TOPICS
INTRODUCTION
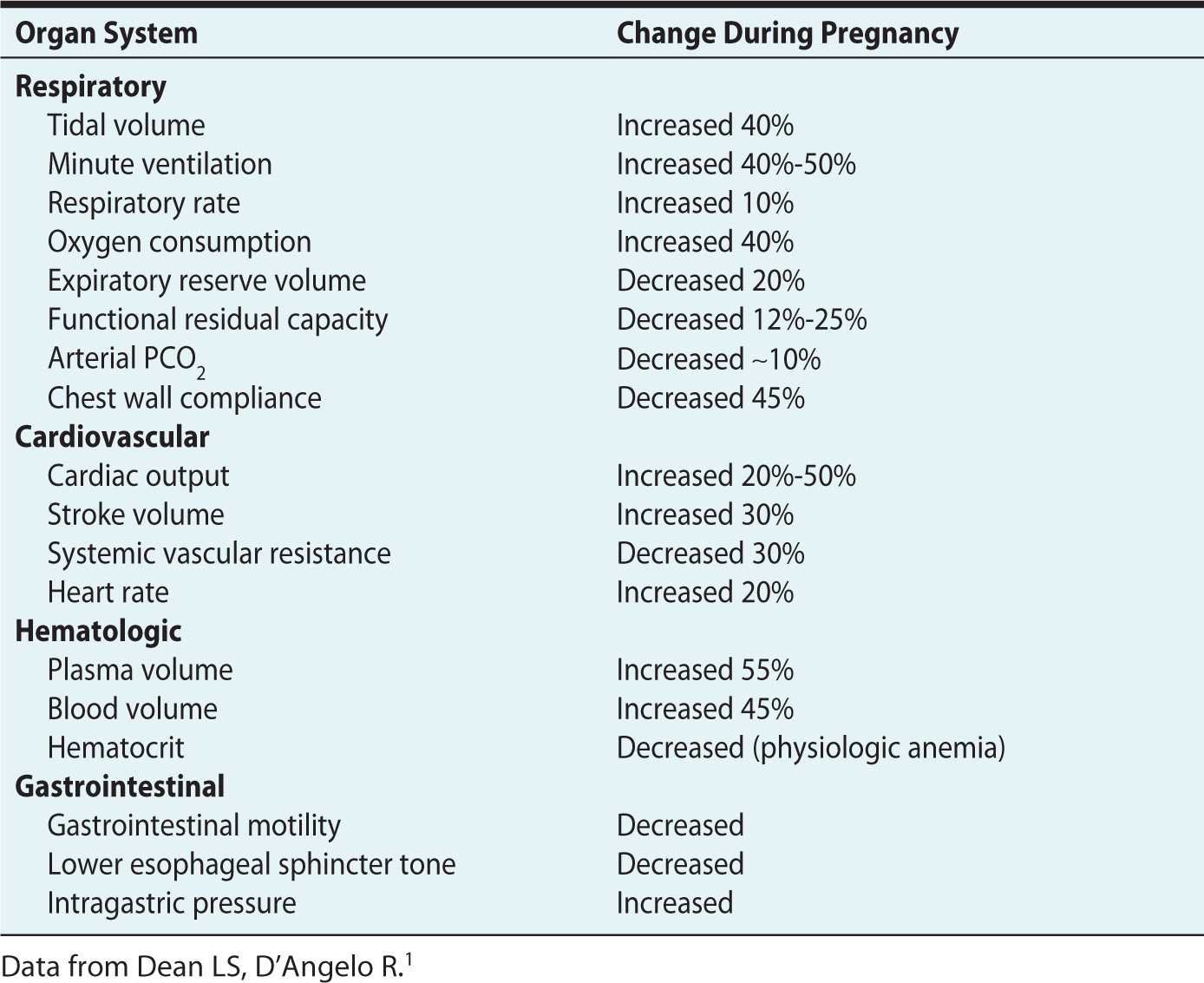
A majority of women experience subjective breathlessness during pregnancy. This complicates the diagnosis of true respiratory pathology. “Dyspnea of pregnancy” is likely related to normal physiologic alterations, summarized in Table 26-1, that serve to maintain the fetus and prepare the mother for labor and delivery.1 The dyspnea associated with pregnancy does not interfere with activities of daily living and is not related to exertion, coughing, or wheezing. Physiologic dyspnea usually improves as pregnancy progresses, particularly with “quickening,” which is defined as the maternal perception of initial fetal movement. In contrast, pathologic dyspnea from cardiac or pulmonary origins may have an abrupt onset, be progressive in its severity, occur even at rest, or be associated with cough, chest pain, fever, or hemoptysis. Dyspnea due to cardiac or respiratory pathology worsens as the pregnancy reaches the third trimester. Pregnant women with a respiratory rate greater than 20 breaths/min, increased work of breathing, or the presence of rales, wheezing, or murmurs deserve prompt evaluation for potential cardiopulmonary pathology.2
Table 26-1. Physiologic Changes During Pregnancy
ACUTE RESPIRATORY FAILURE
Epidemiology
Acute respiratory failure (ARF) is defined by the inability to maintain adequate oxygenation or ventilation. Although ARF is rare (occurring in less than 0.1% of pregnancies), it remains one of the most common indications for intensive care unit admission in pregnant women.3 The etiology of ARF in pregnancy is diverse and may or may not be directly related to pregnancy (Table 26-2). Acute respiratory distress syndrome (ARDS) has been defined by the American-European Consensus Conference with the following criteria: lung injury of an acute onset, bilateral infiltrates present on chest x-ray, PaO2-to-FiO2 ratio less than or equal to 200, and pulmonary artery wedge pressure less than 18 mm Hg or the absence of clinical evidence of left atrial hypertension.3 The estimated maternal mortality rate due to ARF is reported to be 30% to 35% and, in the setting of ARDS, regardless of the inciting etiology, the mortality rate can be as great as 70%.4 Fetal mortality is also high, most commonly reported at 20% to 30%, and it is usually due to complications from premature delivery or perinatal hypoxia.3
Table 26-2. Differential Diagnosis of Acute Respiratory Failure in Pregnancy
Pathophysiology
A respiratory insult during pregnancy may be more likely to lead to ARF. Increased oxygen consumption and decreased functional residual capacity (FRC) render pregnant women, particularly in the latter half of pregnancy, more susceptible to hypoxia, hypercarbia, and acidosis during short periods of apnea or hypoventilation. Chronic mild respiratory alkalosis during pregnancy helps promote elimination of fetal waste but limits buffering capacity during periods of maternal acidosis.3 Maternal mortality with ARF is found to be associated with low pH, initial loss of consciousness, which is probably related to hypoxia, disseminated intravascular syndrome (DIC), and sepsis.4
Management and Anesthetic Considerations
Obstetric patients admitted to the hospital with ARF should be followed closely in an intensive care unit. Some hospitals have obstetric critical care units to meet the special demands of caring for sick parturients and planning for delivery.
The primary management goals for patients with ARF include identification and treatment of the underlying cause of lung injury, optimizing adequate oxygen delivery, and maintaining fluid homeostasis. Additional goals include nutritional support, monitoring of fetal status, and planning for delivery.
Low alveolar closing pressure, due to a decreased FRC, increases the risk of alveolar collapse and atelectasis, especially in the supine position.3 Fetal hemoglobin has a higher affinity for oxygen than adult hemoglobin (see Figure 26-1). However, oxygenation needs of the fetus require higher maternal oxygen saturation compared to nonpregnant women. Maternal oxygen saturation greater than 90% and/or maternal PaO2 greater than 65 mm Hg are reasonable goals to ensure adequate fetal oxygenation.5,6 Hyperventilation should be avoided because hypocarbia can lead to uterine artery vasoconstriction, and alkalosis can diminish oxygen unloading to the fetus. Adequate oxygen delivery may be achieved by supplying higher inspired concentration of oxygen by face mask, noninvasive positive pressure ventilation, or by mechanical ventilation. Vigorous mechanical ventilation should be avoided because it can result in reduced placental perfusion as a result of low maternal cardiac output and venous return to the heart, augmented by aortocaval compression. Bronchodilator therapy and vasopressors might be useful adjuncts.7
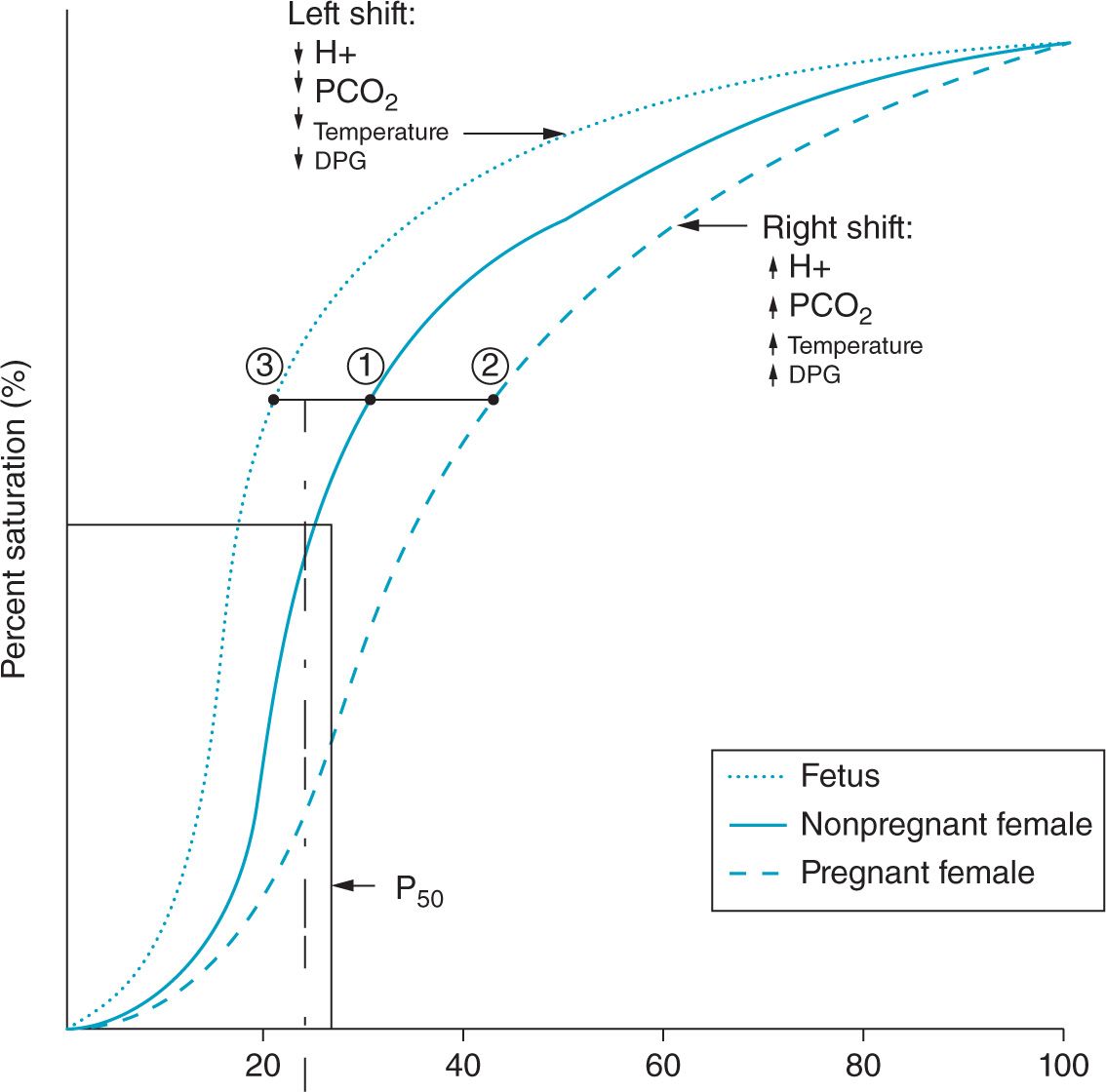
Figure 26-1. Theoretical oxyhemoglobin dissociation curves. Curve 1: Normal oxyhemoglobin dissociation curve in a nonpregnant adult. Curve 2: Oxyhemoglobin dissociation curve of a pregnant female at term gestation. Note that the curve is shifted to the right due to a 30% increase in erythrocyte 2,3–DPG to improve oxygen delivery to the fetus. Curve 3: Oxyhemoglobin dissociation curve of a fetus. Note that the curve is shifted to the left.
Goals of mechanical ventilation are to provide adequate oxygenation and to optimize ventilation with avoidance of barotrauma and increased transpulmonary pressure. Indications for intubation and mechanical ventilation for pregnant women are the same as for nonpregnant women and include the need for airway protection or failure to maintain adequate oxygenation and ventilation. Extra equipment and/or personnel should be available during endotracheal intubation in near-term pregnant women because of the potential for difficult airway management. Uterine displacement, either manually or with adequate pelvic tilt, is recommended to prevent aortocaval compression and improve preload in the supine position. Pregnant women should generally be considered as “full stomach aspiration risk” regardless of nothing-by-mouth status. Except in the most life-threatening emergencies, they should receive a nonparticulate antacid and a rapid-sequence induction with cricoid pressure. Preoxygenation is critical due to the potential to rapidly develop worsening hypoxia with apnea. Gentle manipulation of the upper airway is required during laryngoscopy to prevent trauma and bleeding, and a smaller endotracheal tube should be used because of a smaller glottic opening. A nasal airway should be avoided to prevent epistaxis.
Fetal monitoring, if appropriate for gestational age, should be performed, and a multidisciplinary plan for rapid delivery should be agreed on in the event of maternal or fetal deterioration. Cesarean delivery should be reserved primarily for obstetric indications, because optimizing the maternal cardiorespiratory status should promote fetal well-being and growth. Such delivery should be reserved for maternal indications or when the fetus is near term if labor and vaginal delivery are not attainable due to maternal condition.3,5
Extreme mechanical hyperventilation (end-tidal CO2 less than 24 mm Hg) may cause uterine vasoconstriction and a decrease in maternal cardiac output.1 Invasive hemodynamic monitoring, such as an arterial line or pulmonary artery catheter, may be required to optimize fluid homeostasis and thus prevent pulmonary edema while maintaining adequate organ perfusion. The head of the bed should also be elevated to decrease aspiration risk, and appropriate oral hygiene care should be performed to decrease nosocomial infections.3 Analgesia or even sedation may be necessary for maternal comfort and reduction of oxygen demands during positive pressure ventilation.3 The impact of maternal sedation on fetal heart tracings will need to be considered in making decisions about fetal health and indications for delivery. Prophylactic measures to prevent the development of deep venous thromboses is particularly important for pregnant or postpartum women due to their hypercoagulable state.1
PNEUMONIA
Epidemiology
Pneumonia complicates an estimated 0.4 to 2.7 per 1000 deliveries and is the most common cause of maternal mortality resulting from nonobstetric infection. The overall maternal mortality rate from pneumonia has improved to less than 4% over the past 50 years because of targeted treatment with more effective antibiotics and better critical care management.6,8 Community-acquired pneumonia (CAP) is a common but serious cause of hospital admission for hypoxia, fever, shortness of breath, cough, and pleuritic chest pain. Nonpregnant and pregnant women are susceptible to similar pathogens. The most common bacterial agents for CAP are Streptococcus pneumoniae and Haemophilus influenzae. Atypical agents such as Legionella species and Mycoplasma pneumoniae are seen rarely, and specific serologic testing for these organisms is usually not performed.5,8
Viral pathogens responsible for pneumonia in pregnancy include influenza A and B (including swine flu, H1N1 virus), varicella zoster virus, and coronavirus (severe acute respiratory syndrome). The novel H1N1 strain of the 2009-2010 influenza season created a historic epidemic that resulted in severe illness in pregnant women. Parturients infected with the H1N1 virus were at increased risk for complications, including hospitalization, respiratory failure, premature delivery, nonreassuring fetal status, and even death. Data collected by the Centers for Disease Control and Prevention (CDC) from August to December 2009 indicated an alarming 5% maternal mortality rate among 509 hospitalized pregnant women with H1N1.9 Regardless of H1N1, influenza during pregnancy in general has a high complication rate even during normal influenza seasons. For instance, parturients experience a near 10-fold increase in influenza-related morbidity as compared to nonpregnant women afflicted with the disease (10.5 versus 1.9 per 10,000 women).5 The CDC recommends that all pregnant women receive the influenza vaccine. Also recommended is the use of pneumococcal vaccine for high-risk parturients with chronic diseases, such as asplenia, immunocompromise, sickle cell disease, and so on.5
Etiology/Risk Factors
Women with asthma or anemia, which is defined as hematocrit less than or equal to 30%, also have a five-fold increase of developing pneumonia during pregnancy. Additionally, substance abuse, smoking, chronic medical conditions, preexisting pulmonary disease, and human immunodeficiency virus (HIV) infection are also associated with higher rates of pneumonia in pregnancy.10 The mode of delivery may also affect the incidence of pneumonia. For instance, during the postpartum period, women having a cesarean delivery have a greater incidence of pneumonia than those having a vaginal delivery.10
Pathophysiology
The physiologic changes that occur during pregnancy render parturients more susceptible to developing pneumonia. The decreased FRC and increased oxygen requirement associated with pregnancy compromise respiratory functions. Delayed gastric emptying, increased intragastric pressure, and a relaxed gastroesophageal sphincter predispose to aspiration. In addition, multiple immunologic changes occur that decrease the maternal immune response to infection.10 For instance, the activity of natural killer cells, helper T-type 1 cells, and T-cytotoxic 1 cells are reduced, thereby reducing the production of interleukin-2, interferon, and tumor necrosis factor.
Pneumonia may also be associated with several pregnancy-related complications. The incidence of preterm labor in women with CAP has been reported to be as high as 44%, and one-third of women may deliver prematurely.5,6,8–10 The incidence of premature rupture of membranes is increased in women with pneumonia as compared to those without pneumonia. In addition, women with pneumonia during pregnancy are nearly twice as likely to have intrauterine growth restriction with lower birth weights.5
Management and Anesthetic Considerations
Monotherapy with macrolides (erythromycin, azithromycin) is the mainstay of treatment in bacterial pneumonia and is successful in 99% of patients. In cases of drug-resistant Streptococcus pneumonia, ceftriaxone or cefotaxime should be added. Current CDC guidelines recommend that all pregnant women and women who are less than or equal to 2 weeks’ postpartum with documented exposure to the influenza virus or symptoms in the first 48 hours of illness should receive treatment with oseltamivir (Tamiflu) or zanamivir (Relenza) to reduce perinatal morbidity and mortality. Patients with varicella pneumonia had high mortality rate (35%-40%) before the introduction of antiviral therapy; with the advent of antiviral therapy, this is reduced to approximately 15%. These patients should be hospitalized early, and antiviral treatment with intravenous acyclovir should be initiated to reduce respiratory complications.6 As described in Table 26-3, American Thoracic Society guidelines can be adapted and applied during pregnancy with a 96% success rate at predicting a complicated pneumonia course requiring critical care support.5 Given the rapidity of complications that can occur, some obstetricians choose to hospitalize all pregnant women with pneumonia for overnight observation to complete a full workup, including chest x-ray, complete blood count, electrolyte panel, blood cultures if clinically warranted, and oxygen assessment of both the mother and fetus.6
Table 26-3. Possible Risk Factors for a Complicated Course of Community-Acquired Pneumonia During Pregnancya









