Fig. 16.1
Cross section of epidural space. (1) Ligamentum flavum, (2) epidural space with venous plexus, (3) spinal ganglion, (4) spinous process, (5) body of vertebra, (6) dorsal branch of spinal nerve, (7) ventral branch of spinal nerve (With permission from the Danilo Jankovic)

Fig. 16.2
Cross section at the level of the C6. (1) Ligamentum flavum, (2) anterior epidural space,(3) posterior epidural space, (4) subarachnoid space with the spinal cord,(5) spinal dura mater, (6) spinal pia mater, (7) epidural veins, (8) anterior and posterior spinal nerve roots (With permission from Danilo Jankovic)
Fig. 16.3
Cervical, thoracic, and lumbar spine (With permission from Danilo Jankovic)
Technique
Informed consent for cervical interlaminar epidural block must be conducted prior to the procedure. This should include a discussion of the potential advantages and risks both general and specific to the patient. The cervical epidural interlaminar block should be reserved for the experienced interventionist who is proficient in epidural blockade at the lumbar level. Intravenous access should be established and the block performed in an area where staff, drugs, and equipment are available for resuscitation. Regular monitoring of blood pressure and pulse oximetry should occur during and for 60 min following the procedure. The block can be performed in the sitting (Fig. 16.4), prone, or lateral recumbent positions, with a supportive nurse stabilizing the patient. Pre-syncope and syncope may occur when the block is performed in the sitting position [13] with the added risk of misplacement of the needle. This risk could be reduced with intravenous loading with a crystalloid or colloid solution and doses of a vasopressor as needed. Due to this risk, the prone position is preferred and can be aided with fluoroscopy. Fluoroscopy is recommended as the use of loss of resistance alone has been shown to have a high false positive rate [14].


Fig. 16.4
Patient positioning for the sitting approach to the cervical epidural interlaminar block using loss of resistance to saline
The cervical interlaminar epidural block is most commonly accessed between the C6/C7 and C7/T1 interspace. The volume of solution used is based on clinician preference with some authors recommending that sufficient spread is achieved with the use of 5 ml of solution [15]. Injection of similar volumes at either of these interspaces achieves a very similar spread of contrast solution [16].
When the cervical spine is in the extended position, there is the tendency for the ligamentum flavum to buckle toward the spinal cord and reduce the epidural space [17]. For this reason the patient is positioned with the cervical spine flexed as this maximizes the distance between the ligamentum flavum and the dura compared with the extended position. This flexion is achieved in the prone position through the patient having two pillows under their chest with the forehead resting on a rolled towel (Fig. 16.5).


Fig. 16.5
Patient positioning for the preferred prone approach. Pillows under the chest achieve good flexion of the cervical spine while still allowing for a clear face to support breathing. Fluoroscopy can be easily performed with this position
The technique should be performed with full sterile technique using mask, sterile gloves, and gown. Due to the ligamentum flavum being thinner at the cervical region, the loss of resistance may be more reliably detected with the use of a 16-gauge Tuohy needle rather than an 18 gauge. Using loss of resistance with saline in the syringe is recommended as using loss of resistance to air can rarely result in pneumocephalus [18] in the event of a dural puncture. With the spinous processes being quite horizontal, the direction of the needle should be perpendicular to the skin and therefore perpendicular to the floor in the prone position. The right-handed interventionist would stand on the patient’s left side when in the prone position. Ultimately fluoroscopy aids with direction and redirection as the needle is advanced.
On loss of resistance, careful aspiration of the needle should be performed as venous tap and dural puncture is generally only detected on aspiration of the needle. This is especially the case in the prone position due to the 10 cm of vertical height of the epidural needle.
A small volume (1–2 ml) of radiopaque contrast approved for epidural use can be injected to confirm the placement within the epidural space. Figure 16.6 demonstrates an epidurogram with a smaller volume of contrast solution, whereas Fig. 16.7 shows the normal appearance of an epidurogram with a larger volume of contrast.

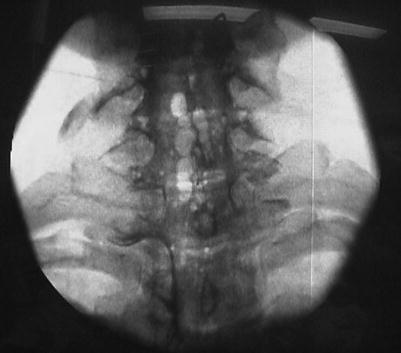





Fig. 16.6
Epidurogram of the cervical epidural space with a small volume of contrast solution. The epidural Tuohy needle is in position at the C7/T1 interspace
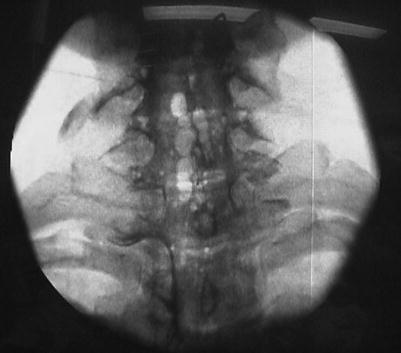
Fig. 16.7
Epidurogram of the cervical epidural space following a larger volume of contrast solution. Loss of resistance to air was used in this case with the bubbles of air visible in the epidural space following injection of the contrast solution
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








