Cardiac anatomy and physiology
Knowing how to interpret an electrocardiogram (ECG) allows you to provide better patient care. For example, when caring for a patient with an arrhythmia or myocardial infarction, correctly interpreting an ECG can help you assess the patient’s condition and, when necessary, begin lifesaving measures. Having a clear understanding of cardiac anatomy and physiology is the first step toward developing these essential skills.
Cardiac anatomy
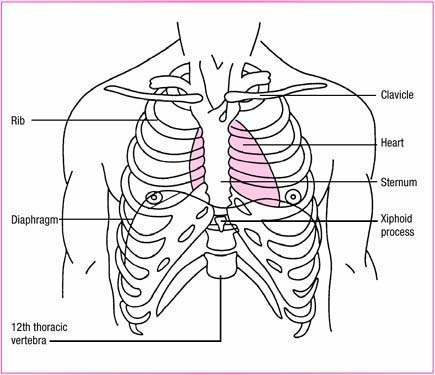
The heart is a hollow, muscular organ that lies obliquely in the chest behind the sternum in the mediastinum (the cavity between the lungs and in front of the spine). The top of the heart, called the base, lies just below the second rib. The bottom of the heart, called the apex, tilts forward and down toward the left side of the body and rests on the diaphragm. (See Where the heart lies, page 4.)
The heart varies in size, depending on the person’s body size, but is roughly 5″ (12 cm) long and 3½″ (9 cm) wide, or about the size of the person’s fist. The heart’s weight, typically 9 to 12 oz (255 to 340 g), varies depending on the person’s size, age, sex, and athletic conditioning. An athlete’s heart usually weighs more than average, whereas an elderly person’s heart weighs less. (See Changes in the heart, page 5.)
Heart wall
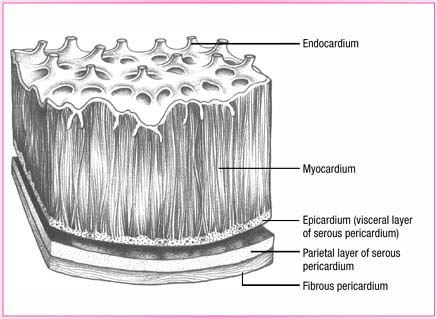
The heart wall contains three layers. The epicardium, the outermost layer, consists of squamous epithelial cells overlying connective tissue. The myocardium, the middle and thickest layer, forms the largest portion of the heart’s wall. This layer of muscle tissue
contracts with each heartbeat. The endocardium, the heart wall’s innermost layer, consists of a thin layer of endothelial tissue that lines the heart valves and chambers. (See Layers of the heart wall, page 6.)
contracts with each heartbeat. The endocardium, the heart wall’s innermost layer, consists of a thin layer of endothelial tissue that lines the heart valves and chambers. (See Layers of the heart wall, page 6.)
Enveloping the heart is the pericardium, a fluid-filled sac that acts as a tough, protective covering. It consists of the fibrous pericardium and the serous pericardium. The fibrous pericardium is composed of tough, white, fibrous tissue, which fits loosely around the heart and protects it. The serous pericardium, the thin, smooth, inner portion, has two layers:
the parietal layer, which lines the inside of the fibrous pericardium
the visceral layer, which adheres to the surface of the heart.
Heart chambers
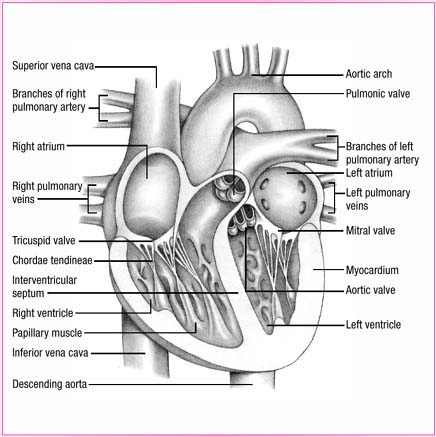
The heart contains four chambers—two atria and two ventricles. (See Inside a normal heart, page 7.) The right atrium lies in front of and to the right of the smaller but thicker-walled left atrium. The right and left atria serve as volume reservoirs for blood being sent into the ventricles. An interatrial septum separates the two chambers and helps them contract, forcing blood into the ventricles.
The right and left ventricles serve as the pumping chambers of the heart. The right ventricle lies behind the sternum and forms the largest part of the heart’s sternocostal surface and inferior border. The left ventricle forms the heart’s apex, most of its left border, and most of its posterior and diaphragmatic surfaces. The interventricular septum separates the ventricles and helps them pump.
Because the atria act as reservoirs for the ventricles and pump the blood a shorter distance, their walls are considerably thinner than the walls of the ventricles. Likewise, the left ventricle has a much thicker wall than the right ventricle because it works
harder, pumping blood against the higher pressures of the aorta.
harder, pumping blood against the higher pressures of the aorta.
Changes in the heart
The heart of the older adult
As a person ages, his heart usually becomes slightly smaller and loses its contractile strength and efficiency (although exceptions occur in people with hypertension or heart disease). By age 70, cardiac output at rest has diminished by about 30% to 35% in many people.
Irritable with age
As the myocardium of the aging heart becomes more irritable, extra systoles may occur, along with sinus arrhythmias and sinus bradycardias. In addition, increased fibrous tissue infiltrates the sinoatrial node and internodal atrial tracts, which may cause atrial fibrillation and flutter.
