CHAPTER 21 Conduction Disturbances in Acute Myocardial Infarction
Anatomy
The sinus node, sinoatrial conduction system, atrioventricular (AV) node, bundle of His, right bundle, left bundle dividing into anterior and posterior fascicle, and myocardial Purkinje fibers form components of the conduction system. The sinoatrial node is supplied by the atrial branch of the proximal right coronary artery (RCA) in 55% of cases and the proximal left circumflex artery in 45% of cases.1 The RCA perfuses the AV node and the proximal portion of the His bundle in most cases (left circumflex artery in 10% of cases). The septal branches of the left anterior descending artery supply the distal part of the His bundle, the right bundle branch, and the anterior fascicle of the left bundle branch. The posterior fascicle of the left bundle is supplied by septal branches from both the left anterior descending artery and the RCA.
Incidence
Based on multicenter retrospective reviews in the prethrombolytic era, left bundle branch block (LBBB) was the most common block, occurring in 38% of patients who had preexisting or new intraventricular conduction delay.2,3 This statement is controversial, however, because in 1975, Lie and coworkers4 found that complete LBBB secondary to acute MI is rare. Right bundle branch block (RBBB) with left anterior fascicular block (LAFB) was also common, occurring in 34% of patients who developed an intraventricular conduction delay. RBBB, RBBB with left posterior fascicular block (LPFB), and “alternating bundle branch block” occurred in 11%, 10%, and 6% of patients with new intraventricular conduction delay; isolated LAFB and LPFB were uncommon. Twenty-two percent of patients developed high-grade AV block or complete heart block.
In the thrombolytic era, the available data suggest that the incidence of complete heart block in acute MI may be lower with thrombolytic therapy at 4% to 5%,5 and the combined end point of complete heart block or second-degree AV block is 7% to 10%. The onset of complete heart block occurred within the first 2 days after MI in 81% of patients who developed complete heart block.
Specific Conduction Abnormalities
Sinoatrial Node
Sinus Bradycardia
Sinus bradycardia is the most common arrhythmia in inferior MI and three times more common in inferoposterior than anterior MI.6 Possible mechanisms include increased vagal tone (common), neurologic reflexes, and infarction or ischemia of the sinus node or the surrounding atrium.
Atrioventricular Node
Prolongation of the P–R interval (so-called first-degree block) can arise in the AV node, the bundle of His, or the bundle branches. AV nodal delay is usually seen in cases of occlusion of the RCA proximal to the right ventricular branch.8 This conduction abnormality may also manifest as second-degree AV block or complete AV block.
Below the Atrioventricular Node
The various forms of conduction abnormalities known to occur below the AV node include Mobitz II second-degree AV block, 2:1 AV block, and RBBB with or without left anterior or posterior fascicular block. RBBB is much more common than complete LBBB owing to dual supply of various fascicles of the left bundle and a wide area of distribution within the myocardium. The clinical prognosis is worse when RBBB plus LAFB is the result of the MI, predicting early death owing to pump failure.9
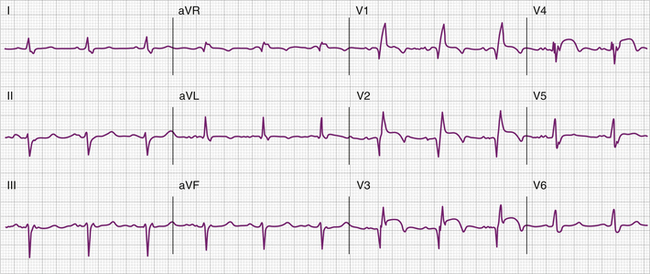
Complete heart block with inferior MI generally results from an intranodal lesion. It is associated with a narrow QRS complex, and develops in a progressive fashion from first-degree to second-degree to third-degree block (Fig. 21-1). It often results in asymptomatic bradycardia (40 to 60 beats/min) and is usually transient, resolving within 5 to 7 days. LBBB occurs as a form of aberration during bradycardia—either sinus bradycardia or AV block with a junctional escape mechanism. Complete heart block with anterior MI generally occurs abruptly in the first 24 hours. It can develop without warning or may be preceded by the development of RBBB with either LAFB or LPFB (bifascicular or trifascicular block) (Fig. 21-2).3 The escape rhythm is wide and unstable, and the event is associated with a high mortality (approximately 80%) from arrhythmias and pump failure. Heart block in this setting is thought to result from extensive necrosis that involves the bundle branches traveling within the septum.
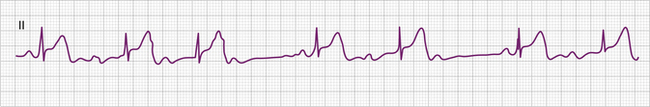
Figure 21-1 Mobitz type I atrioventricular block and inferior myocardial infarction.
(Courtesy of Ary Goldberger, MD.)