Key Concepts
 Cardiopulmonary resuscitation and emergency cardiac care should be considered any time an individual cannot adequately oxygenate or perfuse vital organs—not only following cardiac or respiratory arrest.
Cardiopulmonary resuscitation and emergency cardiac care should be considered any time an individual cannot adequately oxygenate or perfuse vital organs—not only following cardiac or respiratory arrest.
 Regardless of which transtracheal jet ventilation system is chosen, it must be readily available, use low-compliance tubing, and have secure connections.
Regardless of which transtracheal jet ventilation system is chosen, it must be readily available, use low-compliance tubing, and have secure connections.
 Chest compressions and ventilation should not be delayed for intubation if a patent airway is established by a jaw-thrust maneuver.
Chest compressions and ventilation should not be delayed for intubation if a patent airway is established by a jaw-thrust maneuver.
 Attempts at intubation should not interrupt ventilation for more than 10 s.
Attempts at intubation should not interrupt ventilation for more than 10 s.
 Chest compressions should be immediately initiated in the pulseless patient.
Chest compressions should be immediately initiated in the pulseless patient.
 Whether adult resuscitation is performed by a single rescuer or by two rescuers, two breaths are administered every 30 compressions (30:2), allowing 3-4 s for each two breaths. The cardiac compression rate should be 100/min regardless of the number of rescuers.
Whether adult resuscitation is performed by a single rescuer or by two rescuers, two breaths are administered every 30 compressions (30:2), allowing 3-4 s for each two breaths. The cardiac compression rate should be 100/min regardless of the number of rescuers.
 Health care personnel working in hospitals and ambulatory care facilities must be able to provide early defibrillation to collapsed patients with ventricular fibrillation as soon as possible. Shock should be delivered within 3 min (± 1 min) of arrest.
Health care personnel working in hospitals and ambulatory care facilities must be able to provide early defibrillation to collapsed patients with ventricular fibrillation as soon as possible. Shock should be delivered within 3 min (± 1 min) of arrest.
 Lidocaine, epinephrine, atropine, naloxone, and vasopressin, but not sodium bicarbonate, can be delivered via a catheter whose tip extends past the tracheal tube. Dosages 2-2½ times higher than recommended for intravenous use, diluted in 10 mL of normal saline or distilled water, are recommended for adult patients.
Lidocaine, epinephrine, atropine, naloxone, and vasopressin, but not sodium bicarbonate, can be delivered via a catheter whose tip extends past the tracheal tube. Dosages 2-2½ times higher than recommended for intravenous use, diluted in 10 mL of normal saline or distilled water, are recommended for adult patients.
 If intravenous cannulation is difficult, an intraosseous infusion can provide emergency vascular access in children.
If intravenous cannulation is difficult, an intraosseous infusion can provide emergency vascular access in children.
 Because carbon dioxide, but not bicarbonate, readily crosses cell membranes and the blood-brain barrier, the resulting arterial hypercapnia will cause intracellular tissue acidosis.
Because carbon dioxide, but not bicarbonate, readily crosses cell membranes and the blood-brain barrier, the resulting arterial hypercapnia will cause intracellular tissue acidosis.
 A wide QRS complex following a pacing spike signals electrical capture, but mechanical (ventricular) capture must be confirmed by an improving pulse or blood pressure.
A wide QRS complex following a pacing spike signals electrical capture, but mechanical (ventricular) capture must be confirmed by an improving pulse or blood pressure.
Cardiopulmonary Resuscitation: Introduction
One goal of anesthesiology is to maintain the function of vital organ systems during surgery. It is not surprising, therefore, that anesthesiologists have played a major role in the development of cardiopulmonary resuscitation techniques outside the operating room.  Cardiopulmonary resuscitation and emergency cardiac care (CPR-ECC) should be considered any time an individual cannot adequately oxygenate or perfuse vital organs—not only following cardiac or respiratory arrest.
Cardiopulmonary resuscitation and emergency cardiac care (CPR-ECC) should be considered any time an individual cannot adequately oxygenate or perfuse vital organs—not only following cardiac or respiratory arrest.
This chapter presents an overview of the American Heart Association (AHA) and the International Liaison Committee on Resuscitation (ILCOR) Year 2010 recommendations for establishing and maintaining the ABCDs of cardiopulmonary resuscitation: Airway, Breathing, Circulation, and Defibrillation (Table 55-1, Figures 55-1 and 55-2). The 2010 CPR-ECC guidelines have been updated with new evidence-based recommendations. Still of import to the layperson are that the pulse should not be checked, and chest compression without ventilation may be as effective as compression with ventilation for the first several minutes. If a lay rescuer is unwilling to perform mouth-to-mouth ventilation, chest compressions alone are preferred to doing nothing. For the health care provider, defibrillation using biphasic electrical current works best and tracheal tube (TT) placement should be confirmed with a quantitative capnographic waveform analysis. More importantly, in the new guidelines, emphasis has been placed on the quality and adequacy of compressions, minimizing interruption time of compressions and the preshock pause (the time taken from the last compression to the delivery of shock).
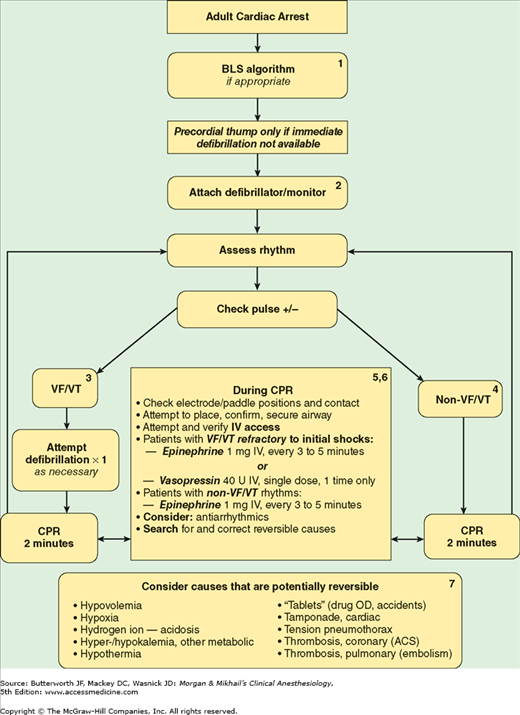
Figure 55-1
Universal algorithm for adult emergency cardiac care. BLS, basic life support; VF/VT, ventricular fibrillation and pulseless ventricular tachycardia; CPR, cardiopulmonary resuscitation. (Data from The American Heart Association BLS and ACLS Guidelines 2010 for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2010;122:S685.)
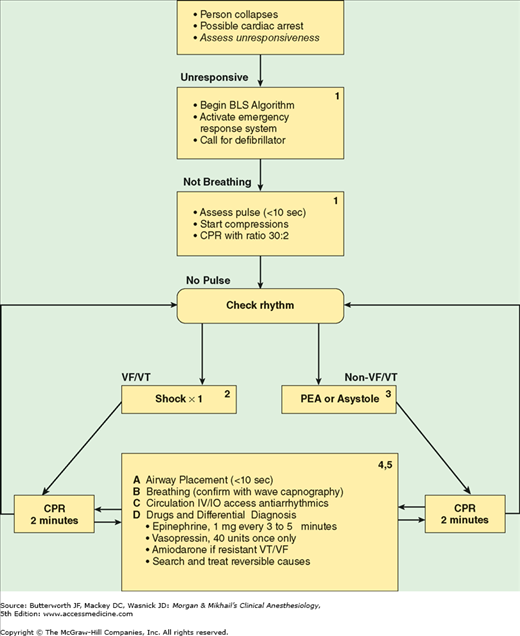
Figure 55-2
Comprehensive emergency cardiac care algorithm. BLS, basic life support; VF/VT, ventricular fibrillation and pulseless ventricular tachycardia; PEA, pulseless electrical activity; CPR, cardiopulmonary resuscitation. (Data from The American Heart Association BLS and ACLS Guidelines 2010 for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2010;122:S685.)
The sequence of steps in resuscitation has been changed in the 2010 guidelines from ABC (airway and breathing first, before compression) to CAB (compression first, with airway and breathing treated later). Emphasis has also been placed on physiological monitoring methods to optimize CPR quality and return of spontaneous circulation (ROSC). The rule of tens and multiples can be applied: less than 10 s to check for pulse, less than 10 s to place and secure the airway, target chest compression adequacy to maintain end-tidal pressure of carbon dioxide (PETCO2) greater than 10, and target chest compression to maintain arterial diastolic blood pressure greater than 20 and central venous oxygen saturation (SCVO2) greater than 30.
Changes in drug recommendations are notable for exclusion of atropine in the settings of pulseless electrical activity (PEA) and asystole, addition of the use of chronotropic drug infusions as an alternative to pacing in unstable/symptomatic bradycardia, and recommendation for use of adenosine in the management of wide-complex monomorphic tachycardia.
This chapter is not intended as a substitute for a formal course in either life support without the use of special equipment (Basic Life Support [BLS]) or with the use of special equipment and drugs (Advanced Cardiac Life Support [ACLS]). The recommendations described are for infants, children, and adults; resuscitation of neonates is discussed in Chapter 42.
Airway
Although the A of the mnemonic ABC stands for airway, it should also stand for the initial assessment of the patient. Before CPR is initiated, unresponsiveness is established and the emergency response system is activated. During low blood flow states such as cardiac arrest, oxygen delivery to the heart and brain is limited by blood flow rather than by arterial oxygen content; thus, in the new guidelines, greater emphasis is placed on immediate initiation of chest compressions than on rescuer breaths.
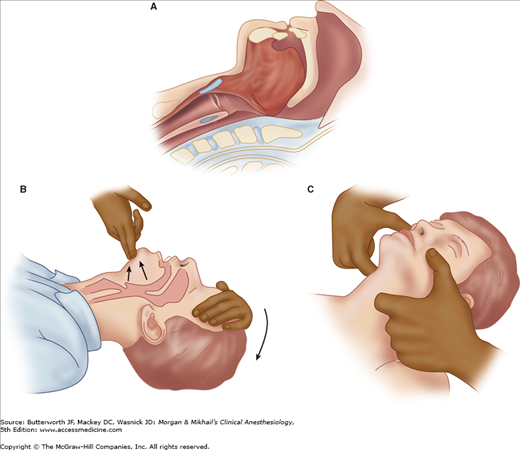
The patient is positioned supine on a firm surface. After initiation of chest compressions, the airway is evaluated. The airway is most commonly obstructed by posterior displacement of the tongue or epiglottis. If there is no evidence of cervical spine instability, a head-tilt chin-lift should be tried first (Figure 55-3). One hand (palm) is placed on the patient’s forehead applying pressure to tilt the head back while lifting the chin with the forefinger and index finger of the opposite hand. The jaw-thrust may be more effective in opening the airway and is executed by placing both hands on either side of the patient’s head, grasping the angles of the jaw, and lifting. Basic airway management is discussed in detail in Chapter 19, and the trauma patient is considered in Chapter 39.
Figure 55-3
Loss of consciousness is often accompanied by loss of submandibular muscle tone (A). Occlusion of the airway by the tongue can be relieved by a head-tilt chin-lift (B) or a jaw-thrust (C). In patients with possible cervical spine injury, the angles of the jaw should be lifted anteriorly without hyperextending the neck.
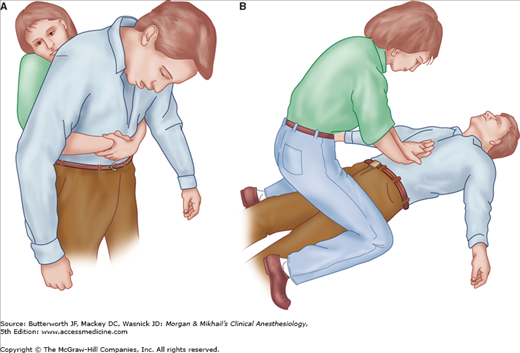
Any vomitus or foreign body visible in the mouth of an unconscious patient should be removed. If the patient is conscious or if the foreign body cannot be removed by a finger sweep, the Heimlich maneuver is recommended. This subdiaphragmatic abdominal thrust elevates the diaphragm, expelling a blast of air from the lungs that displaces the foreign body (Figure 55-4). Complications of the Heimlich maneuver include rib fracture, trauma to the internal viscera, and regurgitation. A combination of back blows and chest thrusts is recommended to clear foreign body obstruction in infants (Table 55-2).
| Infant (1-12 mo) | Child (>12 mo) | Adult | |
|---|---|---|---|
| Breathing rate | 20 breaths/min | 20 breaths/min | 10-12 breaths/min1 |
| Pulse check | Brachial | Carotid | Carotid |
| Compression rate | >100/min | 100/min | 100/min |
| Compression method | Two or three fingers | Heel of one hand | Hands interlaced |
| Compression/ventilation ratio | 30:2 | 30:2 | 30:2 |
| Foreign body obstruction | Back blows and chest thrusts | Heimlich maneuver | Heimlich maneuver |
If after opening the airway there is no evidence of adequate breathing, the rescuer should initiate assisted ventilation, by inflating the victim’s lungs with each breath using mouth-to-mouth, mouth-to-nose, mouth-to-stoma, mouth-to-barrier device, mouth- to-face shield, or mouth-to-mask rescue breathing or by using a bag-mask device (see Chapter 19). Breaths are delivered slowly (inspiratory time of ½-1 s) with a smaller tidal volume [Vt] (approximately 700-1000 mL, smaller [400-600 mL] if supplemental O2 is used) than was recommended in the past.
With positive-pressure ventilation, even with a small Vt, gastric inflation with subsequent regurgitation and aspiration are possible. Therefore, as soon as it is feasible, the airway should be secured with a TT, or, if that is not possible, an alternative airway should be inserted. There is inadequate evidence to support the optimal timing of the placement of an artificial airway; however, chest compressions should not be interrupted for more than 10 seconds to place any airway. Alternative airways include the esophageal-tracheal Combitube (ETC), laryngeal mask airway (LMA), pharyngotracheal lumen airway, King laryngeal tube, and cuffed oropharyngeal airway. The ETC and LMA, along with oral and nasopharyngeal airways, face masks, laryngoscopes, and TTs, are discussed in Chapter 19. Of these, the LMA is increasingly preferred for in-hospital arrests. The 2010 CPR-ECC guidelines recommend a TT as the airway adjunct of choice if personnel skilled in placing it are available.
Independent of which airway adjunct is used, the guidelines state that rescuers must confirm TT placement with a Petco2 detector—an indicator, a capnograph, or a capnometric device. The best choice for confirmation of TT placement is continuous capnographic waveform analysis. All confirmation devices are considered adjuncts to clinical conformation techniques (eg, auscultation). Once an artificial airway is successfully placed, it must be carefully secured with a tie or tape (25% of airways are displaced during transportation).
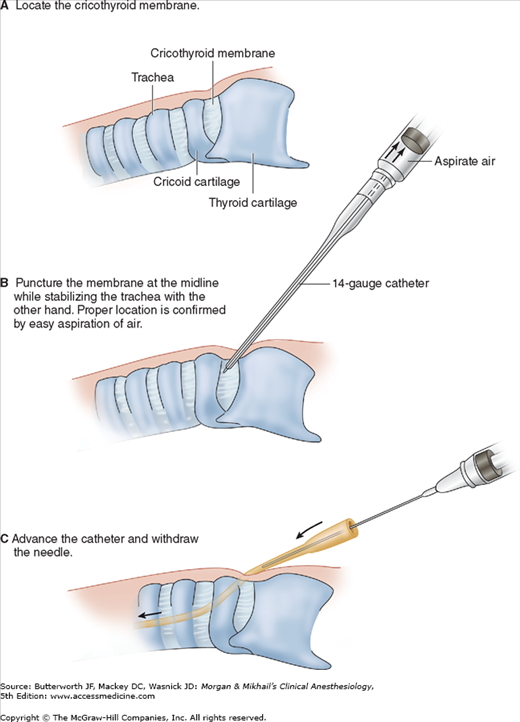
Some causes of airway obstruction may not be relieved by conventional methods. Furthermore, tracheal intubation may be technically impossible to perform (eg, severe facial trauma), or repeated attempts may be unwise (eg, cervical spine trauma). In these circumstances, cricothyrotomy or tracheotomy may be necessary. Cricothyrotomy involves placing a large intravenous catheter or a commercially available cannula into the trachea through the midline of the cricothyroid membrane (Figure 55-5). Proper location is confirmed by aspiration of air. A 12- or 14-gauge catheter requires a driving pressure of 50 psi to generate sufficient gas flow (for transtracheal jet ventilation). The catheter must be adequately secured to the skin, as the jet ventilation pressure can otherwise easily propel the catheter out of the trachea.
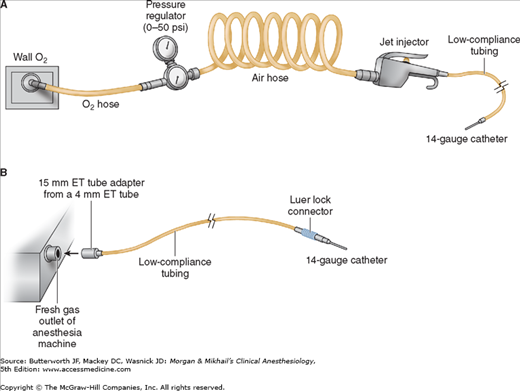
Various systems are available that connect a high-pressure source of oxygen (eg, central wall oxygen, tank oxygen, or the anesthesia machine fresh gas outlet) to the catheter (Figure 55-6). A hand-operated jet injector or the oxygen flush valve of an anesthesia machine controls ventilation. The addition of a pressure regulator minimizes the risk of barotrauma.
 Regardless of which transtracheal jet ventilation system is chosen, it must be readily available, use low-compliance tubing, and have secure connections. Direct connection of a 12- or 14-gauge intravenous catheter to the anesthesia circle system does not allow adequate ventilation because of the high compliance of the corrugated breathing tubing and breathing bag. One cannot reliably deliver acceptable ventilation through a 12- or 14-gauge catheter with a self-inflating resuscitation bag.
Regardless of which transtracheal jet ventilation system is chosen, it must be readily available, use low-compliance tubing, and have secure connections. Direct connection of a 12- or 14-gauge intravenous catheter to the anesthesia circle system does not allow adequate ventilation because of the high compliance of the corrugated breathing tubing and breathing bag. One cannot reliably deliver acceptable ventilation through a 12- or 14-gauge catheter with a self-inflating resuscitation bag.
Adequacy of ventilation—particularly expiration—is judged by observation of chest wall movement and auscultation of breath sounds. Acute complications include pneumothorax, subcutaneous emphysema, mediastinal emphysema, bleeding, esophageal puncture, aspiration, and respiratory acidosis. Long-term complications include tracheomalacia, subglottic stenosis, and vocal cord changes. Cricothyrotomy is not generally recommended in children younger than 10 years of age.
Breathing
Assessment of spontaneous breathing should immediately follow the opening or the establishment of the airway.  Chest compressions and ventilation should not be delayed for intubation if a patent airway is established by a jaw-thrust maneuver. Apnea is confirmed by lack of chest movement, absence of breath sounds, and lack of airflow. Regardless of the airway and breathing methods employed, a specific regimen of ventilation has been proposed for the apneic patient. Initially, two breaths are slowly administered (2 s per breath in adults, 1-1½ s in infants and children). If these breaths cannot be delivered, either the airway is still obstructed and the head and neck need repositioning or a foreign body is present that must be removed.
Chest compressions and ventilation should not be delayed for intubation if a patent airway is established by a jaw-thrust maneuver. Apnea is confirmed by lack of chest movement, absence of breath sounds, and lack of airflow. Regardless of the airway and breathing methods employed, a specific regimen of ventilation has been proposed for the apneic patient. Initially, two breaths are slowly administered (2 s per breath in adults, 1-1½ s in infants and children). If these breaths cannot be delivered, either the airway is still obstructed and the head and neck need repositioning or a foreign body is present that must be removed.
Mouth-to-mouth or mouth-to-mask (mouth-to-barrier-device) rescue breathing should be instituted in the apneic patient, even in the hospital setting when the crash cart is on its way. Pinching the nose allows formation of an airtight seal between the rescuer’s lips and the outside of the victim’s mouth. Successful rescue breathing (700-1000 mL Vt, 8-10 times per minute in an adult with a secured airway and a ratio of 30 compressions to 2 ventilations if the airway is unsecured) is confirmed by observing the chest rising and falling with each breath and hearing and feeling the escape of air during expiration. The most common cause of inadequate mouth-to-mouth ventilation is insufficient airway control. Mouth-to-mouth-and-nose breathing is more effective in infants and small children than in adults.
A rescuer’s exhaled air has an oxygen concentration of only 16-17% and contains significant CO2. Supplemental oxygen, preferably 100%, should always be used if available. If supplemental oxygen is used, a smaller VT of 400-700 mL is recommended.
Mouth-to-mask or barrier device breathing has a hygienic advantage over mouth-to-mouth breathing as the rescuer’s lips form a seal with an intervening device. Devices that avoid mouth-to-mouth contact should be immediately available everywhere in the hospital. Ventilation with a mask may be performed more easily in some patients because the rescuer may be able to adjust the airway or make an airtight seal more effectively. Furthermore, some mouth-to-mask devices allow the delivery of supplemental oxygen.