The heart of the child
The heart of an infant is positioned more horizontally in the chest cavity than an adult’s is. As a result, the apex is positioned at the fourth left intercostal space. Until age 4, the apical impulse is left of the midclavicular line. By age 7, the heart is located in the same position as an adult’s heart is.
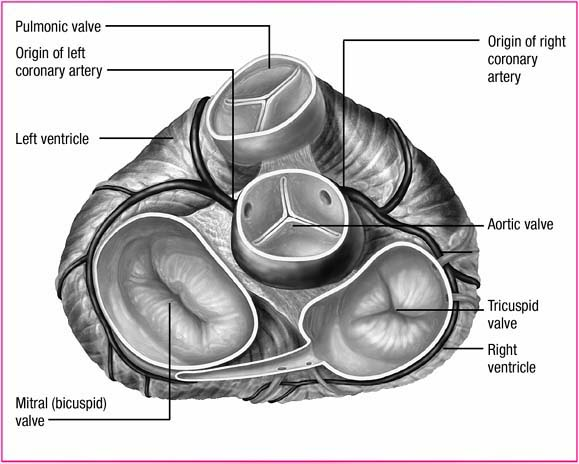
Heart valves
The heart contains four valves—two atrioventricular (AV) valves (tricuspid and mitral) and two semilunar valves (aortic and pulmonic) (See A view of the heart’s valves, page 8.) Each valve consists of cusps, or leaflets, that open and close in response to pressure changes within the chambers they connect. The primary function of the valves is to keep blood flowing through the heart in a forward direction. When the valves close, they prevent backflow, or regurgitation, of blood from one chamber to another. Closure of the valves is associated with heart sounds.
Atrioventricular valves
The two AV valves are located between the atria and ventricles. The tricuspid valve, named for its three cusps, separates the right atrium from the
right ventricle. The mitral valve, sometimes referred to as the bicuspid valve because of its two cusps, separates the left atrium from the left ventricle. Closure of the AV valves is associated with S1, or the first heart sound.
right ventricle. The mitral valve, sometimes referred to as the bicuspid valve because of its two cusps, separates the left atrium from the left ventricle. Closure of the AV valves is associated with S1, or the first heart sound.
The cusps, or leaflets, of these valves are anchored to the papillary muscles of the ventricles by small tendinous cords called chordae tendineae. The papillary muscles and chordae tendineae work together to prevent the cusps from bulging backward into the atria during ventricular contraction. Disruption of either of these structures may prevent complete valve closure, allowing blood to flow backward into the atria. This backward blood flow may cause a heart murmur.
Semilunar valves
The semilunar valves receive their name from their three cusps
that resemble half moons. The pulmonic valve, located where the pulmonary artery meets the right ventricle, permits blood to flow from the right ventricle to the pulmonary artery and prevents backflow into the right ventricle. The aortic valve, located where the left ventricle meets the aorta, allows blood to flow from the left ventricle to the aorta and prevents blood backflow into the left ventricle.
that resemble half moons. The pulmonic valve, located where the pulmonary artery meets the right ventricle, permits blood to flow from the right ventricle to the pulmonary artery and prevents backflow into the right ventricle. The aortic valve, located where the left ventricle meets the aorta, allows blood to flow from the left ventricle to the aorta and prevents blood backflow into the left ventricle.
Increased pressure within the ventricles during ventricular systole causes the pulmonic and aortic valves to open, allowing ejection of blood into the pulmonary and systemic circulation. Loss of pressure as the ventricular chambers empty causes the valves to close. Closure of the semilunar valves is associated with S2, or the second heart sound. (See Flow of blood through the heart.)
Flow of blood through the heart
| As shown in the illustrations below, blood follows a specific path as it flows through the heart. Keep in mind that right and left heart events occur simultaneously. The right atrium receives deoxygenated blood returning from the body through the inferior and superior venae cavae and from the heart through the coronary sinus. The left atrium receives oxygenated blood flowing from the lungs through the pulmonary veins. | The increasing volume of blood in the right atrium raises the pressure in the chamber above the pressure in the right ventricle. This increased pressure causes the tricuspid valve to open and blood flows to the right ventricle. Simultaneously, as the volume of blood in the left atrium increases, the pressure in the left atrium exceeds the pressure in the left ventricle. The mitral valve opens and blood flows into the left ventricle. | The right ventricle pumps blood through the pulmonic valve into the pulmonary arteries and then into the lungs. There, oxygen is picked up and excess carbon dioxide is released. The blood returns, oxygenated, to the left atrium, completing pulmonic circulation. The left ventricle pumps blood through the aortic valve into the aorta and then throughout the body. Deoxygenated blood returns to the right atrium, completing systemic circulation. |
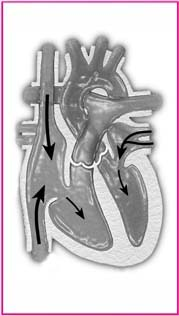 | 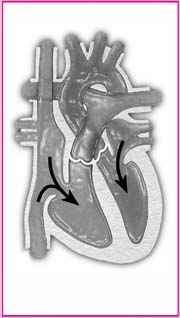 | 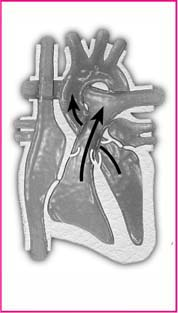 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree