Carcinoma of the Lung
Spiro Demetis MD, FCCP
Carcinoma arising from cellular elements of the tracheobronchial tree or lung parenchyma accounts for significant morbidity and mortality. The case fatality rate for lung cancer is one of the highest of all malignancies (greater than 90%), and lung cancer accounts for approximately 30% of all cancer deaths in the United States. The most important aspects of epidemiology, diagnosis, treatment, and prevention will be reviewed here.
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
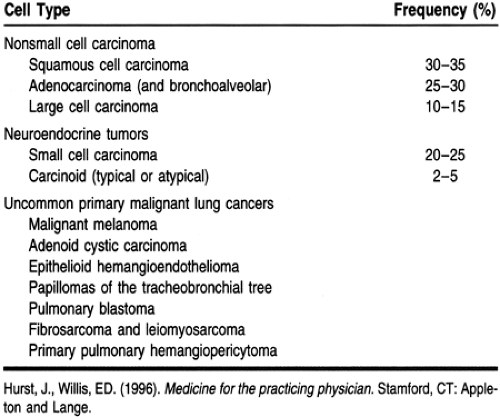
Bronchogenic carcinoma is so named because most lung cancers arise from the tracheobronchial tree. The histologic classification of lung cancer is shown in Table 73-1. The most important task for the pathologist when examining lung specimens is to differentiate between nonsmall cell lung carcinoma (NSCLC) and small cell lung carcinoma (SCLC). This is an important distinction: the staging and the recommended treatment are different for these cancers. NSCLC is more common than SCLC.
Squamous cell (epidermoid) carcinoma is the most common type of NSCLC, closely followed by adenocarcinoma. Squamous cell carcinomas arise from bronchial epithelial cells where squamous metaplasia is present. This cell type is most strongly associated with smoking. The histologic hallmarks of these tumors include keratin “onion pearls” and intercellular bridges. Because 65% of squamous cell cancers arise in the central airways, they present with chronic cough, hemoptysis, or obstructive atelectasis. Squamous cell carcinoma is most often associated with hypercalcemia. After complete resection, local recurrence is most common.
Adenocarcinomas, in contrast, tend to occur most often in the periphery of the lung rather than the central airway. They are more common in women. Tobacco use is a risk factor for this cancer, as is significant exposure to ionizing radiation (eg, mining of uranium). Adenocarcinomas are more likely to metastasize to extrapulmonary sites than are squamous cell cancers. After complete resection of an intrathoracic tumor, distal metastasis to the brain or bone is the most frequent pattern of recurrence. Because of their peripheral location, they are less likely to cause symptoms early in their development. A variable degree of glandular formation and positive staining with mucin carmine are the histologic hallmarks of adenocarcinomas.
Bronchoalveolar carcinoma is a subtype of adenocarcinoma that originates in the terminal bronchioles and extends into the alveolar spaces. The most common radiologic presentation is that of a pneumonic infiltrate. Sputum cytology is usually positive in this type of NSCLC.
SCLC and carcinoid tumors account for about 25% to 30% of all lung carcinomas. Similar to squamous cell cancers, they arise centrally and present clinically with cough, hemoptysis, and obstructive pneumonitis. These tumors have the potential to produce many humoral substances (eg, serotonin, somatostatin, vasoactive intestinal peptide, bombesin) and may produce several neuroendocrine syndromes. Carcinoid syndrome is rarely seen with bronchial carcinoid tumors (2% to 5% incidence).
EPIDEMIOLOGY
The incidence of lung cancer is highest in industrialized nations. The most important risk factor for the development of bronchogenic carcinoma is tobacco smoke. More than 90% of lung cancers in the United States are attributed to smoking; only 2% of lung cancers occur in nonsmokers. The risk for developing lung cancer is directly related to the number of cigarettes smoked daily, years of use, depth of inspiration, cigarette tar content, use of filterless cigarettes, and age of smoking onset. Although the risk for lung cancer is significantly reduced by smoking cessation, it never reaches that of lifelong nonsmokers (Sobue et al, 1991).
Although the data are conflicting, the odds ratio for developing lung cancer with prolonged and significant exposure to environmental tobacco smoke (passive smoking) is 1:34 (National Research Council, 1986). It is believed that 3000 to 5000 lung cancer deaths annually may be caused by exposure to environmental tobacco smoke.
Exposure to potential carcinogens in the workplace increases the risk for the development of lung cancer. Some of these carcinogens are ionizing radiation, asbestos, arsenic, vinyl chloride, nickel, and aromatic hydrocarbons. All of these can act as cocarcinogens with tobacco smoke, and the risk for lung cancer in exposed smokers is multiplicative. Radon produces alpha particles and is directly carcinogenic to the respiratory epithelium. It also acts as a cocarcinogen with tobacco smoke. All homes contain some radon; the concentrations are highest in the basement and lower floors. Lifelong residence in a home with a radon concentration of 8 pCi/L is estimated to result in a lifetime risk for a nonsmoker of about 1 in 100. Although this is controversial, some experts recommend taking remedial measures for homes that consistently test at greater than 4 pCi/L ambient air.
Chronic obstructive pulmonary disease and pulmonary fibrosis are pulmonary diseases that independently increase the risk for the development of bronchogenic carcinoma. Poor clearance of potential carcinogens is the probable mechanism in chronic obstructive lung disease. Persistent chronic inflammation in diseases leading to pulmonary fibrosis is likely to cause the increased incidence of bronchogenic carcinoma.
The overall incidence of lung cancer in the United States is 80 cases per 100,000 population. There are well-recognized racial, sex, and geographic differences. The incidence is higher in African Americans than in whites. One of the highest rates in the world is seen in African Americans living in the New Orleans area (107 cases per 100,000).
It is likely that the rates of lung cancer in men will plateau by the year 2000. This is mostly attributed to decreasing smoking trends in young white males. On the other hand, the incidence of lung cancer will continue to rise in women because of the considerable increase in tobacco use by females over the last three decades.
DIAGNOSTIC CRITERIA
The definitive diagnosis of lung carcinoma requires the identification of malignant cells in a cytologic specimen (sputum, lung washings, lung brushings, or pleural fluid) or the detection of areas of malignant transformation in a biopsy specimen from the lung parenchyma or bronchi. Lung cancer should be suspected in any patient presenting with a lung nodule or mass on chest x-ray, even in the absence of any symptoms, or when a pneumonia fails to resolve radiologically in 6 to 8 weeks after appropriate antibiotic therapy, especially in a patient with a history of tobacco use. Lung cancer should always be suspected in a smoker who presents with chronic cough, especially when complicated by hemoptysis, even if the chest x-ray is reported as normal.
HISTORY AND PHYSICAL EXAM
The clinical presentation of lung cancer is diverse and depends on the following:
Location of the primary tumor (central versus peripheral, and its relation to surrounding structures)
Presence of distant metastases
Presence of paraneoplastic syndromes or other coexisting diseases.
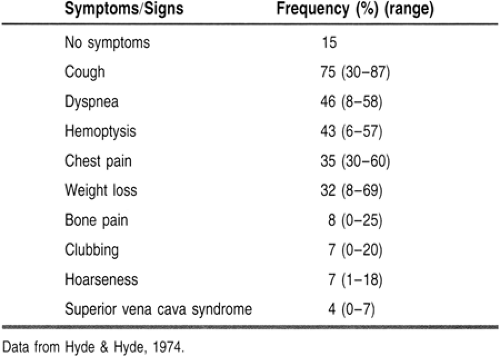
Although only 15% of lung cancer patients are asymptomatic at the time of diagnosis, the early symptoms are nonspecific and are often ignored for prolonged periods.
The signs and symptoms of lung cancer at the time of diagnosis are summarized in Table 73-2. Cough is by far the most common complaint, followed by dyspnea and hemoptysis. Central (endobronchial) lesions are more likely to be associated with cough early on, and ultimately may lead to hemoptysis. Hemoptysis, when present, is the most alarming symptom to patients, and they usually seek medical attention expeditiously. Critical narrowing of a bronchus by endobronchial tumor or by extrinsic compression may lead to all the symptoms associated with postobstructive pneumonitis (eg, fever, dyspnea, nonproductive cough). Significant weight loss is almost always reported at the time of diagnosis. Localized chest wall pain may be seen secondary to metastases to the thoracic skeletal structures (ribs, sternum, vertebral bodies), muscles, and skin.
The physical exam findings are variable and depend on the extent of intrathoracic spread and the presence and location of distant metastases. The lung exam may be completely normal, even when there is radiologic evidence of tumor. Centrally located (endobronchial) tumors are likely to cause symptoms earlier. The provider may appreciate decreased air entry to a particular lung segment or high-pitched inspiratory sounds over the involved bronchus. Large pleural effusions may also result in compressive atelectasis, along with all the expected physical exam findings (eg, decreased air entry, bronchial breathing, dullness to percussion). The presence of supraclavicular or cervical adenopathy is an important clinical finding and implies advanced inoperable disease.
The presence of significant jugular venous distention suggests involvement of the superior vena cava or pericardial carcinomatosis. All the signs of cardiac tamponade may be seen (eg, enlarged cardiac silhouette, narrow pulse pressure, low cardiac output state, metabolic acidosis), and they should prompt an urgent request for echocardiography, followed by pericardiocentesis or pericardial window. Funduscopic evidence of papilledema, even in the absence of symptoms, should lead to the performance of cranial computed tomography (CT) or magnetic resonance imaging (MRI) to rule out brain metastases. A variety of neurologic findings may be detected on the physical
exam, depending on the level of involvement and the presence of paraneoplastic syndromes.
exam, depending on the level of involvement and the presence of paraneoplastic syndromes.
Direct invasion of the brachial plexus, most often associated with apical or superior sulcus tumors, may result in Pancoast’s syndrome. This syndrome is characterized by referred pain to the scapula, shoulder, or arm (along with shoulder and upper extremity weakness) and Horner’s syndrome (ptosis, myosis, and hemifacial anhidrosis). Hoarseness of voice and dysphagia are ominous signs and indicate direct mediastinal spread by the tumor and advanced nonsurgical disease.
Superior vena cava syndrome may result from mediastinal invasion. Patients with this syndrome report headaches, facial fullness, and edema of the upper extremities. The cause of this syndrome is intraluminal thrombosis of the superior vena cava secondary to extrinsic compression by the tumor. Rarely, lung cancer presents with cardiac tamponade secondary to pericardial infiltration.
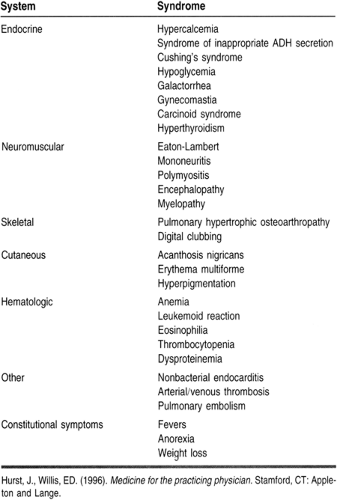
Not infrequently, the initial clinical manifestations of lung cancer may be secondary to metastatic disease or paraneoplastic syndromes associated with bronchogenic carcinoma. An exhaustive list of the paraneoplastic syndromes associated with bronchogenic carcinoma is provided in Table 73-3. Headaches, a variety of neurologic deficits, and seizures may be seen with intracranial or spinal cord metastases. Although metastases to the adrenals are common, the incidence of adrenal insufficiency is exceedingly rare. Liver metastases are also common and likewise do not frequently result in hepatic failure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree