
Blast Injuries
David W. Callaway and Leon D. Sanchez
During the period from 1996 to 2006 global terrorism-related bombings have increased fourfold with associated injuries increasing nearly eightfold (1). In the United States alone, there were over 36,000 explosion-related events and greater than 5,900 injuries from 1983 to 2002 (2). The extent of blast-related trauma is determined by a complex interaction of the physical components of the explosive device (e.g., size, explosive choice, delivery system, and adulterants), the environment (e.g., open versus confined space, distance from blast, reflecting surfaces, structural collapse, or medium in which the blast is transmitted), and intrinsic host factors such as age and comorbidities (3).
Conventional explosives are categorized as either high-order or low-order. High-order explosives (HE), such as TNT, Semtex, and dynamite produce a supersonic overpressure shock wave that results in rapid transient increases in ambient pressure (peak overpressure). This shock wave causes rapid external loading on the body, especially at points of air–tissue interface and is responsible for primary blast injuries (PBIs). High-order explosive detonations also result in secondary, tertiary, and quaternary blast injuries (Table 50.1). In contrast, low-order explosives (LE), such as pipe bombs and petroleum-based bombs result in subsonic explosions without resulting peak overpressure.
In HE detonations, the blast wave is composed of three components: the positive phase, the negative phase, and subsequent blast wind. During the positive phase, the blast wave expands radially at the speed of sound, causing a sudden increase in the ambient pressure (peak overpressure). This peak overpressure is responsible for PBIs. The biologic effect of the PBI depends directly on the level of peak overpressure and the duration of this positive phase. In the following negative phase, pressure drops below ambient levels, creating a vacuum and subsequent blast wind. The blast wind generates projectiles and can throw victims, resulting in secondary and tertiary blast injuries.
Blast wave propagation depends on the medium in which the explosion is detonated. As the shock wave expands, the overpressure decreases, and the velocity of propagation diminishes. In open air, the peak pressure of the shock wave falls off as the inverse of the distance from the explosion to the third power. In denser media, such as water, explosions produce shock waves that have a much higher peak overpressure and a faster rate of propagation than comparable explosions in air (1). The compressive shock wave results in greater blast loading on the victim and more severe injuries. The shock waves reflect off the surface of the water, creating tension waves that interact with the blast wave and diminish wave propagation. As a result, the overpressure effects increase with depth of submersion. Explosions within confined spaces are subject to reflection and magnification of the blast wave, leading to greater overpressure, longer positive phase duration, and an increased incidence of PBIs and death (Fig. 50.1).
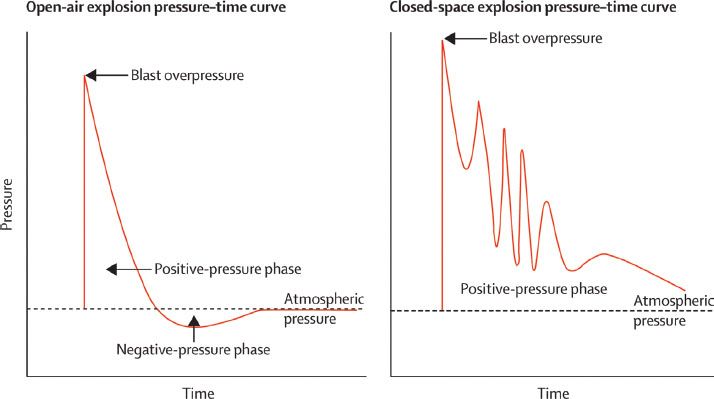
FIGURE 50.1 Difference in pressure curves between open- and closed spaces. (From Wolf SJ, Bebarta VS, Bonnett CJ, et al. Blast injuries. Lancet. 2009;374(9687):405–415.)
CLINICAL PRESENTATION
Blast injuries are classified into four categories: primary, secondary, tertiary, and quaternary (Table 50.1). PBI is unique to HE explosions. As the shock wave passes through biologic tissue, the injury is greatest at the interface between tissues of different densities, such as the lungs, the tympanic membrane (TM), and the bowel. The organ most vulnerable to PBI is the TM, followed by the lungs (4–8). The incidence of PBI in open space explosions is 10%, as compared to 38% in confined spaces (9). PBI is relatively uncommon in survivors of major explosive attacks. Many victims with PBI are very close to the source of the explosion and succumb to secondary and tertiary injuries prior to receiving medical care.
TABLE 50.1
Mechanisms of High-Order Explosive Blast Injury
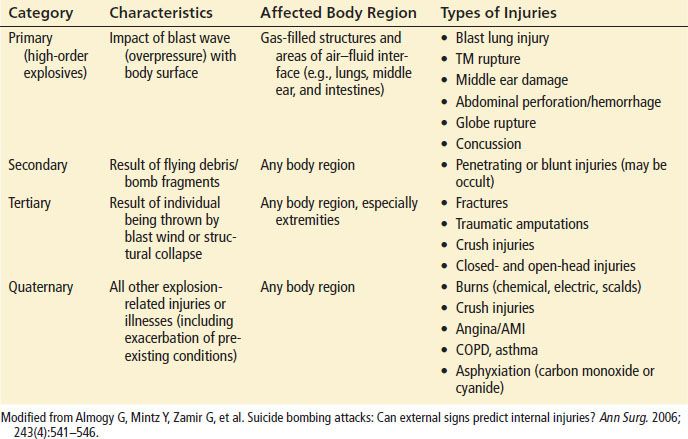
Secondary blast injury (SBI) predominates in victims presenting to emergency departments (EDs) (10). In SBI, the blast wave can propel objects, either intrinsic (e.g., shrapnel) or extrinsic (e.g., components of the target such as metal from a bus door) to the device that result in both blunt and penetrating trauma. The effective range of injury in SBI is greater than for PBI. Tertiary blast injuries are a result of the victims being thrown by the blast wind or by subsequent structural collapse. Quaternary blast injuries comprise a broad range of blast-related injuries that include burns, toxic inhalations (e.g., cyanide or carbon monoxide), asphyxiation, particulate inhalation, and exacerbation of pre-existing conditions. Quaternary blast injuries are common in industrial explosions.
An overwhelming majority (80% to 90%) of blast survivors present to the ED with non–life-threatening secondary, tertiary, and quaternary injuries (11,12). Soft tissue injuries (burns, abrasions, and embedded foreign bodies) are by far the most common injuries from terrorist bombings. Nine percent to 22% of victims will present with critical injuries (13). Studies of terrorist bombing incidents reveal that 50% of surviving casualties present to treatment facilities within the first hour (8,10). In general, there is a biphasic presentation, with more critically ill patients presenting in the “second wave” (8,11).
The TM is the structure most sensitive to peak overpressure and most commonly injured in blast victims, seen in up to 9% to 47% of blast survivors with significant injuries (14,15). Depending upon the orientation of the victim to the blast, increases in ambient pressure of 2 to 5 psi can result in rupture of the TM. The most common PBI is a linear tear in the inferior portion (pars tensa) of the TM. With increases in overpressure, the blast wave may also result in damage to the cochlea or ossicle dislocation (resulting in sensorineural hearing loss and tinnitus) (16). There is debate about the correlation between TM rupture and more life-threatening PBI. Isolated TM rupture does not appear to predict serious PBI reliably and with sufficient sensitivity (17,18,19). There is increasing evidence that suggests TM rupture as a predictor of significant concussive closed head injury.
The lung is the second most commonly affected organ in PBI. The threshold for lung damage is approximately 15 psi of peak overpressure, with moderate to severe lung damage observed with 50 psi (4). The advancing blast wave creates a pressure differential across the alveolar–capillary interface that results in damage to the lung parenchyma. Blast lung injury (BLI) is a unique injury defined by diffuse lung contusions, pulmonary edema, and occasionally pneumothorax or hemothorax. BLI is the most common fatal PBI among initial survivors.
The blast wave can also cause diffused parenchymal lacerations and can create fistulas between the alveolar spaces and the pulmonary veins. Venoalveolar fistulas allow air into the pulmonary venous system, which can then travel to the left side of the heart and enter the systemic circulation. Arterial air embolisms can result in sudden death, neurologic syndromes (e.g., cerebral or spinal infarction), and myocardial ischemia seen in some victims in the immediate postblast period.
Blast injury to the bowel requires higher peak overpressure and is more frequent in confined space or underwater blasts than in open-air explosions. The blast wave can cause serosal tears, intramural hemorrhages, or bowel perforation. Shear injuries to mesenteric vessels can cause ischemia or infarction that leads to delayed intestinal rupture. The colon (primarily the ileocecal region) is the visceral organ most frequently injured in PBIs. Solid organ damage is rare and directly related to proximity to the blast.
DIFFERENTIAL DIAGNOSIS
An accurate history of the timing, location, and proximity to the explosion is critical to the diagnosis and initial management of blast injuries. In patients with signs of respiratory distress, BLI should be suspected. The clinician should also consider cardiac contusions, reactive airway disease, acute myocardial infarction, toxic exposure (e.g., carbon monoxide or cyanide), or exacerbation of other underlying diseases. The differential diagnosis of shock in the blast victim must include BLI, hemorrhagic shock, spinal shock, ammonia nitrate exposure (explosive adulterant), acute myocardial infarction, and acute arterial embolism.
The etiology of altered mental status in the blast victim ranges from physiologic shock (e.g., hypovolemic, cardiogenic, or neurogenic) to closed head injury to psychogenic shock. Hearing loss may be from TM rupture, ossicle dislocation, foreign body impaction, or temporary stunning of the vestibular–cochlear system.
ED EVALUATION
Blast trauma does not occur in isolation. Emergency physicians must evaluate blast victims for blunt and penetrating trauma, blast-specific injuries, and exacerbations of chronic disease. The initial evaluation of the blast victim focuses on rapidly identifying life-threatening conditions and risk stratifying multiple patients.
One approach is to segregate patients based on the presence or absence of external signs of trauma. Patients in apparent distress or with signs of external trauma should be evaluated based on the ATLS Guidelines with secondary and tertiary examination focusing on ENT, ocular, and neurologic examination. Of note, the Injury Severity Score grossly underestimates the complexity of injury and the necessary resource utilization (9). In patients without apparent life-threatening injury, the main goal of initial evaluation is to identify PBI that may be obscured by secondary or tertiary wounds. The provider should obtain a focused history including location of blast (confined space or open air), distance of victim from blast, status of additional casualties, any details regarding the explosion (e.g., single suicide bomber, vehicle borne improvised explosive device, or presence of industrial chemicals, etc.). History should focus on symptoms concerning for PBI including chest pain, shortness of breath, cough, abdominal pain, tinnitus, or focal neurologic deficits. Concerning physical examination findings include tachypnea, hypoxia, decreased breath sounds, oropharyngeal pettechiae, chest wall crepitance, or abdominal tenderness. While absence of TM rupture does not preclude serious PBI, TM rupture should raise suspicion for more serious PBI and possible closed head injury (8,10). Any patient with a ruptured TM or with cardiopulmonary symptoms requires a chest radiograph to evaluate for BLI.
Routine laboratory testing is rarely useful in the management of PBIs. The arterial blood gas (ABG) is one exception. The ABG is particularly useful in the symptomatic patient, and oxygen desaturation may be the earliest sign of decompensation in the patient with BLI. The ABG may also assist with the diagnosis and management of toxic exposures to chemicals such as cyanide or carbon monoxide.
KEY TESTING
• Chest x-ray for suspected BLI
• ABG for suspected BLI









