FIGURE 25-1. Intravenous regional anesthesia: Injection of local anesthetic and placement of the tourniquet.
General Considerations
Intravenous regional anesthesia (IVRA) was first described in 1908 by the German surgeon A.G. Bier, hence the procedure name Bier block. Originally, anesthesia was obtained by the intravenous injection of procaine in a previously exsanguinated vascular space, isolated from the rest of the circulation by two Esmarch bandages used as tourniquets. After initial enthusiasm, the technique fell into obscurity for >50 years. In 1963, Holmes reintroduced the Bier block with the novel use of lidocaine, describing a series of 30 patients in The Lancet. Today, intravenous regional anesthesia of the upper limb remains popular because it is reliable, cost effective, safe, and simple to administer. It is a widely accepted technique well suited for brief minor surgeries such as wrist or hand ganglionectomy, carpal tunnel release, Dupuytren contractures, reduction of fractures, and others. Since the duration of anesthesia depends on the length of time the tourniquet is inflated, there is no need to use long-acting or more toxic agents. Its application for longer surgical procedures is precluded by the discomfort caused by the tourniquet, typically beginning within 30 to 45 minutes. Other disadvantages include incomplete muscle relaxation (where important) and lack of postoperative pain relief. With the implementation of a safety protocol and with meticulous attention to detail, concerns about local anesthetic (LA) toxicity should merely be a theoretical issue.
Anatomy
The only relevant anatomy is the location and distribution of peripheral veins in the extremity to be blocked. By preference, a vein as distal as possible is chosen. The antecubital fossa is an alternative only when more distal peripheral access is lacking.
Distribution of Anesthesia
The entire extremity below the level of the tourniquet is anesthetized. Numerous radiographic, radioisotope, and neurophysiologic studies looked into the site of action of IVRA. However, the exact mechanism still remains the subject of debate and controversy. The likely mechanism is that the local anesthetic, via the vascular bed, reaches both peripheral nerves and nerve trunks (vasae nervorum), and nerve endings (valveless venules). Diffusion of local anesthetic into the surrounding tissues also plays a role. Ischemia and compression of the peripheral nerves at the level of the inflated cuff is probably another contributory component of the mechanism of IVRA. Again, anesthesia achieved by intravenous regional anesthesia is limited only by the inevitable pain due to tourniquet application; and, therefore, it is used typically for procedures lasting 30 to 45 minutes.
Equipment
Equipment includes the following items (Figure 25-2):
FIGURE 25-2. Equipment for intravenous (IV) regional anesthesia consists of IV catheter, Esmarch, and local anesthetic.
• Local anesthetic agent: lidocaine HCl (0.25–2%)
• Rubber tourniquet
• IV catheters (18- or 20-gauge)
• 500-mL or 1-L bag of IV solution (crystalloid)
• Infusion set
• Pneumatic tourniquet, ideally with a double cuff
• One Esmarch bandage (about 150 cm in length, 10 cm in width)
• Syringes
Positioning and Preparation
The patient lies in the supine position with the vein selected for block placement readily accessible. Baseline vital signs are assessed; blood pressure, oxygen saturation, and ECG monitoring are applied. Intravenous access in the nonoperated extremity is obtained. Small doses of benzodiazepine for anxiolysis or small aliquots of opioids in case of discomfort, or both, may be administered. Adequate premedication will improve tourniquet tolerance and benzodiazepines can prevent the potential central nervous system signs of mild local anesthetic toxicity should the level of local anesthetic raise. An intact tourniquet system is essential for success and safety. Therefore, pneumatic cuffs always must be checked for air leaks before starting any IVRA procedure.
Technique
The technique consists of the following steps:
1. An IV cannula is inserted in the extremity opposite to the block side.
2. A double pneumatic tourniquet is placed on a padding layer of soft cloth (stockinette) with the proximal cuff high on the upper arm.
3. An IV cannula is inserted and carefully secured into a peripheral vein of the operative limb, as far distally as feasible. The cannula is flushed with saline before capping (Figure 25-3).
FIGURE 25-3. A small gauge intravenous catheter is inserted in the peripheral vein and secured.
4. The entire arm is elevated for 1 to 2 minutes to allow for passive exsanguination (Figure 25-4). After exanguination, while still keeping the arm high, a rubber Esmarch bandage is wrapped around the arm, spirally from the hand to the distal cuff of the double tourniquet, to exsanguinate the extremity completely (Figure 25-5).

FIGURE 25-4. A double well-padded tourniquet is placed on the upper arm. The arm is elevated to allow for passive exsanguinations.

FIGURE 25-5. With the arm elevated, an Esmarch bandage is systematically applied from the fingertips to the double tourniquet to help empty the venous bed.
5. While the axillary artery is digitally occluded, the proximal cuff is inflated to 50 to 100 mm Hg above systolic arterial blood pressure (Figure 25-6).
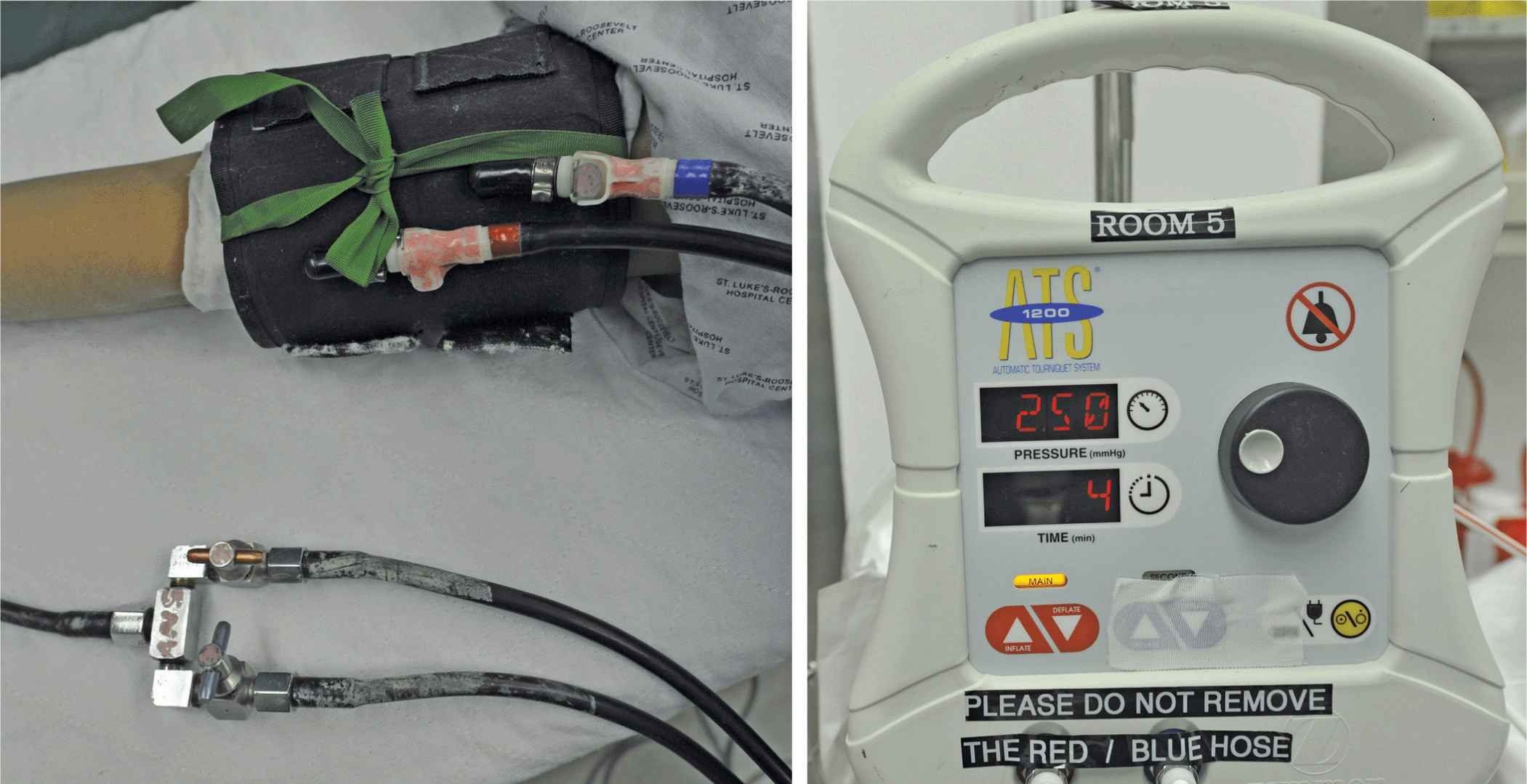
FIGURE 25-6. With the Esmarch in place, the double tourniquet is inflated in the following sequence: The distal cuff (red) is inflated first, followed by inflation of the proximal cuff (blue). Once the proximal cuff is inflated and checked for functionality, the distal cuff is deflated. The cuff pressure is determined by the patient’s systolic blood pressure; the cuff pressure should be about 100 mmHg above the arterial systolic blood pressure.
6. Sequence for initial tourniquet management:
a. Exsanguinate by elevation and Tourniquet wrapping
b. Inflate distal cuff
c. Inflate proximal cuff
d. Deflate distal cuff
7. Inject local anesthetic.
8. After reaching the correct pressure, the Esmarch bandage is removed and 12 to 15 mL of preservative-free 2% lidocaine HCl (or 30–50 mL of 0.5% lidocaine HCl) is slowly injected via the indwelling extra catheter (20 mL/min) (Figure 25-7). The volume depends on the size of the arm being anesthetized and the concentration of the anesthetic solution. Commonly recommended maximal dose is 3 mg/kg.

FIGURE 25-7. With the extremity exsanguinated and the proximal cuff inflated, local anesthetic is injected to anesthetize the extremity.
9. After the injection, the arm is lowered to the level of the table. The IV cannula from the anesthetized hand is removed, and in a sterile manner, pressure is quickly applied over the puncture site.
10. The onset of anesthesia is almost immediate after injection. When the tourniquet pain is reported by the patient, the distal cuff should be inflated and the proximal cuff deflated about 25 to 30 minutes after the beginning of anesthesia (Figure 25-8).

FIGURE 25-8. Management of the tourniquet pain. When the patient complains of tourniquet pain, the distal cuff (red) is inflated. Once the distal tourniquet is assured to be inflated and functional, the proximal tourniquet (blue) is deflated. All connectors must be clearly labeled (color coded in our practice) to avoid error in the sequence of inflation/deflation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








