CHAPTER 5 Complications, toxicity, and safety
Complications and toxicity
Principles underlying complications and errors
Human factors can be defined as lapses in, or lack of, safe habit, or the occurrence of a vigilance decrement resulting from sleep deprivation, fatigue, recent alcohol or drug ingestion, or boredom. Inexperience on the part of the anesthesiologist is likely to contribute to poor decision-making or an error in judgment. An important component in the avoidance of complications arising from these factors is awareness of anesthesiologists as individuals and of their role in complication development. They should thus seek to establish safe working practices and individual self-discipline that may act to counterbalance these risks.1–3
Central nervous system toxicity
The signs and symptoms of local anesthetic-induced CNS toxicity are shown in Figure 5.1. An initial phase of CNS excitability, as demonstrated by light-headedness, dizziness, visual and auditory disturbance, muscle twitching, and convulsions, is followed by CNS depression, with coma, then respiratory depression and arrest. This sequence of events occurs because of an initial inhibition, at lesser concentrations, of inhibitory pathways in the amygdala. At greater concentrations, both inhibitory and excitatory pathways are inhibited, resulting in generalized CNS depression.5–8
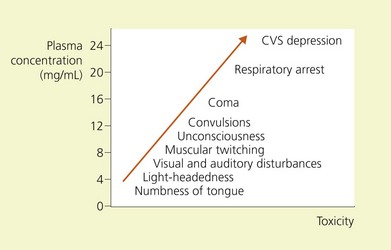
Figure 5.1 Relations of signs and symptoms of local anesthetic toxicity to plasma concentrations of lidocaine.
(From Ref. 4, Covino BG, Wildsmith JAW. Clinical pharmacology of local anesthetic agents. In: Cousins MJ, Bridenbaugh PO (eds). Neural blockade in clinical anesthesia and management of pain, 3rd edn. Philadelphia: © Lippincott-Raven; 1998.)
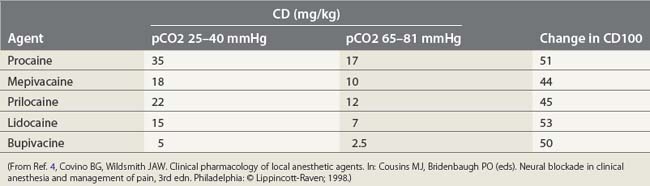
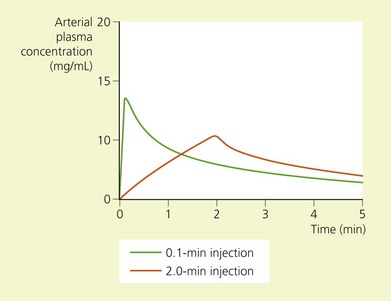
The toxic potential of each anesthetic drug is related to its potency as an anesthetic agent (Table 5.1),9 and the rate at which it is injected or absorbed (Fig. 5.2). Hypercapnia and acidosis lower the convulsive threshold for local anesthetic drugs. This occurs in a number of ways. A high pCO2 will increase cerebral blood flow, resulting in greater rates of drug delivery; decreased intracellular pH facilitates the formation of the cationic form of drug, i.e. the active form; and hypercapnia and acidosis result in diminished protein-binding of drug, thereby making available a greater proportion of free drug.10
(From Ref. 4, Covino BG, Wildsmith JAW. Clinical pharmacology of local anesthetic agents. In: Cousins MJ, Bridenbaugh PO (eds). Neural blockade in clinical anesthesia and management of pain, 3rd edn. Philadelphia, © Lippincott-Raven; 1998.)
Local anesthetic-induced seizures are effectively terminated by administration of barbiturate or benzodiazepine drugs.11,12 The doses required are small and one should remain mindful that their myocardial depressant effects are additive to those of local anesthetic drugs.
Cardiovascular system toxicity
The depolarization phase of the action potential in cardiac tissue differs from nerve tissue in that the fast influx of Na+ is followed by a slow influx of Ca2+. This influx of Ca2+ is responsible for the spontaneous depolarization that is characteristic of cardiac tissue (Fig. 5.3, Table 5.2). Local anesthetic drugs depress the maximal depolarization rate of the cardiac action potential, Vmax, secondary to inhibition of Na+ conductance. With increasing concentrations of local anesthetics, prolongation of conduction times occurs, producing an increase in the P–R interval and QRS duration. At greater concentrations this is followed by sinus bradycardia, sinus arrest, and atrioventricular dissociation.14,15 Local anesthetics also profoundly depress cardiac contractility, a phenomenon that may be related to the displacement of Ca2+ from the sarcolemma.16–18
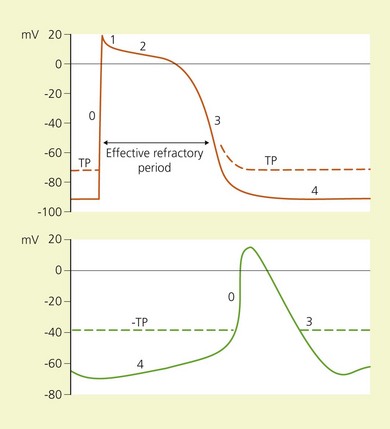
(From Ref. 13, Stoelting RK. Heart. In: Pharmacology and physiology in anesthetic practice. 2nd ed. Philadelphia, © JB Lippincott; 1991.)
Table 5.2 Ion movement during phases of the cardiac action potential
| Phase | Ion | Movement across cell membrane |
|---|---|---|
| 0 | Na+ | In |
| 1 | K+ | Out |
| Cl− | In | |
| 2 | Ca2+ | In |
| K+ | Out | |
| 3 | K+ | Out |
| 4 | Na+ | In |
(From Ref. 13, Stoelting RK. Heart. In: Pharmacology and physiology in anesthetic practice. 2nd ed. Philadelphia: © JB Lippincott; 1991.)
The CC/CNS ratio is that of the dosage required for cardiovascular collapse (CC) to the dosage required to produce convulsions. It is approximately 7.1 for lidocaine and 3.7 for bupivacaine, suggesting a greater margin of safety in the use of lidocaine.19 The high lipid-solubility of bupivacaine results in a slow rate of dissociation from the tissues, and thus a persistent effect on Vmax. Cardiovascular collapse resulting from bupivacaine is therefore resistant to treatment. The potential for cardiac toxicity is enhanced in pregnancy, for reasons not fully understood, and also in the presence of hypoxia and hypercapnia.20–22 These factors enhance the toxic potential of bupivacaine to a greater degree than they do lidocaine.
Peripheral vasculature
Local anesthetic drugs have a biphasic action on vascular smooth muscle.23 At low concentrations they produce vasoconstriction. As the concentration increases, the effect becomes one of vasodilatation. These observations have been explained as being due to stimulation of spontaneous myogenic activity at low concentrations and inhibition of the same at greater concentrations.
Nerve injury
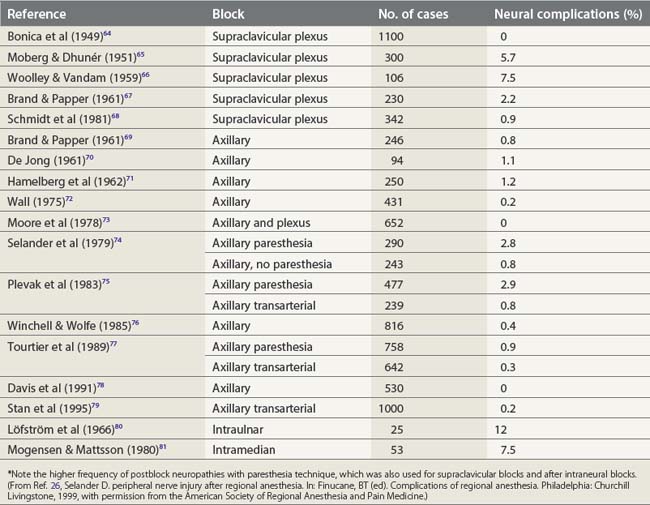
Nerve stimulation is one effective technique for locating a peripheral nerve. Prospective studies have demonstrated that a paresthesia technique can significantly increase the risk of postblock neuropathies (2.8%), while the transarterial approach to the brachial plexus is associated with paresthesia in as many as 40% of cases,24,25 producing neuropathy in 0.8% (Table 5.3). In contrast, a nerve stimulation technique aims to avoid nerve contact and has been shown to produce important block-related neuropathies in only 0–0.3% of cases.27
The risk of penetrating a nerve fascicle is reduced when a short-bevel (45°) needle is used, compared with a standard long-bevel (15°) needle, the reason being that nerve fascicles tend to roll away more readily from the advancing short-bevel needle tip.28 Although the incidence of injury is less with short-bevel needles, when injury does occur it is more severe.
Intraneural needle position is associated with painful paresthesias on injection, and intraneural injection causes nerve damage and cell death by mechanical disruption, disruption of the blood–nerve barrier, high endoneural pressure (above capillary perfusion pressure) (Fig. 5.4), and direct neurotoxicity of local anesthetic agent. This situation is further aggravated if the solution contains epinephrine.29,30 Therefore it is important to maintain verbal contact with the patient, avoid paresthesias, administer small incremental doses of drug, and reposition the needle if paresthesias are elicited.
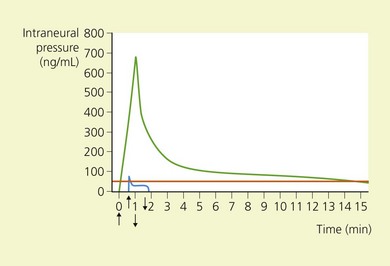
(From Ref. 26, Selander D. Peripheral nerve injury after regional anesthesia. In: Finucane, BT (ed). Complications of regional anesthesia. Philadelphia, Churchill Livingstone, 1999, with permission from the American Society of Regional Anesthesia and Pain Medicine.)
In attempting to establish the etiology of nerve lesions in the postoperative period, the differential diagnosis must initially take into account patient positioning, tourniquet use, surgical trauma, and the presence of tight casts or dressings.31–33 Follow-up of the patient in the immediate postoperative period will help to avoid inaccurate labeling of the deficit as ‘anesthesia-related’.
Allergic reactions
Allergic reactions to local anesthetics occur rarely.34 Indeed, most ‘allergic reactions’ to local anesthetics are in fact adverse reactions. Nevertheless, para-aminobenzoic acid is a product of the hydrolysis of ester local anesthetics and is a known allergen.35–37 Allergy to amide local anesthetics is still rarer. However, some preparations contain methylparaben (an allergen), because of its excellent bacteriostatic and fungistatic properties.38 After a case of allergy to a local anesthetic agent, intradermal testing of the full range of anesthetic agents is worthwhile, because allergy to one agent does not necessarily imply allergy to another.37,39
Infection
The presence of infection at the site of puncture is generally accepted as being a contraindication to regional anesthesia. The paucity of reports detailing infective complications of peripheral nerve block suggests that local and generalized infections following nerve blocks are rare. Disastrous infective complications continue to be reported following central neuraxial block, however, and the increasing use of peripheral nerve catheters suggests some elementary precautions be taken in this regard.40 Unfortunately, no recommendations exist as to aseptic technique for spinal, epidural, or peripheral nerve block.41 A review of the literature serves to highlight the following points:40
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree