Complication
Presentation
Cutaneous adverse reactions
Atrophy, alopecia, hyperpigmentation, folliculitis
Myonecrosis/myotoxicity
Attributed to local anesthetic or corticosteroid
Intra-arterial injection
Central nervous system manifestations
Cardiovascular manifestations
Subarachnoid injection
Brain stem anesthesia
45.2.5 Cutaneous Adverse Reactions
Depot steroid preparations are commonly used for occipital nerve blocks. Rare but well recognized, cutaneous side effects of local corticosteroid injections have been reported. Side effects include full-thickness soft tissue atrophy, alopecia, hyperpigmentation, and folliculitis (Fig. 45.1) [8–11]. The incidence of soft tissue atrophy after corticosteroid injection has been reported as <1% [12]. The risk of cutaneous adverse reactions appears to correlate with the quantity and solubility of the corticosteroid injected. Insoluble, particulate corticosteroids such as triamcinolone are more likely to cause adverse outcomes compared to soluble agents such as methylprednisolone or betamethasone. The underlying mechanism is associated with vasoconstriction of the surrounding vessels and deposit of insoluble crystals at the site, which results in atrophy of the skin and interruption of hair growth [12].


Fig. 45.1
Alopecia and cutaneous atrophy following an occipital nerve block
45.2.6 Myonecrosis
The exact mechanism of analgesia induced by corticosteroids is unknown but is attributed to their anti-inflammatory effects, which reduce chemical mediators that stimulate nociception. Intramuscular injection of local anesthetics and corticosteroid can lead to myonecrosis (Fig. 45.2). Lidocaine, bupivacaine, and mepivacaine have been found to be myotoxic. The pathogenesis of myotoxicity is complex. The muscle fibers hypercontract, degenerate, and swell with inflammatory cell infiltration and necrosis after injection. The underlying mechanism is thought to be the interaction of the local anesthetic with the sarcoplasmic reticulum. Intracellular calcium increases and further reuptake of calcium is inhibited, subsequently causing cell death [13]. Histological changes in the muscle are reversed between 2 to 5 weeks after initial insult to the muscle. Although muscle regeneration is expected, late-stage scarring has been reported. Concentration of local anesthetic correlates with degree of damage. The evidence that triamcinolone alone is myotoxic is limited, but a combination of triamcinolone and bupivacaine was more myotoxic than bupivacaine alone. A synergistic effect has been suggested with the two-drug combination. Corticosteroids seem to delay the regenerative process after bupivacaine-induced myonecrosis [14].
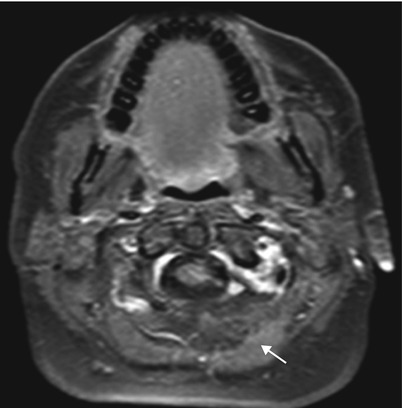
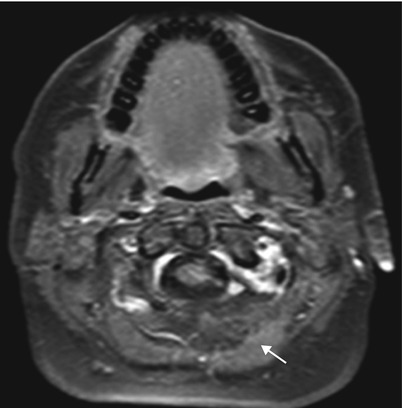
Fig. 45.2
Magnetic resonance imaging revealing atrophy of the left splenius capitius muscle (white arrow) after an occipital nerve block
45.2.7 Intra-arterial Injection
Intra-arterial injection of local anesthetic into the occipital artery can result in local anesthetic systemic toxicity. Substantial plasma concentrations of local anesthetics are required to produce central nervous system manifestations. Retrograde vascular spread along the occipital artery and then anterograde spread in the internal carotid artery makes the brain concentrations of local anesthetic high [15]. The classic symptoms of local anesthetic systemic toxicity are tinnitus, perioral numbness, agitation, confusion, seizures, and loss of consciousness (Table 45.2). Bradycardia and hypotension may progress to asystole and prolongation of the QTc interval and ventricular arrhythmia. In a review of published cases from 1979 to 2009, one study identified a total of 93 events of local anesthetic systemic toxicity, central nervous system toxicity in 89% of the cases, and cardiovascular toxicity in 51%. Simultaneous toxicity of both was 44%. The time of onset of symptoms ranged from less than 1 min to greater than 10 min after a single injection of local anesthetic [16].
Table 45.2
Local anesthetic systemic toxicity
Symptoms | Perioral numbness, metallic taste, tinnitus, agitation, coma |
|---|---|
Signs | Central nervous system: Seizure Cardiovascular system: Hyper- or hypotension, tachy- or bradycardia, ventricular arrhythmia, cardiac arrest
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|



