Atrioventricular blocks
Atrioventricular (AV) heart block refers to an interruption or delay in the conduction of electrical impulses between the atria and the ventricles. The block can occur at the AV node, the bundle of His, or the bundle branches. When the site of the block is the bundle of His or the bundle branches, the block is referred to as infranodal AV block. AV block can be partial, where some or all of the P waves are conducted to the ventricle (first or second degree), or complete, where no P waves conduct to the ventricle (third degree).
The heart’s electrical impulses normally originate in the sinoatrial (SA) node, so when those impulses are blocked at the AV node, atrial rates are usually normal (60 to 100 beats/minute). The clinical significance of the block depends on the number of impulses completely blocked and the resulting ventricular rate. A slow ventricular rate can decrease cardiac output and cause symptoms such as light-headedness, hypotension, and confusion.
Various factors may lead to AV block. Typical causes include:
myocardial ischemia, which impairs cellular function and causes cells to conduct impulses slowly or inconsistently
myocardial infarction (MI)
excessive serum levels of, or an exaggerated response to, a drug (such as digoxin [Lanoxin], amiodarone [Cordarone], beta-adrenergic blockers, and calcium channel blockers), which may increase the refractory period of a portion of the conduction system
lesions along the conduction pathway
congenital anomalies that affect the conduction system (such as ventricular septal defects) as well as anomalies of the conduction system
inadvertent damage to the heart’s conduction system during cardiac surgery
inadvertent damage to the conduction system during radiofrequency ablation.
AV blocks are classified according to the site of the block and the severity of the conduction abnormality. The sites of AV block include the AV node, bundle of His, and bundle branches. Severity of AV block is classified in degrees: first-degree AV block; second-degree AV block, type I (Wenckebach or Mobitz I); second-degree AV block, type II (Mobitz II) AV block; and third-degree (complete) AV block. The classification system for AV blocks aids in the determination of the patient’s treatment and prognosis.
First-degree atrioventricular block
First-degree AV block occurs when the conduction of electrical impulses from the atria to the ventricles is delayed. This delay usually occurs at the level of the AV node, or bundle of His. After being delayed, the impulse is conducted through the normal conduction pathway.
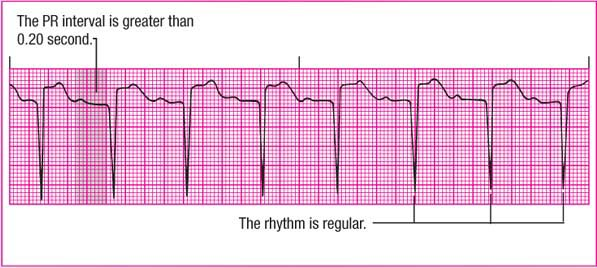
First-degree AV block is characterized by a PR interval greater than 0.20 second. This interval remains constant beat to beat.
Causes
First-degree AV block may result from myocardial ischemia or MI, myocarditis, hyperkalemia, rheumatic fever, or degenerative changes in the heart associated with aging. The condition may also result from the toxic effects of drugs, such as digoxin, calcium channel blockers, and beta-adrenergic blockers.
Clinical significance
First-degree block, the least dangerous type of AV block, indicates a delay in the conduction of electrical impulses through the normal conduction pathway. In general, a rhythm strip with this block looks like normal sinus rhythm except that the PR interval is longer than normal.
First-degree AV block may cause no symptoms in a healthy person. The arrhythmia may be transient, especially if it occurs secondary to drugs or ischemia early in the course of an MI.
Because first-degree AV block can progress to a more severe type of AV block, the patient’s cardiac rhythm should be monitored for changes. (See Recognizing first-degree AV block.)
ECG characteristics
Rhythm: Atrial and ventricular rhythms are regular.
Rate: Atrial and ventricular rates are the same and within normal limits.
P wave: Normal size and configuration; each P wave followed by a QRS complex.
PR interval: Prolonged (greater than 0.20 second) but constant.
QRS complex: Duration usually remains within normal limits if the conduction delay occurs in the AV node. If the QRS duration exceeds 0.12 second, the conduction delay may be in the His-Purkinje system.
T wave: Normal size and configuration unless the QRS complex is prolonged.
QT interval: Usually within normal limits.
Other: None.
Signs and symptoms
The patient’s pulse rate is usually normal and the rhythm is regular. Most patients with first- degree AV block are asymptomatic because cardiac output isn’t significantly affected. If the PR interval is extremely long, a longer interval between the first heart sound and the second heart
sound may be noted on cardiac auscultation.
sound may be noted on cardiac auscultation.
Interventions
Treatment generally focuses on identification and correction of the underlying cause. For example, if a drug is causing the AV block, the dosage may be reduced or the drug discontinued. Close monitoring can help detect progression of first-degree AV block to a more serious form of block.
Evaluate a patient with first-degree AV block for underlying causes that can be corrected, such as drugs or myocardial ischemia. Observe the ECG for progression of the block to a more severe form. Administer digoxin, calcium channel blockers, and beta-adrenergic blockers cautiously.
Type I second-degree AV block
Also called Wenckebach or Mobitz I block, type I second-degree AV block occurs when each successive impulse from the SA node is delayed slightly longer than the previous impulse. This pattern of progressive prolongation of the PR interval continues until an impulse fails to be conducted to the ventricles. (See Recognizing type I second-degree AV block.)
Usually, only a single impulse is blocked from reaching the ventricles. Following this nonconducted P wave or dropped beat, the pattern is repeated. This repetitive sequence of two or more consecutive beats followed by a dropped beat results in “group beating.” Type I second-degree AV block generally occurs at the level of the AV node.
Causes
Type I second-degree AV block commonly results from increased parasympathetic tone or the effects of certain drugs. Coronary artery disease (CAD), inferior-wall MI, and rheumatic fever may increase parasympathetic tone and result in the arrhythmia. It may also be caused by cardiac medications, such as beta-adrenergic blockers, digoxin, and calcium channel blockers.
Clinical significance
Type I second-degree AV block may occur normally in an otherwise healthy person. Almost always transient, this type of block usually resolves when the underlying condition is corrected. Although an asymptomatic patient with this block has a good prognosis, the block may progress to
a more serious form, especially if it occurs early in an MI.
a more serious form, especially if it occurs early in an MI.
Recognizing type I second-degree AV block
To help you recognize type I second-degree atrioventricular (AV) block, review this sample rhythm strip.
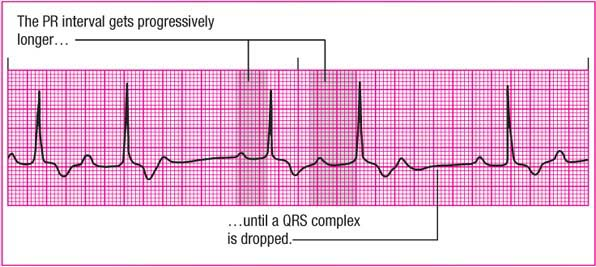 |
Rhythm: Atrial—regular; ventricular—irregular
Rate: Atrial—0 beats/minute; ventricular—50 beats/minute
P wave: Normal
PR interval: Progressively prolonged
QRS complex: 0.08 second
T wave: Normal
QT interval: 0.46 second
Other: Wenckebach pattern of grouped beats
ECG characteristics
When you’re trying to identify type I second-degree AV block, think of the phrase “long, longer, dropped,” which describes the progressively prolonged PR intervals and the missing QRS complexes. The QRS complexes are usually normal because the delays occur in the AV node. (See Rhythm strip patterns, page 184.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree