unit (ICU) often necessitates emergency dialysis for optimization of volume and metabolic status.1 AKI often develops as one of the manifestations of multiple organ failure1–4 and is an independent risk factor for mortality.5–7 Despite technological advances in renal replacement therapy (RRT) and improved delivery methods, the in-hospital mortality rate associated with AKI ranges from 35% to 80% in critically ill patients.1–5,8–11 This may be in part explained by the fact that presently no effective pharmacologic therapy exists for AKI and that RRT is only a supportive therapy for AKI. However, timing of initiation and dose and modality of RRT may affect the outcomes.12–13 This chapter describes the different modalities of RRT and addresses the basic principles regarding selection of different RRT for management of patients with renal failure and/or volume overload in the cardiac intensive care unit (CICU).
Indications for Renal Replacement Therpy
In a multinational study, the prevalence of AKI requiring RRT in the ICU was reported at 5.7%.1 More importantly, there is an increasing need for dialysis in the CICU as highlighted in a recent study from the ADHERE registry stating that 91% of the patients hospitalized for acute decompensated heart failure (ADHF) had some degree of renal failure, with 64% having at least moderate renal failure and that 14% of them required initiation of RRT.14
The basic goals for management of patients with AKI are maintenance of fluid and electrolyte balance, avoidance of nephrotoxic agents (i.e., aminoglycosides, radiocontrast agents, etc.), maintenance of adequate nutrition, and appropriate dosing of medications according to the renal function.15 When conservative therapy fails to achieve optimal fluid and metabolic control, dialysis is initiated. The most widely accepted indications for RRT in patients with AKI are: (1) fluid overload refractory to diuretics; (2) hyperkalemia (usually serum potassium >6.5 mEq/L); (3) severe metabolic acidosis (arterial pH <7.1); (4) signs of uremia, such as pericarditis, neuropathy, or unexplained altered mental status. However, there is a wide disparity among nephrologists regarding the timing of initiation of dialysis based on concentrations of blood urea nitrogen (BUN) or serum creatinine and/or urine output in the ICU.16–19
Principles and Technical Aspects of Renal Replacement Therapy
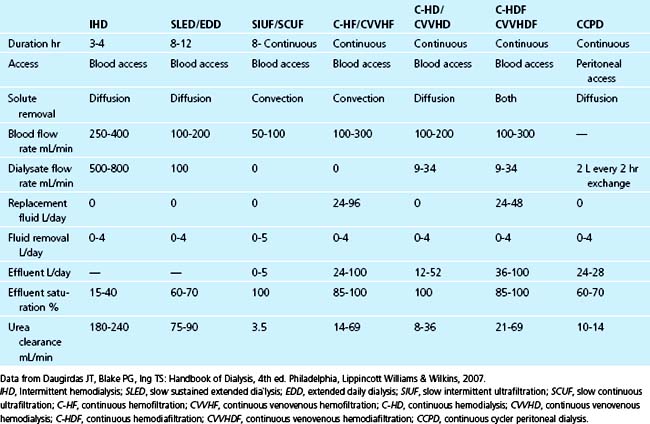
There are multiple modalities of dialysis that are included under RRT and are summarized in Table 51-1. The comparison of solute removal and main features of various techniques are summarized in Table 51-2. These modalities mainly differ in the principles of solute removal and rate of solute removal. Solute removal during dialysis occurs by three mechanisms: (1) passive diffusion of solutes between the plasma and the dialysis fluid along their concentration gradient; (2) convection (i.e., dragging of the solutes along with the plasma water across the filter membrane); and (3) adsorption of solutes to the filter membrane. Each modality will be discussed in the following sections.
Table 51–1 Modalities of Renal Replacement Therapy
| Intermittent Therapies | Hybrid Therapies | Continuous Therapies |
|---|---|---|
CAVHD, Continuous arteriovenous hemodialysis; CVVHDF, Continuous venovenous hemodialysis; CAVHF, Continuous arteriovenous hemofiltration; CVVHF, Continuous venovenous hemofiltration; CAVHDF, Continuous arteriovenous hemodiafiltration; CVVHDF, Continuous venovenous hemodiafiltration.
Continuous Renal Replacement Therapies (CRRT)
The concept of continuous dialysis was introduced in the 1960s, but only recently has this modality become well established in the ICU.20 Solute removal is achieved either by convection, diffusion, adsorption, or a combination of these methods depending upon the prescription. It is the therapy of choice in critically ill patients who are hemodynamically unstable and are in need of dialysis. The therapy is intended to run 24 hours a day. Depending on the mechanism of solute removal, CRRT are subclassified into continuous venovenous hemofiltration (CVVH), continuous venovenous hemodialysis (CVVHD), continuous venovenous hemodiafiltration (CVVHDF), and slow continuous ultrafiltration (SCUF).
CVVH uses convection for solute removal with ultrafiltration rates (fluid removal rate) on an average of 1 to 4 L/hr. Fluid balance is achieved by replacing the ultrafiltrate with a physiologic electrolyte–based replacement solution, which can be infused either before or after the dialyzer. Solute removal in CVVH is regulated by the characteristics of the membrane and on the site of replacement solution administration, either predialyzer (predilution hemofiltration) or postdialyzer (postdilution hemofiltration). For the same effluent flow rate, clearance in predilution hemofiltration mode is less than that in postdilution hemofiltration. However, because of the dilution of blood by the replacement fluid before entering the dialyzer, much higher filtration fractions (larger effluent flow rate and replacement fluid rate) are feasible in predilution hemofiltration.21 By contrast, CVVHD uses only dialysate and hence, removes solute by diffusion. The dialysate flow rates (9 to 34 mL/min)22 in this modality are significantly lower than the dialysate flow rates in IHD and SLED/EDD. CVVHDF, as the name implies, uses both dialysate and replacement fluid and thus uses both diffusive and convective clearance.23 Finally, SCUF does not use either dialysate or replacement fluid and is primarily used for optimization of volume status in patients that are hemodynamically unstable. Hence, CRRT techniques differ in the mechanism of solute removal. Despite the difference in the mechanism of solute clearance to achieve metabolic control, no study to date has clearly demonstrated improved clinical outcomes based on the different modality of CRRT.
The CRRT modalities can be performed using either an arteriovenous or venovenous circuit. Pump-driven venovenous circuits are better because they allow for higher solute clearance and also eliminate the need for arterial cannulation.24 A prospective study comparing two consecutive groups of patients with AKI treated with either CVVHD (25 patients) or CAVHD (continuous arteriovenous hemodialysis, 28 patients) revealed a greater amount of hourly ultrafiltrate (mean, 590 mL versus 424 mL; P < 0.001) with CVVHD, but urea and creatinine clearances were not significantly different between the two groups. The major advantage of CVVHD was the substantial decrease in the number of access-related complications (2 versus 10; P < 0.025). Therefore the use of venovenous circuit is preferred over arteriovenous circuit.24
CRRT Compared with IHD
CRRT is superior to IHD for the management of patients with AKI, particularly in patients that are hemodynamically unstable. The gradual removal of fluid and solute during CRRT enhances hemodynamic stability, which allows for increased salt and water removal and aggressive nutritional support. Furthermore, enhanced clearance of inflammatory mediators, particularly with hemofiltration in patients with concomitant sepsis, might provide additional benefits.25–27
However, to date no study has shown a survival benefit with CRRT when compared with IHD. This might be in part explained by the fact that most of the studies comparing IHD and CRRT have been nonrandomized observational studies or retrospective case series in which analysis was confounded by variations in disease severity among treatment groups.28–32 In a multicenter study, conducted at four academic medical centers in Southern California, Mehta and colleagues33 randomized 166 patients with AKI to IHD or CRRT. In the primary intention-to-treat analysis, 28-day all-cause mortality was 59.5% in patients that were randomized to CRRT compared with 41.5% in patients randomized to IHD (P < 0.02). However, unbalanced randomization had resulted in more patients with significantly higher APACHE III scores and a higher prevalence of liver failure in the CRRT group, both of which are associated with increased mortality. Adjustment for this imbalance in randomization using multivariate techniques yielded an adjusted odds of death associated with CRRT of 1.58 (95% CI 0.7 to 3.3). Similarly, Swartz and colleagues34 used multivariate regression to adjust for severity of illness in 349 patients and reported that the adjusted risk of death associated with CRRT was 1.09 (95% CI 0.67 to 1.80) compared with IHD, which suggests neither a benefit nor a hazard associated with modality of dialysis. Since then, two meta-analyses35,36 comparing CRRT and IHD have shown improved outcomes with CRRT, but these results have not been supported by any of the randomized trials. In aggregate, after randomization of more than 700 patients, no survival benefit can be ascribed to modality of dialysis therapy.
Several studies37–39 have reported that despite the absence of a survival benefit, CRRT is associated with improved recovery of renal function compared with IHD. The analyses used in these studies, however, only considered recovery of renal function in surviving patients, and did not adjust for differences in mortality between the treatment groups. Reanalyzing the data using an end point that combines both mortality and nonrecovery of renal function demonstrated no apparent difference in outcome between groups.40 Similarly, no difference in recovery of renal function was observed in three recent randomized trials.41–43 Thus current data do not suggest improved recovery of renal function with CRRT. Although SLED has similar hemodynamic effects and metabolic control as CRRT,44 currently no study has compared outcomes between SLED and other modalities.
In summary, current data suggest that survival and recovery of renal function are similar with both IHD and CRRT. In the majority of patients, selection of modality should therefore be based upon local expertise and available resources. In selected patients, CRRT may provide enhanced hemodynamic stability, and better management of volume status and nutritional requirements. It also provides for better preservation of cerebral perfusion in patients with brain injury or fulminant liver failure.45
Optimal Timing for Initiation of RRT
In its early use, IHD was initiated only once advanced signs and symptoms of uremia and volume overload had set in.46–47 Despite control of these symptoms, no reduction in mortality was demonstrated. This led to the concept of “prophylactic” IHD.48 Three retrospective studies reported that early (defined as BUN less than 93 to 150 mg/dL) versus late initiation of dialysis (BUN greater than 160 to 200 mg/dL) was associated with improved survival (43% to 75% for early dialysis versus 12% to 58% for late dialysis).49,50 Another prospective study of 18 patients reported better survival (69% versus 20%) with early initiation of dialysis (BUN <60 versus 150 mg/dL).51 Similarly, using the Program to Improve Care in Acute Renal Disease (PICARD) database, a multicenter observational study for AKI, Liu and colleagues13 reported that patients in the “high” BUN group at time of initiation of dialysis had slightly lower survival rates at 14 and 28 days despite having a reduced burden of organ failure when compared with patients in the “low” BUN group. This result was not confirmed by another prospective study of 34 patients with AKI, which showed no difference in mortality among patients who started dialysis at BUN of 60 mg/dL or later at 100 mg/dL.52
In relation to the timing of CRRT and clinical outcomes, three nonrandomized studies have reported improved outcomes, including improved survival with early versus late initiation of therapy.13,53–55 In a retrospective study of 100 consecutive patients treated with CVVH in a single shock trauma unit, survival was 39% among patients who were initiated on CVVH with BUN less than 60 mg/dL compared with 20% in patients with BUN greater than 60 mg/dL at the time of initiation of RRT.53
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree