Asthma
Lawrence Glaubiger MD
Harry Pomeranz PA-C
Asthma is a chronic, persistent inflammatory disorder of the airway. It affects people of all ages and is characterized by exacerbations of coughing, wheezing, chest tightness, and difficulty breathing. Asthma is not a specific disease, but rather a syndrome that is triggered by precipitating factors such as allergens and results in reversible airway hyperresponsiveness and narrowing. Complex inflammatory events are responsible for both acute attacks and chronic disease.
New treatment strategies and pharmacologic therapies have developed as a result of an emerging understanding of the pathophysiology of asthma. However, despite an explosion of information concerning the inflammatory cells and mediators involved in asthma, morbidity and mortality rates are on the rise.
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
The human airway consists of a trachea and right and left mainstem bronchi, which divide into ever-narrowing and smaller branches. Nonstriated muscles and fibrous tissue surround the trachea and main bronchi, which are lined with ciliate epithelial cells. These cells remove mucus produced by goblet cells, lymphocytes, and neutrophils. Mast cells are the most important inflammatory cells, followed by helper T cells, eosinophils, and macrophages.
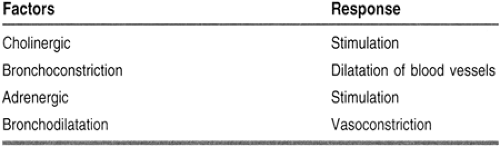
Cholinergic stimulation causes constriction of the bronchi, dilation of the local blood vessels, and increased mucus production. Adrenergic stimulation leads to bronchodilation, mucosal vasoconstriction, and increased ion secretion, resulting in increased ciliary rate and mucus clearance. Bronchodilation results from circulating catecholamines, such as epinephrine and glucocorticoids, which are affected by circadian rhythms, resulting in lower levels at night and early morning (Table 72-1).
The respiratory epithelium has an extensive network of beta-2 receptors that oppose bronchoconstriction. Stimulation of the beta receptors on the mast cells and other inflammatory cells stabilizes them and inhibits the release of inflammatory mediators.
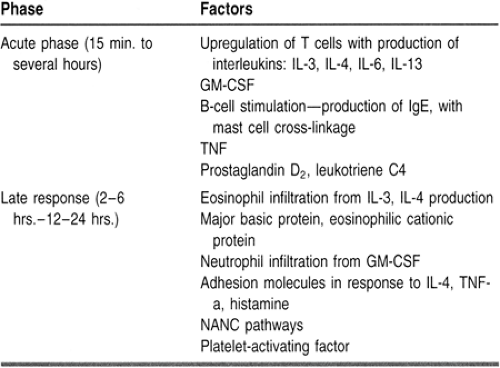
An asthma attack is made up of two phases, an acute phase response and a late phase response. The acute response begins within 5 to 15 minutes of the inciting event and lasts up to an hour. It begins with the interaction of an allergen and a macrophage. The late response occurs within 2 to 6 hours and lasts 12 to 24 hours. It is characterized by the increased infiltration of eosinophils and neutrophils. The sequence of events is summarized in Table 72-2.
Early in an asthma attack, there is increased minute ventilation, which causes hypocarbia. With tiring of the respiratory muscles, there is a reduction in minute ventilation, and hypocarbia is replaced by normocarbia. This should be a signal that the patient is progressing to respiratory failure and might require mechanical ventilation (Fig. 72-1).
Chronic Disease
After repeated attacks and chronic damage to the airways, there are certain classic findings in the biopsy of the bronchial mucosa. There is extensive epithelial cell damage and loss of ciliated mucosa and thickening of the basement membrane. Goblet cell hyperplasia is routinely seen. The bronchial wall is edematous as a result of vascular leakage from swollen and damaged endothelial cells. There is hyperplasia of the bronchial smooth muscle cells rather than hypertropy of the muscle fibers. All these chronic changes thicken the airway walls and narrow the airway diameter. The patient, instead of having only episodic symptoms, could become constantly symptomatic, as in other obstructive lung diseases.
EPIDEMIOLOGY
Asthma is estimated to affect 14 to 15 million persons in the United States, or about 5% of the population. It is the most common chronic disease of childhood, affecting an estimated 4.8 million children. It accounts for 5000 deaths a year. There are 470,000 hospitalizations annually from asthma. The National Health Interviews Survey reported an increase in those affected by asthma from 6.8 million to 10.3 million from 1980 to 1990. The rate for women increased by 50%, with African American women most affected (Asthma, United States, 1992).
In 1990, the cost of care for asthma was estimated at $6.2 billion, nearly 1% of the U.S. health care cost. Nearly half of that, 43%, was spent on emergency department treatment, hospitalization, and fatal asthma.
There are marked geographic differences in mortality rates, with especially high rates in four regions: New York City; Cook County, Illinois; Maricopa County, Arizona; and Fresno County, California. Twenty-one percent of all deaths from asthma occurred in New York City and Cook County, areas that account for only 6.8% of the population at risk. Both New York and Cook County had concentrations of extremely high incidence of asthma in small districts of impoverished inner-city neighborhoods (Weiss et al, 1992).
Race/ethnicity and socioeconomic status affect asthma prevalence but have a greater impact on hospitalization and
mortality rates. Race-specific hospitalization rates were similar when adjusted for income, suggesting that socioeconomic status is a greater risk for asthma morbidity than race alone.
mortality rates. Race-specific hospitalization rates were similar when adjusted for income, suggesting that socioeconomic status is a greater risk for asthma morbidity than race alone.
The physical environment of poor urban centers may also be a contributing factor. Housing in these neighborhoods tends to be deteriorated, with increased exposure to indoor air pollution, including irritant gases, and allergens such as mites, roaches, molds, and animals. Good nutrition is harder to maintain on a limited income, and lower education levels and poor support systems contribute to difficulty in maintaining good health. High-quality, ongoing health care may be difficult to find in underserved areas. Overburdened clinics and emergency departments can delay crucial treatment delivery in acute situations.
DIAGNOSTIC CRITERIA
Diagnosis is usually made clinically with a history of periodic wheezing, breathlessness, and chest tightness. However, asthma can present with just the symptom of cough. Symptoms that increase at night, or especially in the early morning hours, are characteristic of asthma.
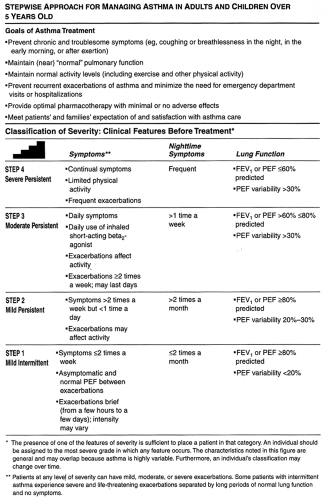
Classification of asthma is based on the severity of clinical symptoms and lung function, determined by peak expiratory flow (PEF) measurements. Peak flow meters are inexpensive and easy to use. Improvement or worsening of disease can be documented by having the patient keep a diary of PEF recordings. Nocturnal symptoms and diurnal variability are important in classifying asthma. A drop in PEF to less than 80% of personal best alerts the patient to an impending attack. A PEF of 50% of personal best requires the immediate attention of a health care provider (Table 73-3).
Lung function tests are a more objective method of diagnosing bronchial hyperactivity. Because of the variable nature of the disease, spirometry cannot be relied on for diagnosing asthma. An increase in the forced expiratory volume in 1 second (FEV1) of 12% or an increase in the forced vital capacity of 300 mL after the use of a beta-2 agonist suggests reversible airflow obstruction, which is seen in asthma.
Airway challenges have been used to make the diagnosis of bronchial hyperactivity. A bronchial provocation test can be done using methacholine or histamine. Doubling concentrations of the drug delivered to the patient from a nebulizer and the concentration which causes a 20% decrease in the initial FEV1 achieved before the challenge is called PC20. Studies using histamine have demonstrated that a PC20 of greater than 8 mg/mL made the diagnosis of bronchial hyperactivity and asthma unlikely. Studies of methacholine also used a similar concept in elucidating bronchial hyperactivity. Starting with 0.1 mg/mL of methacholine, the dose is doubled and the FEV1 is noted with each dose delivered. An FEV1 decrease below 80% of the FEV1 before administration is diagnostic of bronchial hyperactivity and suggestive of asthma if it occurs before or at a concentration of 25 mg/mL of methacholine.
Historically, asthma has been classified by the presence or absence of allergen exposure. Extrinsic asthma refers to symptoms that are triggered by an allergen. A positive skin test to the triggering inhalant and serum studies revealing an elevated IgE would confirm the diagnosis. This type of asthma usually begins in childhood. Intrinsic or nonallergic asthma has no recognizable allergic triggers, nor is there IgE elevation. Acute attacks tend to become more persistent and difficult to control than the extrinsic variety. Intrinsic asthma usually begins in adulthood.
HISTORY AND PHYSICAL EXAM
Factors and conditions known to trigger an asthma attack include:
Exercise: can trigger an attack within 5 to 20 minutes of onset. Exercise-induced asthma is more common in children and is often precipitated by exposure to cold air.
Drugs, particularly aspirin and other nonsteroidal anti-inflammatory medications: An association among aspirin-induced asthma, nasal polyps, and perennial rhinitis has been made.
Irritants such as sulfur dioxide and chemicals such as formaldehyde: Sensitive persons may also be affected by strong odors or perfumes.
Food additives, particularly metabisulfite, and certain dairy products: Some find this particularly troublesome after eating in restaurants that use monosodium glutamate (“Chinese restaurant syndrome”).
Premenstrual worsening of asthma: common, but usually of little clinical significance
Pregnancy: The effect on asthma is unpredictable. Some patients improve during pregnancy; others worsen.
Gastroesophageal reflux: an important trigger of bronchospasm. Acid reflux can cause a reflex vagal stimulation and bronchoconstriction. Concurrent esophageal pH monitoring with peak flow monitoring can determine this cause of asthma.
Cigarette smoking, including passive smoke inhalation
Household factors (eg, living in a damp house, use of gas for cooking, use of a humidifier)
Indoor environmental hazards (eg, silica, chemical fragrances [perfume, paint])
Occupational exposures can increase the prevalence of asthma within the general population. If the incidence of asthma within a particular workplace is several times that of the general population, an association can be made between the occupational environment and asthma. Some occupations in which this association has been made are:
Those who card or spin cotton
Animal handlers
Painters using polyurethane, which contains toluene diisocyanate
Bakers sensitive to cereals, flours, or grain contaminated by insects
Platinum refiners or those working with the industrial compound trimelitic anhydride
Pulp and paper workers, who are exposed to chlorine. Chlorine is an irritant gas and vapor that can cause new-onset asthma; this is referred to as reactive airways distress syndrome. Bleach plant workers are also exposed to chlorine.
Tin and lead solderers. Flux used in tin and lead soldering (colophony) is made of pine resins, a known allergen.
Printers using acacia and arabic gums, also made of tree resins. Those who work or live near Western red cedar and oak are also at risk.
Workers processing castor beans in the manufacture of castor bean oil.
Psychosocial factors have also been associated with asthma. Depression can increase the mortality rate from asthma, especially among children. Alcohol abuse, schizophrenia, recent unemployment, and family disruption or loss have also been associated with asthma deaths.
Screening for risk factors should include assessing how asthma is affecting the patient’s self-esteem and stress levels. The patient should be encouraged to elicit the reaction of family or friends to the disease and to develop coping mechanisms for physical and emotional stress.
The physical exam of the patient with chronic asthma focuses on the skin, airway, respiratory tract, and chest. Vital signs may show increased respiratory rate, tachycardia, and pulsus paradoxus (a difference of more than 10 mmHg in blood pressure between inspiration and expiration). Eczema on flexor surfaces or other signs of atopy should be noted, as well as the presence of rhinitis, sinusitis, or nasal polyps.
For some, the presence of an upper airway disease can influence the function of the lower airway. Allergic rhinitis or sinusitis may exacerbate asthma, or those with chronic, unremitting asthma may find an association with persistent sinusitis. At times of active allergic rhinitis, the use of topical corticosteroids for allergic rhinitis can decrease the intensity of the asthma symptoms.
Inspection of the chest may reveal signs of hyperinflation of the lungs, such as hunched shoulders or pigeon chest. Intercostal retractions or the use of accessory muscles indicates severe disease. The quality and intensity of breath sounds and the presence of wheezing, rales, or stridor are assessed on auscultation. Mild asthma might reveal wheezing only at end expiration. With increasing severity of disease, wheezing is heard throughout the respiratory cycle. Prolonged expiration or inspiration that equals expiration is also a sign of severe asthma. The absence of wheezing may be a sign of poor air movement and may signal danger and deterioration of the patient’s condition. The inability to speak in full sentences or a staccato pattern of speech may also indicate worsening disease.
CLINICAL WARNING
The absence of wheezing may signal a lack of air movement; this may be a danger sign.
DIAGNOSTIC TESTS
Baseline spirometry should be obtained, as well as serial PEF readings. Patients can determine which readings can be expected during symptomatic and asymptomatic periods, given their level of disease. Personal best levels should be known by both the patient and the provider. Complete pulmonary
function studies can show other causes of upper airway disorders that simulate asthma.
function studies can show other causes of upper airway disorders that simulate asthma.
A chest x-ray can rule out nonasthmatic causes of airway narrowing. A sputum stain may show eosinophilia, which is characteristic of asthma, or neutrophils, which are more common in bronchitis. Stains of nasal secretions can likewise reveal eosinophils, which are more suggestive of asthma, or neutrophils, which are more suggestive of sinusitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree