A delta and C fibers, under normal conditions, transmit nociceptive (pain) information to the spinal cord from their free nerve endings in the periphery. In chronic pain conditions, the A beta fibers, which normally transmit nonnoxious information, also participate in nociceptive transmission.
 Most randomized studies on the efficacy of epidural steroid injections show temporary relief of radicular pain. Studies on thermal rhizotomy of the medial branches, for relief of facet syndrome, show benefit that lasts 3 to 12 months. This relief avoids the usage of addicting opioids.
Most randomized studies on the efficacy of epidural steroid injections show temporary relief of radicular pain. Studies on thermal rhizotomy of the medial branches, for relief of facet syndrome, show benefit that lasts 3 to 12 months. This relief avoids the usage of addicting opioids.
 Injection of neuraxial local anesthetics and methylprednisolone, when performed 3 to 4 times during the acute stage of herpes zoster, may prevent the development of postherpetic neuralgia. Postherpetic neuralgia is mostly managed pharmacologically, although interventional techniques may be used in resistant cases.
Injection of neuraxial local anesthetics and methylprednisolone, when performed 3 to 4 times during the acute stage of herpes zoster, may prevent the development of postherpetic neuralgia. Postherpetic neuralgia is mostly managed pharmacologically, although interventional techniques may be used in resistant cases.
 Antidepressants are effective in neuropathic pain syndromes but their use is limited because of their side effects. The newer serotonin–norepinephrine reuptake inhibitors have properties that result in less drug interactions and improved efficacy.
Antidepressants are effective in neuropathic pain syndromes but their use is limited because of their side effects. The newer serotonin–norepinephrine reuptake inhibitors have properties that result in less drug interactions and improved efficacy.
 Anticonvulsants are effective in most neuropathic pain syndromes. Their favorable side effect profile and speed of therapeutic effect makes them the first line of treatment for these syndromes. Their efficacy is improved when combined with an opioid or an antidepressant.
Anticonvulsants are effective in most neuropathic pain syndromes. Their favorable side effect profile and speed of therapeutic effect makes them the first line of treatment for these syndromes. Their efficacy is improved when combined with an opioid or an antidepressant.
 Complex regional pain syndrome that does not respond to nerve blocks and physical therapy may respond to spinal cord stimulation.
Complex regional pain syndrome that does not respond to nerve blocks and physical therapy may respond to spinal cord stimulation.
 Opioids are the mainstay for cancer pain management and are effective in neuropathic pain although at higher doses.
Opioids are the mainstay for cancer pain management and are effective in neuropathic pain although at higher doses.
 The majority of pain secondary to cancer is effectively managed pharmacologically with opioids, anticonvulsants, and antidepressants. Neurolysis of the visceral sympathetic system for pain secondary to abdominal or pelvic cancer relieves pain, decreases opioid consumption, and improves the patients’ quality of life.
The majority of pain secondary to cancer is effectively managed pharmacologically with opioids, anticonvulsants, and antidepressants. Neurolysis of the visceral sympathetic system for pain secondary to abdominal or pelvic cancer relieves pain, decreases opioid consumption, and improves the patients’ quality of life.
 Vertebroplasty and kyphoplasty are indicated for vertebral compression fractures, although some newer studies question their efficacy.
Vertebroplasty and kyphoplasty are indicated for vertebral compression fractures, although some newer studies question their efficacy.
 Spinal cord stimulation is effective in patients with failed back syndrome, complex regional pain syndrome, angina, and critical limb ischemia.
Spinal cord stimulation is effective in patients with failed back syndrome, complex regional pain syndrome, angina, and critical limb ischemia.
 Intrathecal drug delivery systems are valuable options in patients in whom opioids are ineffective at high doses or cause unacceptable side effects.
Intrathecal drug delivery systems are valuable options in patients in whom opioids are ineffective at high doses or cause unacceptable side effects.
Multimedia
 Nociceptive Pathways
Nociceptive Pathways
 Pain Sensitization
Pain Sensitization
ANATOMY, PHYSIOLOGY, AND NEUROCHEMISTRY OF SOMATOSENSORY PAIN PROCESSING
Primary Afferents and Peripheral Stimulation
A variety of mechanical, thermal, electrical, or chemical stimuli can result in the sensation and perception of pain. Information about these painful or noxious stimuli is transmitted to higher brain centers by receptors and neurons that are often distinct from those that carry innocuous somatic sensory information. The mammalian somatosensory system is subserved by four groups of afferent fibers differentiated by their anatomy, rate of transmission, and sensory modality transduced (Table 57-1).
TABLE 57-1. PRIMARY AFFERENT FIBERS AND THEIR FUNCTION
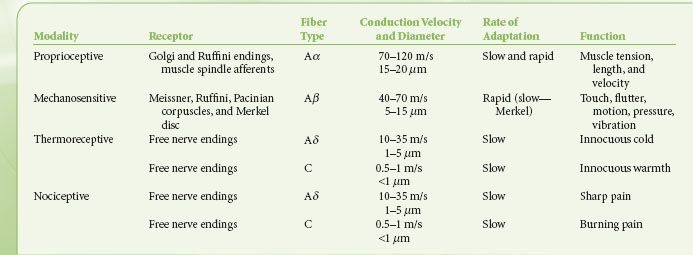
The first group, the heavily myelinated large-diameter A alpha (Aα) fibers, have specialized terminals incorporated within muscle spindles, Golgi tendon organs, and joints. These fibers and their respective end organs transduce proprioceptive information. The second group, the heavily myelinated large-diameter A beta (Aβ) fibers, have specialized encapsulated nerve endings including the Meissner, Pacinian, and Ruffini corpuscles and the Merkel disc, which transduce innocuous or low-threshold mechanical stimulation. Aα fibers do not ordinarily participate in signaling pain sensations to the central nervous system. However, the activation of Aβ and, possibly, Aα fibers has been invoked as a part of the mechanism for the production of pain relief by transcutaneous electrical nerve stimulators, which may implicate both fibers in a role in pain signal processing.1 As well, it is becoming increasingly apparent that in chronic pain states, these fibers may indeed participate in pain signaling by adopting a “phenotype” similar to that of a C fiber (vide infra).2
 The next groups of fibers represent the specialized sensory neurons that respond to actual or potential tissue damage, the nociceptors. The lightly myelinated medium-diameter A delta (Aδ ) fibers and the unmyelinated small-diameter C fibers have free nerve endings that transduce noxious or high-threshold thermal, mechanical, and chemical stimulation. Patients with a mutation of the tyrosine kinase protein A, which is a component of the nerve growth factor receptor, fail to develop Aβ, Aδ, or C fibers and have no ability to sense pain.3 Unlike receptors in the first two groups (Aα and Aβ), the Aδ and C fibers respond to stimulation of their receptive fields in a characteristic manner with slow adaptation and residual firing following the withdrawal of the stimulus. Although these two fiber groups respond similarly to stimulation, they mediate different aspects of pain sensation. The rapidly conducting Aδ fibers mediate the “first” pain or epicritic pain, which is well localized and is characterized as sharp or prickling. The slowly conducting C fibers mediate the “second” pain or protopathic pain, which temporally follows the epicritic pain and is poorly localized or diffuse and is characterized as burning or dull.4
The next groups of fibers represent the specialized sensory neurons that respond to actual or potential tissue damage, the nociceptors. The lightly myelinated medium-diameter A delta (Aδ ) fibers and the unmyelinated small-diameter C fibers have free nerve endings that transduce noxious or high-threshold thermal, mechanical, and chemical stimulation. Patients with a mutation of the tyrosine kinase protein A, which is a component of the nerve growth factor receptor, fail to develop Aβ, Aδ, or C fibers and have no ability to sense pain.3 Unlike receptors in the first two groups (Aα and Aβ), the Aδ and C fibers respond to stimulation of their receptive fields in a characteristic manner with slow adaptation and residual firing following the withdrawal of the stimulus. Although these two fiber groups respond similarly to stimulation, they mediate different aspects of pain sensation. The rapidly conducting Aδ fibers mediate the “first” pain or epicritic pain, which is well localized and is characterized as sharp or prickling. The slowly conducting C fibers mediate the “second” pain or protopathic pain, which temporally follows the epicritic pain and is poorly localized or diffuse and is characterized as burning or dull.4
The majority of Aδ and C nociceptors are polymodal and therefore are responsible for the transduction of noxious stimuli of different modalities. Nociceptive nerve endings are also located in muscle, the fascia, and adventitia of blood vessels, the knee joint, the dura, and the viscera. Recent evidence suggests that sensory transduction in the skin can include mediation by nonneural skin cells including keratinocytes and epithelial cells. These cells are thought to directly participate in touch and thermal sensation and are believed to communicate with the nerve ending through paracrine transmission.5 The keratinocytes and epithelial cells may also play a role in neuropathic and inflammatory pain conditions though the release of neuronal activating chemical mediator, or neurotransmitter, including calcitonin gene–related peptide (CGRP).6 Chemical mediators of pain are numerous. These mediators come from sources intrinsic to the neuron, including various neurotransmitters such as serotonin and substance P, and extrinsic to the nervous system, including substances from inflammatory/immune cells and red blood cells such as prostaglandins, kinins, cytokines, chemokines, and adenosine triphosphate that are released following injury to the tissue.
The primary afferent peripheral (distal) terminals express a variety of specific transducer channels that are sensitive over a range of stimulus intensities. When they are activated by the appropriate stimulus (thermal, chemical, or mechanical) these channels activate voltage-sensitive cation channels (NaV and CaV) and initiate an action potential. The sodium channel is of special interest following the discovery of its involvement in patients that are insensitive to pain. An epidemiologic study identified three Pakistani families with congential insensitivity to pain. All were found to possess nonsense mutations of the SCN9A gene resulting in truncation of the Nav1.7 isoform of the sodium channel.7 Other mutations of this gene result in the impaired inactivation of this channel resulting in paroxysmal extreme pain disorder or hyperexcitability resulting in erythromelalgia.8,9
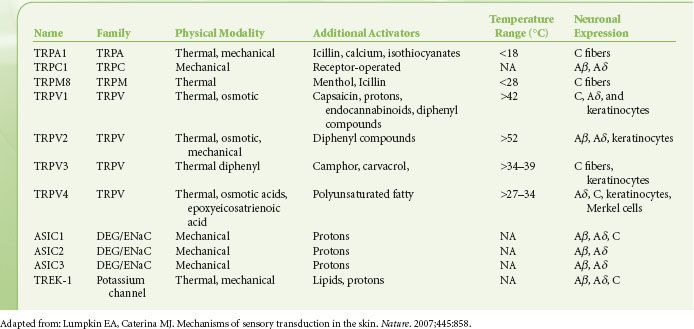
The understanding of the molecular underpinning of the sensory processing of pain has primarily come from studying two families of proteins, the TRP and the DEG/ENaC channels. The cloning and characterization of the “capsaicin” receptor of the transient receptor potential (TRP) family of nonselective cation channels expanded the field immensely10 (Table 57-2). Members of this molecular family transduce thermal, mechanical, and chemical information in the periphery. The capsaicin receptor named TRP vanilloid 1 (TRPV1), which responds not only to capsaicin and other vanilloid compounds, but which is also activated by acid and heat, provides an excellent example of the integration of multiple sensory modalities within a single neuron and is localized to nociceptors.10 Furthermore, acidic environments can lower the activation threshold of the channel to heat stimuli. Therefore, the TRPV1 receptor may represent an important therapeutic target in inflammatory (acidic) pain conditions. Mice lacking the TRPV1 receptor are deficient in their response to thermal, but not mechanical or other noxious stimuli.11 These data suggest that this member of the family of TRP channels may play a role in the integration of noxious chemical and thermal stimuli while having relatively less to do with mechanical transduction. Although mechanical transduction has been less well characterized than either thermal or chemical nociceptive transduction, there is evidence of mechanically activated channels in the degenerins family of the nematode Caenorhabditis elegans. In mammals, studies have provided evidence that the transduction channel is a complex of degenerin and the epithelial Na+ channel (DEG/ENaC)12 and may have a role in the transduction of mechanical stimuli in humans. The subunit composition of the DEG/ENaC channel may play a role in determining whether a mechanical stimuli is sensed as noxious or innocuous.13
TABLE 57-2. MECHANOSENSORY AND THERMOSENSORY TRANSDUCTION CHANNELS FOUND IN MAMMALS
Neurochemistry of Peripheral Nerve and the Dorsal Root Ganglion
The nociceptive primary afferents, the Aδ and C fibers, represent the principal target of pharmacologic manipulation by the physician treating pain. Glutamate receptors, as well as opioid, substance P, somatostatin, and vanilloid receptors, have been identified on the peripheral endings of these nerve fibers. Although the transmission of acute nociceptive information is primarily by the Aδ and C fibers, a subset of the Aδ and C fibers are “thermoreceptors” that transduce innocuous cold and warm information, respectively. The cell bodies of primary afferents, regardless of the structure they innervate, make up the dorsal root ganglia (DRG) located just outside the spinal cord within the bony foramen.
Primary afferent activation results in a postsynaptic excita- tory event in the spinal cord. Glutamate is the primary neurotransmitter serving this function. Acute activation events are mediated by the AMPA-type (α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid) glutamate receptor present on the dorsal horn neurons. This receptor produces a robust, but short-lasting depolarization of the postsynaptic membrane by increasing sodium conductance and augmenting the activation of the NMDA-type (N-methyl-D-aspartate) glutamate receptor. In addition to glutamate, populations of primary afferents contain and release a variety of neuropeptides including substance P, calcitonin gene–related peptide, adenosine triphosphate, adenosine, galanin, and somatostatin and growth factors including brain-derived nerve growth factor.14
Neurobiology of the Spinal Cord and Spinal Trigeminal Nucleus
Primary afferent fibers enter the gray matter of the spinal cord through the dorsal root entry zone and innervate the spinal cord. The majority of heavily myelinated primary afferent fibers (Aα, Aβ) carrying sensory information, including tactile, pressure, and vibratory sense, enter in dorsal roots, traverse across the top of the dorsal horn of the spinal cord (Lissauer’s tract), and ascend ipsilaterally within the dorsal column and provide collateral branches into the gray matter of the dorsal horn. The small-diameter lightly myelinated and the small-diameter unmyelinated fibers transmitting temperature and nociceptive information enter Lissauer’s tract and innervate the gray matter of the spinal cord. Unlike the heavily myelinated fibers, these fibers may also ascend rostrally or descend caudally through Lissauer’s tract before they innervate adjacent spinal levels.
The gray matter of the spinal cord is made up of synaptic terminations of primary afferents and the second-order neurons that form the first stage of processing and integration of sensory information. The gray matter of the spinal cord is divided into 10 laminae on the basis of histologic appearance. The dorsal horn includes laminae I to VI and represents the primary sensory complement of the spinal cord (Fig. 57-1). The ventral horn, including laminae VII to IX and lamina X, is involved in somatic motor and autonomic functions, respectively. Somatic C-fiber nociceptive afferent endings primarily terminate in the laminae I and II of the same and/or one to two adjacent spinal segments from which they entered from the periphery, whereas visceral C-fiber nociceptive afferents can terminate in the dorsal horn more than five segments rostrally or caudally. They not only terminate in laminae I, II, V, X ipsilaterally but also in laminae V and X contralaterally. Therefore, visceral afferents have a wider branching pattern and the nociceptive information they transmit is less localizable to a particular area of the body.
FIGURE 57-1. Anatomy: Histologic sections and schematic diagrams of the spinal dorsal horn. The histologic section at left is from the lumbar segment of the spinal cord. It is labeled to show the relationship between the major spinal somatosensory structures. The histologic section at right is from the rat lumbar spinal cord. The outer heavy lines show the boundary of the spinal gray matter while the inner heavy lines show the boundaries of Rexed’s laminae. These boundaries are established by the histologic characteristics of each zone, and the layers are identified by the Roman numerals. The drawing at the bottom illustrates the pattern of primary afferent innervation to the nonhuman primate spinal dorsal horn. The large myelinated (A-beta) fibers segregate to the dorsal aspect of an entering root and then track medially in the dorsal horn and terminate in layers III to V. The small myelinated (A-delta) fibers and C fibers that carry nociceptive information segregate ventrally in the entering roots, course laterally in the dorsal horn, and then largely terminate in the superficial layers (I and II) of the dorsal horn. (Adapted from: Raja SN, Dougherty PM. Anatomy and physiology of somatosensory and pain processing. In: Benzon HT, Raja SN, Molloy RE, Liu SS, Fishman SM, eds. Essentials of Pain Medicine and Regional Anesthesia. 2nd ed. Philadelphia, PA: Elsevier-Churchill Livingstone; 2005;3, with permission.)
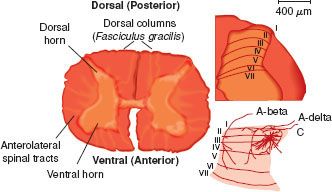
In addition to the primary afferent endings, neurons of the descending pathways and local interneurons also innervate the superficial dorsal horn (laminae I and II). The outer marginal layer or lamina I contain interneurons and cells that send axonal projections to the brainstem and midbrain structures. The substantia gelatinosa, or lamina II, also contains excitatory and inhibitory interneurons but fewer projection neurons. Laminae III and IV contain interneurons and the second-order neurons that make up the dorsal column pathways relaying nonnociceptive sensory and proprioceptive information. Laminae IV to VI contain interneurons and a modest portion of nociceptive projection neurons that distribute input to the brainstem and thalamus.
Nociceptive somatic input is primarily transmitted by second-order lamina I, IV, and V projection neurons as the contralateral spinothalamic tract (STT) pathway traveling to numerous brainstem regions and the thalamus.15 There is a nociceptive visceral processing area in laminae III, IV, V, VII, and X. The visceral nociceptive input is relayed by second-order neurons whose axons travel within the dorsal column. Like the fibers transmitting nonnoxious sensory information, these fibers remain uncrossed until relayed with the crossed medial lemniscal fibers to the thalamus. The visceral pain information transmitted by the ventral STT is likely originating from cells also receiving somatic nociceptive input. Nociceptive and nonnociceptive sensory information from the head, neck, and dura transmitted via the trigeminal nerve innervates the dorsal horn of the spinal trigeminal nucleus in the caudal medulla. The organization and neurotransmitter complement of the spinal trigeminal nucleus is similar to that of the spinal dorsal horn.
Neurobiology of Ascending Pathways
Dorsal Column Tracts
The dorsal column contains the axons of second-order spinal cord projection neurons in addition to the ascending axons of primary afferent neurons relaying touch, pressure, and vibratory sensation. Second-order dorsal column cells in the central visceral processing region of the spinal cord around lamina X also respond to noxious visceral stimulation and converge on some of the thalamic cells receiving nociceptive information from the skin and other somatic structures.
Spinothalamic Tract (STT)
STT neurons are the primary relay cells providing nociceptive input from the spinal cord to supraspinal levels. The axons of STT cells cross the midline of the spinal cord through the anterior white commissure and ascend primarily in the contralateral and anterolateral tracts. The axons of STT cells terminate primarily in the posterior complex of the thalamus including the ventral posterior lateral and ventral posterior medial nuclei. Nonnoxious sensory input from the same body region converges on the same target thalamic neurons providing somatotopic encoding for localization of the input onto the cortical representation of the specific body region, allowing the ability to locate the source of the nociceptive input. The STT cells receiving noxious somatic input are predominantly situated in lamina I and the lateral aspect of the dorsal horn in laminae IV to V.15 However, other STT neurons are scattered throughout the deep dorsal horn, intermediate region including lamina X, and even in lamina VII of the ventral horn. These STT cells receive both somatic and visceral nociceptive information.
Spinobulbar Pathways
Major ascending lateral axonal projections relaying information about noxious stimuli terminate in the reticular formation of the ventrolateral medulla. This spinal projection pathway traverses brainstem regions containing catecholaminergic neurons, including the locus coeruleus and A7 nuclei of the dorsolateral pontine tegmentum (DLPT). These catecholaminergic neurons are involved in multiple functions, including modulation of nociceptive transmission through the spinal cord via descending inhibitory input. Connections between the rostral ventromedial medulla (RVM) and the catecholamine cells of the pons and brainstem serotonergic cells also play a role in descending modulation of noxious transmission in the spinal cord.16 Spinobulbar pathways relaying information about pain also terminate in the parabrachial nucleus, periaqueductal gray (PAG), the RVM, and midline midbrain reticular formation.17
Spinohypothalamic, Limbic, and Cortical Connections
Pain is a sensory experience but also has an affective component to the perception of noxious stimuli. Pain can provoke fear, anxiety, and depression, resulting in autonomic responses including increased heart rate and blood pressure as well as the endocrine stress response. These responses to noxious stimuli are thought to be mediated by the spinohypothalamic and spinoamygdalar pathways. In addition to their affective function, these regions are also thought to be involved in antinociception. Ascending axonal projections of these pathways arise predominantly from the spinal cord laminae I and X.
Neurobiology of Descending Pathways
The primary components of this descending pain inhibition system, but certainly not all-inclusive, is the “triad” of the PAG, the RVM, and the DLPT.17 The PAG is an important site for the production of antinociception following electrical or chemical activation, or the injection of opioid receptor agonists. The endogenous opioid enkephalin is present within this nucleus, and opioid receptors of each subtype are present in this region. The PAG provides dense projections to the RVM, the locus coeruleus, and A7 nuclei.18 Although each of these regions has direct projections to the spinal cord, it has been proposed that their projections to the RVM are important components in the modulation of nociception. Chemical or electrical inactivation of the RVM results in the attenuation of the antinociceptive effects produced by the activation of these midbrain structures.19 Although the RVM can function as a relay nucleus in the production of antinociception by more cephalad midbrain structures including the PAG, it also has a primary role in the suppression of nociceptive transmission at the level of the spinal cord. The suppression of nociceptive reflex behavior is mediated by the axons of RVM neurons that descend within the dorsolateral funiculus and terminate bilaterally in laminae I, II, V, VI, and VII of the spinal cord. Anatomic studies have shown that these axons terminate coincident with interneurons of the dorsal horn that are related to nociceptive transmission.20 Consistent with the anatomic terminations of the RVM axons, physiologic studies have shown that stimulation of the RVM results in the inhibition of a population of nociceptive-specific neurons within the dorsal horn as well as selective inhibition of the nociceptive responses of wide-dynamic range neurons.21 The neurotransmitters found in the RVM neurons include enkephalin, γ-aminobutyric acid (GABA), glutamate, and substance P.22 The DLPT is also an important component of spinal cord nociceptive modulation. It contains all of the noradrenergic neurons that project to the RVM and the spinal cord, and electrical stimulation of the DLPT sites produces spinal cord α2-adrenergic receptor–mediated analgesia.23
Neurobiology of Supraspinal Structures Involved in Higher Cortical Processing
Higher cortical centers play a role in the perception of painful stimuli as well as the integration of the sensory-discriminative and affective components of the noxious stimulation. The localization of the neural structures involved in this perception and integration is still in its adolescence. The development of positron emission tomography and functional magnetic resonance imaging technologies has moved this research forward. These imaging technologies produce indirect evidence of neural activity related to pain stimulation. They look for areas of increased blood flow as an indicator of regions of increased activity resulting from the stimulation. The primary and secondary somatosensory cortexes, the anterior cingulate gyrus, the insula, and the prefrontal cortex appear to be involved in the higher processing of somatic and visceral pain.24 As the primary and secondary cortexes are known to be somatosensory processing regions, the imaging studies are consistent with a sensory-discriminative role of these structures. The insula and frontal cortex may contribute to memory and learning of events related to painful stimuli. The anterior cingulate cortex is thought to be involved in the analysis of the emotional significance of the painful input. Finally, the lentiform nucleus and cerebellum may be involved in the learning of self-protective reflexive motor responsiveness to painful input.
Transition from Acute to Persistent or Chronic Nociception
Pain sensation is unique among the somatosensory modalities in that it does not rapidly adapt to prolonged stimulation as do the other sensory modalities, such as fine touch. In fact, continued stimulation may produce greater noxious sensation or reduce the stimulus threshold or intensity that is necessary for the appreciation of the sensation as noxious. For instance, previously innocuous thermal or mechanical stimulation may be perceived as painful following a prior noxious stimulus. For example, warm water of the shower or the light touch of the towel across sunburned skin produces a painful sensation that may persist for a few minutes following the stimulation. This is termed allodynia. Another example of an altered pain state that may follow an acute injury is that of hyperalgesia, in which a previously noxious stimulus is perceived as more painful. The sensation of increased intensity of noxious stimulation at the site of the injury is the result of the sensitization of the peripheral nociceptors.
Persistent C fiber, but not Aβ fiber, primary afferent activation of lamina I and lamina V, as occurs with tissue injury and inflammation, has been shown to enhance the response to subsequent stimulation and augment the size of the receptive field of the respective dorsal horn neuron. Therefore, afferent input from adjacent dermatomal areas now produces neuronal excitation. Furthermore, nonnoxious stimulation becomes increasingly able to activate these neurons. This general phenomenon has come to be termed wind-up or central sensitization.25 It is these physiologic effects that are believed to underlie the allodynia and hyperalgesia produced by persistent noxious stimulation or tissue injury. This persistent input will lead to cellular damage and migration of inflammatory cells including macrophages and neutrophils into the peripheral tissue. This leads to the release of histamine, bradykinin, prostaglandins, cytokines, growth factors, protons, and peptides that activate or sensitize receptors on the peripheral nociceptor. Activation of these receptors results in depolarization and, under these conditions, spontaneous afferent activity. This activation is thought to explain the allodynia and hyperalgesia observed surrounding the site of injury.
In addition to the alteration of the chemical milieu surrounding the primary afferent distal terminal that results from injury or persistent high-intensity stimulation, axonal sprouting and the formation of neuroma may occur. The neuroma may have an altered complement of ion channels including an up-regulation of sodium channels or a down-regulation of potassium channels that has the net result of increasing neuronal excitability and increasing nociceptive transmission. It has been shown that, following nerve damage, an increase in the expression of sodium channels occurs in the neuroma and the DRG. Numerous sodium channels exist on primary afferents; Nav1.8 and 1.9 subtypes are primarily found on C-fiber DRG cells. Genetic “knock-down” or removal of the Nav1.8 channel had no effect on baseline pain thresholds; however, it reversed nerve injury evoked nociception.26 Also following nerve damage, potassium currents have been shown to be reduced, suggesting a reduction in these channels contributing to spontaneous nociceptive activity. Consistent with this notion, it has been observed that potassium channel antagonists increase and potassium channel agonists decrease ectopic firing after peripheral nerve injury.27 The HCN2 ion channel which carries an inward current Ih that is activated by neuronal hyperpolarization may have a significant role in the sensation of chronic pain from neuropathy or inflammation.28 When this gene product was knocked out of nociceptive primary sensory neurons in mice, the mice failed to express pain behaviors after inflammatory injuries. The mice did not show hyperalgesia or allodynia to mechanical or thermal stimuli in a model of neuropathic injury. The pharmacologic blockade of this channel, or disruption of this gene, could be a potential therapy for those suffering from some conditions of chronic pain.
Neuromas of injured primary afferents have altered sensitivity to a number of humoral factors, including cytokines, prostaglandins, and catecholamines. These factors are released from a variety of cell types including inflammatory cells and neuronal support cells. Cytokines directly activate the nerve and neuroma through receptors that become expressed in the membrane after the nerve injury. A molecule that has been shown to have a prominent role following nerve damage is tumor necrosis factor subunit alpha (TNF-α).29 Shortly after injury, TNF-α decreases potassium conductance, increasing neuronal excitability, while the long-term changes may be produced through the activation of second messenger systems, resulting in altered protein production. Application of TNF-α to the peripheral nerve results in hyperalgesia, while systemic delivery of antibodies to TNF-α or TNF-α–binding protein reduces neuropathic pain.
Prostaglandins are also released from inflammatory cells following nerve and tissue damage. They can enhance the opening of Nav1.8 channels by acting though receptors on the afferent terminal. Nerve growth factor is also released from glial and inflammatory cells after nerve damage, resulting in sprouting of postganglionic sympathetic efferents into the site of injury. Protease-activated receptors isoforms 1, 2, and 4 appear to sensitize TRPV1 channels in nociceptive neurons and are involved in mechanisms of pain and inflammation.30 These receptors are responsive to thrombin activation and could account for pain resulting from a hematoma. The up-regulation of α1-adrenergic receptors has been demonstrated in animals with nerve injuries.31 Stimulation of the postganglionic axons results in the release of catecholamines and excites the injured axon and DRG of the injured axon via α-adrenergic receptors.
Although acute noxious stimuli are transmitted to the spinal cord via Aδ and C fibers, the presence of allodynia is thought to be mediated by the activation of large-diameter Aβ fibers through what has been termed a phenotypic switch.2 Prior to this peripheral injury, the Aβ fibers, unlike the C fibers, do not express substance P. However, following injury these fibers were able to express this neuropeptide.32 These data therefore implicate Aβ fibers in the transmission of noxious peripheral stimulation and provide further support for the involvement of somatic Aβ fibers in at least some form of the allodynic pain states. Furthermore, the blockade of Aβ fibers results in a reduction in light-touch evoked allodynia.33 This phenotypic switch of Aβ fibers may represent another avenue for therapeutic intervention; however, the difficulty will be in differentiating between those Aβ fibers involved in noxious versus nonnoxious sensory information.
MANAGEMENT OF COMMON PAIN SYNDROMES
Low Back Pain: Radicular Pain Syndromes
The common causes of low back pain include radicular pain/radiculopathy from herniated disc or spinal/foraminal stenosis, facet syndrome, and internal disc disruption. Myofascial pain syndrome also causes back pain, whereas sacroiliac joint syndrome and piriformis syndrome cause mostly buttock pain but can present as low back pain or radicular pain. Radicular symptoms of pain, paresthesias, and numbness in a typical dermatomal distribution in the presence of objective signs of weakness, diminished reflexes, and positive straight-leg raise are secondary to pathology or dysfunction of the sensory spinal nerve roots. Low back pain, with or without radicular pain, is mostly due to lesions of the intervertebral discs and degenerative spinal disorders. Other causes include spinal metastasis, vertebral body fractures, infections, abdominal aortic aneurysm, and chronic pancreatic lesions.
Low back and radicular pain secondary to a herniated disc is due to mechanical nerve root compression and the subsequent inflammatory process. The presence of a herniated disc does not necessarily result in pain. Up to 36% of the general population34 and up to 53% of pregnant women35 can have an asymptomatic herniated disc. Follow-up studies on patients with a herniated disc show spontaneous regression without treatment, absence of symptoms in the presence of more abnormalities, and partial or complete resolution with treatment that includes medications, bed rest, physical therapy, traction, or epidural steroids.36 If symptomatic, the patient usually presents with low back pain and radicular symptoms that include paresthesias as well as numbness and weakness in the distribution of the involved nerve root. Radicular pain typically travels along a narrow band and has a sharp, shooting, and lancinating quality. Gait disturbances, loss of sensation, reduced muscle strength, and diminished reflexes involve the appropriate affected dermatomal distribution.
Inflammation in the spinal canal secondary to a herniated disc plays an important role in the causation of back and radicular pain. Herniated nucleus pulposus results in local release of cytokines and other inflammatory mediators that cause a chemical radiculitis. High levels of phospholipase A2 activity were noted in human disc fragments removed at surgery from patients with symptomatic radiculopathy. Increased levels of the inflammatory cytokines interleukin-6 and interleukin-8 were noted from disc material taken from patients with known disc disease.37 The application of disc material onto spinal nerve roots can induce functional and morphologic changes in the nerves. Disc cells express TNF-α, which, when applied to spinal nerve roots, causes similar changes to those seen after application of disc material; selective inhibition of TNF-α may reduce the intraneural edema.38 A double-blind, placebo-controlled study showed that an intradiscal injection of 1.5 mg of etanercept, a TNF-α inhibitor, in a pain-generating disc did not reduce the pain scores or disability scores of patients with chronic discogenic pain or lumbosacral radiculopathy.39
 For patients with radicular symptoms who do not respond to conservative management, including anti-inflammatory medications, epidural steroid injections (ESIs) may be useful. Epidural steroids have an anti-inflammatory effect related to inhibition of phospholipase A2 activity. In addition, steroids have a local anesthetic and antinociceptive effect. The local application of methylprednisolone blocks transmission of C fibers but not the Aβ fibers. Several prospective, randomized, and controlled studies have demonstrated short-term efficacy of ESIs for treatment of lumbar spine radiculopathy40–42 while others have not.43,44 Another study demonstrated less leg pain and sensory deficit with ESI, but the incidence of surgery was the same between the steroid and the control groups.45 For cervical ESIs, the few studies that have been done are mostly descriptive and their results were the same as in lumbar ESIs, that is, transient relief from the injections. The transient efficacy of the ESIs lasted no more than 3 months. These transient effects were noted by the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology,46 which recommended against the routine use of ESIs. This recommendation has to be viewed against the natural history of patients with herniated disc and spinal stenosis as these patients seem to do well over time with conservative management. The transient relief provided by ESIs may minimize the need for opioids and potent anti-inflammatory medications and their related side effects. ESIs should be a component, and not the sole modality, of the conservative management of radicular pain.
For patients with radicular symptoms who do not respond to conservative management, including anti-inflammatory medications, epidural steroid injections (ESIs) may be useful. Epidural steroids have an anti-inflammatory effect related to inhibition of phospholipase A2 activity. In addition, steroids have a local anesthetic and antinociceptive effect. The local application of methylprednisolone blocks transmission of C fibers but not the Aβ fibers. Several prospective, randomized, and controlled studies have demonstrated short-term efficacy of ESIs for treatment of lumbar spine radiculopathy40–42 while others have not.43,44 Another study demonstrated less leg pain and sensory deficit with ESI, but the incidence of surgery was the same between the steroid and the control groups.45 For cervical ESIs, the few studies that have been done are mostly descriptive and their results were the same as in lumbar ESIs, that is, transient relief from the injections. The transient efficacy of the ESIs lasted no more than 3 months. These transient effects were noted by the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology,46 which recommended against the routine use of ESIs. This recommendation has to be viewed against the natural history of patients with herniated disc and spinal stenosis as these patients seem to do well over time with conservative management. The transient relief provided by ESIs may minimize the need for opioids and potent anti-inflammatory medications and their related side effects. ESIs should be a component, and not the sole modality, of the conservative management of radicular pain.
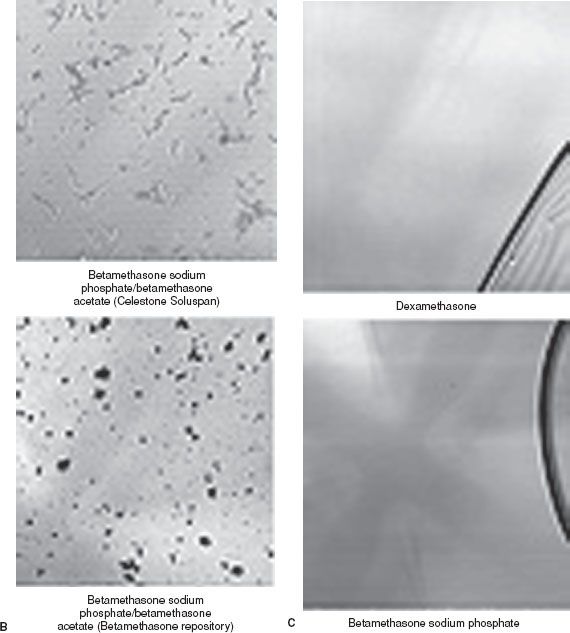
A transforaminal approach can be employed to deposit steroid in the anterolateral epidural space where the herniated disc is located, through the intervertebral foramina, and distally along the nerve root (Fig. 57-2). This approach is especially indicated in radicular pain specific to a single nerve root. Prospective, randomized studies on transforaminal ESIs show the same results as with the interlaminar approach, that is, short-term efficacy of the injection.47–49 The transforaminal approach has a better rationale than the midline interlaminar approach, and studies that compared the two approaches show better efficacy with the transforaminal approach.50,51 A study comparing the parasagittal (paramedian approach) and transforaminal approach showed a more ideal spread of the contrast dye in the parasagittal approach although the efficacy was similar between the two techniques.52
FIGURE 57-2. Right L5 transforaminal epidural injection. Note the spread of the contrast medium proximally into the lateral epidural space and distally along the nerve root.
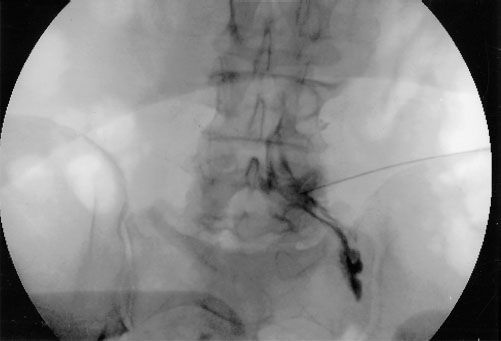
It is advisable that fluoroscopy be used in ESI, especially with the transforaminal approach, to assure insertion of the needle at the affected vertebral level and document the flow of the contrast medium (and the drug). Reassessment should be carried out 2 to 3 weeks after the initial injection. The use of multiple ESIs in a patient, with a short interval between injections, is not advised. If there is no response to an initial injection, it can be repeated once as some patients require a second injection before they respond. If there is partial response, up to three injections can be performed.
The complications of ESI may be due to the technique or from the injected drug, as well as the vehicle and additives. Complications related to the technique include needle trauma, vasospasm, and infection. Glucocorticoids reduce the hypoglycemic effect of insulin and interfere with blood glucose control in patients with diabetes mellitus. Insulin sensitivity may be impaired, there may be no change in the HbA1C levels, or the blood glucose can be increased for 1 week after ESIs. A single dose of 80 mg of methylprednisolone can suppress plasma cortisol levels and the ability to secrete cortisol in response to synthetic corticotropin for up to 3 weeks. Epidural triamcinolone, 80 mg, can suppress serum cortisol and corticotropin levels for up to 7 days after injection. The median recovery to normal levels occurs within 1 month after the last injection, and full recovery is at 3 months.
Injury to the brain or spinal cord can occur with transforaminal ESIs.53 The cerebral/cerebellar events can be ascribed to trauma to the vertebral artery, vasospasm from the injected steroid or dye, or embolism of the particulate steroid via the vertebral artery.54,55 The spinal cord injuries can be ascribed to injury to the radicular artery accompanying the nerve root, spasm of the radicular artery from the injected dye or steroid, embolism of the particulate steroid, or from proximal intraneural spread of the injectate. The injection of contrast medium through a radicular artery that passed to the spinal cord or the anterior spinal artery has been demonstrated. The occurrence of adverse events at the lumbar level has been ascribed to intra-arterial injection into an abnormally low-lying artery of the Adamkiewicz. These adverse events have also been described after injection of local anesthetic or dye, without steroid.55 The use of computed tomography (CT), instead of fluoroscopy, does not assure avoidance of the adverse events.
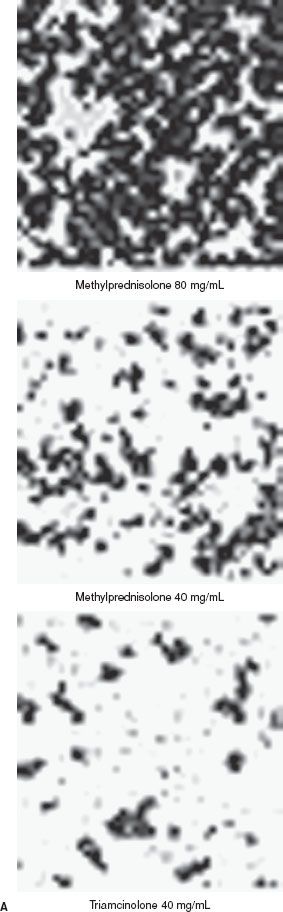
Huntoon56 noted that the vertebral, ascending cervical, and deep cervical arteries supply segmental medullary vessels and that the ascending and deep cervical arteries are within 2 mm of the site of insertion of the needle for cervical transforaminal ESIs. The proximity of these arteries to the site of needle placement makes these blood vessels vulnerable to trauma or unintentional sites of injection of the steroid. Occlusion of the vessels occurs from the particulate steroids. Methylprednisolone acetate has the largest particle size, betamethasone the smallest particles, and triamcinolone acetonide is in between55 (Fig. 57-3). Dexamethasone has no identifiable particles. Dexamethasone appears to be ideal for transforaminal ESIs; however, it is easily washed out from the epidural space, and studies on its efficacy are only preliminary.57 The following steroids are recommended for ESIs: (1) Methylprednisolone, triamcinolone, or betamethasone for interlaminar injections; (2) betamethasone (preferably) or triamcinolone for lumbar transforaminal injections; and (3) dexamethasone for cervical transforaminal injections.
FIGURE 57-3. A: Typical microscopic appearances of methylprednisolone, 80 mg/mL and 40 mg/mL, and triamcinolone 40 mg/mL. The particles are amorphous in appearance. B: The particles of commercial betamethasone (Celestone Soluspan) are rodlike and lucent, while those of the compounded betamethasone (betamethasone repository) are amorphous. C: Note that dexamethasone is pure liquid. (From: Benzon HT, Chew TL, McCarthy R, et al. Comparison of the particle sizes of the different steroids and the effect of dilution: A review of the relative neurotoxicities of the steroids. Anesthesiology. 2007;106:331, with permission.)
ESIs are more effective in patients with acute radicular symptoms; however, they are not effective in patients with chronic lumbar radiculopathy.58 There have been several prospective, randomized controlled studies on the efficacy of surgery in relieving back pain secondary to herniated disc. It appears that surgery for herniated disc produces only short-term relief, whereas the long-term results are comparable with those with conservative management.59 For spinal stenosis, surgery is associated with greater improvements in most outcome measures.
Low Back Pain: Facet Syndrome
Patients with low back pain secondary to facet pathology have pain in the low back that radiates to the ipsilateral posterior thigh and usually ends at the knee. On physical examination there is paraspinal tenderness and reproduction of pain with extension–rotation maneuvers of the back. The diagnosis of facet syndrome is arrived at by a combination of the patient’s history, physical examination findings, and a positive response to diagnostic medial branch blocks or facet joint injections (Fig. 57-4). For medial branch blocks, some investigators recommend the use of local anesthetics with different durations of effect (e.g., lidocaine and bupivacaine) and to correlate the duration of relief with the known duration of effect of the drug.
FIGURE 57-4. Left L4 to L5 facet joint injection. The injection of 5 mL of contrast medium demonstrates the extent of the joint capsule.
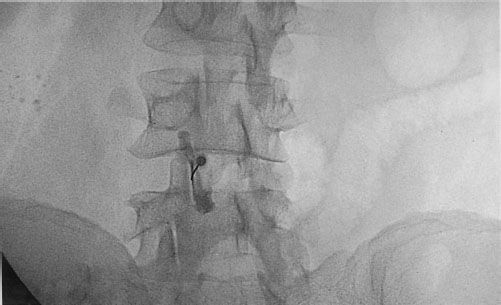
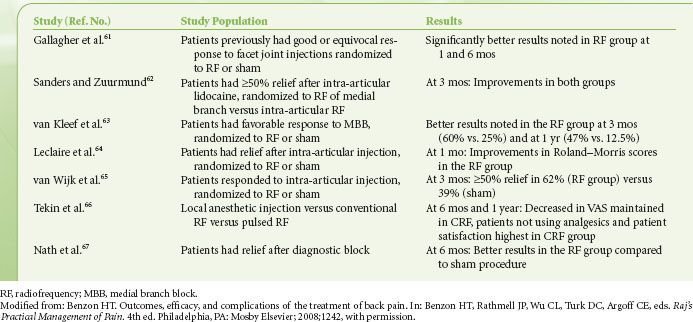
Some patients may have a prolonged response to facet joint injections, that is, up to 3 to 6 months. If the patient has a prolonged response, it is best to wait for recurrence of the pain. If the relief is short-lived, especially after medial branch blocks, then thermal radiofrequency (RF) rhizotomy of the medial branches should be performed. It appears that there is no relationship between the mean sensory stimulation threshold (which denotes proximity of the electrode to the nerve) during lumbar facet rhizotomy denervation and treatment outcome.60 Randomized controlled studies have shown improvements after thermal RF of the lumbar medial branches that lasted 3 to 12 months61–67 (Table 57-3). With regard to cervical facet syndrome, controlled studies on thermal RF of the cervical medial branches have shown different results. Lord et al.68 showed better results after RF (return to work and relief of pain) while Stovner et al.69 showed no difference between the RF and sham procedures.
TABLE 57-3. RANDOMIZED, CONTROLLED STUDIES ON RADIOFREQUENCY DENERVATION OF THE MEDIAL BRANCHES (FACET NERVES)
Buttock Pain: Sacroiliac Joint Syndrome and Piriformis Syndrome
The pain of sacroiliac joint syndrome is located in the region of the affected sacroiliac joint and the medial buttock. The pain may radiate to the groin, posterior thigh, and occasionally below the knee. Physical examination usually reveals tenderness over the sacroiliac sulcus, reduction in the joint mobility, and reproduction of the pain when the affected sacroiliac joint is stressed. The most commonly used tests for sacroiliac joint dysfunction include the FABER Patrick, Gaenslen, Yeoman, sacroiliac shear, and Gillet tests. The FABER Patrick and the Yeoman test do not rule out hip pathology while the Yeoman and the shear tests are more specific for sacroiliac joint syndrome. The presence of symptoms and physical examination findings suggestive of SI joint syndrome, pain on three of the tests, and a positive response to sacroiliac joint injection are adequate to make the diagnosis of sacroiliac joint syndrome.
The treatments for sacroiliac joint syndrome include physical therapy, manipulation, intra-articular steroid injections (Fig. 57-5), radiofrequency denervation, and surgical fusion of the joint. Physical therapy and chiropractic manipulations are used extensively for the treatment of sacroiliac joint disease; however, there is no large outcome study validating their use. Intra-articular injections of steroid (40 to 80 mg of methylprednisolone or other depot steroid) and local anesthetic into the sacroiliac joint results in a few months of pain relief, but again, no prospective controlled studies support their use.
FIGURE 57-5. Sacroiliac joint injection. Note the spread of the contrast medium along the joint. (From: Benzon HT, Nader A. Hip, sacroiliac joint, and piriformis injections. In: Benzon HT, Rathmell J, Wu C, Turk DC, Argoff C, eds. Raj’s Practical Management of Pain. 4th ed. Philadelphia, PA: Mosby Elsevier; 2008;1070, with permission.)

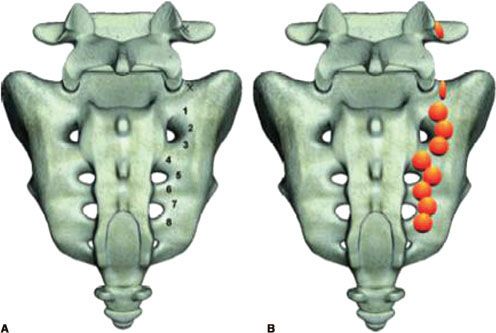
Denervation of the lower portion of the sacroiliac joint may be achieved by the creation of bipolar RF strip lesions along the dorsal border of the sacroiliac joint in a leapfrog manner. Local anesthetic blockade of the sensory innervation of the dorsal portion of the sacroiliac joint—the medial branch of the dorsal rami of L5 and the lateral branches of the dorsal rami of S1 to S3—can be performed initially or when the relief from the sacroiliac joint injection is temporary. Relief from the local anesthetic block may last weeks to months when combined with physical therapy. Monopolar and bipolar thermal radiofrequency lesioning of the lateral branches is performed for a more lasting relief. The bigger lesions created by the water-cooled radiofrequency technique (Fig. 57-6)70 are inherently more effective since it accommodates for the variations in the location of the lateral branches along the lateral border of the sacral foraminas.71
FIGURE 57-6. Target points (A) and expected lesions (B) from water-cooled radiofrequency denervation at the right L5 medial branch and the S1, S2, and S3 lateral branches (From: Cohen SP, Hurley RW, Buckenmaier CC 3rd, et al. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology. 2008;109:279–288, with permission.)
Piriformis Syndrome
Piriformis syndrome, another pain syndrome that originates in the buttock, comprises 5% to 6% of patients referred for the treatment of back and leg pain. It occurs after trauma, surgery, and infection, or from compression of one of the components of the sciatic nerve as it runs between two divisions of the piriformis muscle.72 Patients with piriformis syndrome complain of buttock pain with or without radiation to the ipsilateral leg. The buttock pain usually extends from the sacrum to the greater trochanter of the femur whereas irritation of the sciatic nerve results in a buttock pain that radiates to the ipsilateral leg. Prolonged sitting, as in driving or biking, or getting up from a sitting position aggravates the pain. The pain is aggravated by hip flexion, adduction, and internal rotation. Neurologic examination is usually negative. There may be leg numbness when the sciatic nerve is irritated; the straight-leg test may be normal or limited. Three signs confirm the presence of piriformis syndrome72: (1) The Pace sign wherein there is pain and weakness on resisted abduction of the hip in a patient who is seated with the hip flexed; (2) the Lasègue sign wherein there is pain on flexion, adduction, and internal rotation of the hip in a patient who is supine (note that some clinicians call pain on straight-leg raise the Lasègue sign also); and (3) the Freiberg sign wherein there is pain on forced internal rotation of the extended thigh. Note that the piriformis is an internal rotator of the flexed hip and an external rotator of the extended hip. The diagnosis of piriformis syndrome is made on clinical grounds. Electromyography may detect myopathic and neuropathic changes including a delay in the H-reflex with the affected leg in a flexed, adducted, and internally rotated (FAIR) position as compared with the same H-reflex in the normal anatomic position.73 The CT scan of the soft tissues of the pelvis may show an enlarged piriformis muscle, or abnormal uptake by the muscle, and the MRI confirms an enlarged piriformis muscle.
The treatments of piriformis syndrome include physical therapy combined with medications including muscle relaxants, anti-inflammatory drugs, and analgesics to reduce the spasm, inflammation, and pain. Local anesthetic and steroid injections into the piriformis muscle may break the pain/muscle spasm cycle. Although blind injections can be done, more specific techniques involve identification of the piriformis muscle with muscle electromyography, CT guidance, use of a nerve stimulator, or combined fluoroscopy–nerve stimulator guidance.72 If relief from the local anesthetic does not last, then the piriformis muscle is injected with 100 units of botulinum toxin A in 2 to 3 mL of local anesthetic. The reported complications of botulinum toxin injection include brachial plexopathy, polyradiculoneuritis, and local psoriasiform dermatitis, so precautions should be followed to assure injection of the botulinum toxin into the belly of the piriformis muscle.
Myofascial Pain Syndrome and Fibromyalgia
Myofascial pain syndrome is a painful regional syndrome characterized by the presence of an active trigger point in a skeletal muscle. The trigger point can be felt as a palpable taut band and manipulation of the trigger point by digital pressure or by penetration by a needle may induce a twitch response. There is spot tenderness in the taut band, pressure on the tender nodule induces pain that the patient recognizes as an experienced pain pattern, and there may be painful limitation to full passive range of motion of the affected muscle. There is usually an electromyographic demonstration of spontaneous electrical activity characteristic of active loci in the tender nodule of a taut band.
The management of myofascial pain syndrome includes repeated applications of a cold spray over the trigger point in line with the involved muscle fibers, followed by gentle massage of the trigger point and stretching of the affected muscle. Another treatment is local anesthetic injection or dry needling of the trigger point. Trigger point injections may be done under ultrasound but the benefits of this technique have not been proven. Recent studies show that dry needling may be as effective as local anesthetic injection; however, the local anesthetic makes the procedure less painful. Several injections at 1- to 3-week intervals, followed by physical therapy, may result in a long-term benefit. Botulinum toxin injections have been recommended but the results of clinical studies have not been uniform.74,75 Physical therapy includes improving posture, body mechanics, relaxation techniques, trigger point massage, post-isometric relaxation, and reciprocal inhibition.
Fibromyalgia
The American College of Rheumatology criteria for classification of fibromyalgia,76 established in 1990, requires two components: A history of widespread pain for at least 3 months and allodynia to digital pressure at 11 or more of 18 anatomically defined tender points. The tender points are located in the occiput, the intertransverse spaces between C5 and C7, trapezii, supraspinatus, the second rib, just lateral to the costochondral junctions, lateral epicondyles, glutei, greater trochanters, and knees. Others employ a whole body pain diagram to indicate areas of pain and obviate the need for tender points.77 Finally, some clinicians do not require tender points and expand the definition of fibromyalgia to include symptoms of fatigue, sleep disturbance, and cognitive dysfunction.78
There is a strong genetic and familial component to the development of fibromyalgia. Also, family members of fibromyalgia patients are also more likely to have irritable bowel syndrome, temporomandibular disorders, headaches, and a host of other regional pain syndromes. They have higher concentrations of substance P and glutamate in CSF compared with normal controls.79,80
The opioidergic activity is normal or increased in fibromyalgia, and levels of cerebrospinal fluid enkephalins are roughly twice as high in these patients compared to healthy controls.81 The increased activity of endogenous opioidergic systems explains the anecdotal experience of clinicians that opioids are ineffective in this syndrome. On the other hand, the principal metabolite of norepinephrine, 3-methoxy-4-hydroxyphenethylene glycol (MPHG), is lower in the CSF of patients with fibromyalgia.82 This may explain the efficacy of drugs that raises both serotonin and norepinephrine (tricyclic antidepressants, duloxetine, milnacipran, tramadol).
The optimal treatment of fibromyalgia supports a multifaceted program comprising pharmacologic therapy and nonpharmacologic therapy (education, exercise, and cognitive behavioral therapy). Efficacious medications for treatment of fibromyalgia include the two SNRIs, duloxetine and milnacipran.83,84 Pregabalin, amitriptyline, gabapentin, and gamma-hydroxybutyrate (sodium oxybate) are also effective.85,86 Exercise programs, specifically low-intensity low-impact programs, appear to be beneficial. Cognitive-behavioral therapy and operant-behavioral therapy also appear to be helpful in these patients.
NEUROPATHIC PAIN SYNDROMES
Herpes Zoster and Postherpetic Neuralgia
Some patients with acute herpes zoster have a prodrome of dermatomal pain before the skin eruptions. The pain of acute herpes zoster is usually moderate in severity and can be managed with analgesics, and the pain usually subsides with healing of the rash. Ten percent to 15% of the patients develop postherpetic neuralgia (PHN), or pain that persists >3 months after resolution of the rash; the incidence rises to 30% to 50% in the elderly. The risk factors for the development of PHN include increased pain during the acute stage, greater severity of the skin lesion, older age, and the presence of a prodrome. The use of antiviral drugs acyclovir, famciclovir, or valacyclovir has been shown to hasten the healing of the rash, reduce the duration of viral shedding, and decrease the increase of PHN.
 Most of the studies on the efficacy of neuraxial and peripheral nerve blocks, performed during the acute stage of herpes zoster were either retrospective or case series. Prospective, randomized, and controlled studies provide conflicting results. A study in which epidural methylprednisolone and bupivacaine was compared with acyclovir and prednisolone showed the epidural steroid group to have less pain (1.6% vs. 22%) and less allodynia (4% vs. 12%) at 1 year.87 Another study in which standard therapy with oral antiviral medications and analgesics was compared with standard therapy and epidural methylprednisolone and bupivacaine noted less pain in the epidural group (48% vs. 58%) at 1 month but not at 3 months (21% vs. 28%).88 The difference between the two studies is that only one epidural injection was performed in the study that showed no long-term beneficial effect of epidural steroid compared with two to four injections in the study that showed benefit with ESIs. To be effective in preventing PHN, the blocks are preferably done within 2 to 4 weeks of the onset of rash.
Most of the studies on the efficacy of neuraxial and peripheral nerve blocks, performed during the acute stage of herpes zoster were either retrospective or case series. Prospective, randomized, and controlled studies provide conflicting results. A study in which epidural methylprednisolone and bupivacaine was compared with acyclovir and prednisolone showed the epidural steroid group to have less pain (1.6% vs. 22%) and less allodynia (4% vs. 12%) at 1 year.87 Another study in which standard therapy with oral antiviral medications and analgesics was compared with standard therapy and epidural methylprednisolone and bupivacaine noted less pain in the epidural group (48% vs. 58%) at 1 month but not at 3 months (21% vs. 28%).88 The difference between the two studies is that only one epidural injection was performed in the study that showed no long-term beneficial effect of epidural steroid compared with two to four injections in the study that showed benefit with ESIs. To be effective in preventing PHN, the blocks are preferably done within 2 to 4 weeks of the onset of rash.
 The mainstay of treatment for PHN is pharmacologic management that includes anticonvulsants, opioids, and antidepressants. Although the antidepressants have been found to be effective, their use is precluded by the frequent occurrence of side effects. The side effects include anticholinergic effects such as tachycardia, dry mouth, constipation, and prostatism in the elderly. Nortriptyline is preferred over amitriptyline because it is equally effective and better tolerated. Studies showed opioids and tramadol to be efficacious.89–91
The mainstay of treatment for PHN is pharmacologic management that includes anticonvulsants, opioids, and antidepressants. Although the antidepressants have been found to be effective, their use is precluded by the frequent occurrence of side effects. The side effects include anticholinergic effects such as tachycardia, dry mouth, constipation, and prostatism in the elderly. Nortriptyline is preferred over amitriptyline because it is equally effective and better tolerated. Studies showed opioids and tramadol to be efficacious.89–91
The anticonvulsants gabapentin and pregabalin are usually effective in the management of PHN.92–94 The side effects of the drugs include somnolence, dizziness, and peripheral edema. Two studies showed that the combination of gabapentin and controlled- release morphine, and gabapentin and nortriptyline, were more effective and at lower daily dosages than either drug given alone.95,96 Based on efficacy, antidepressants are the first choice for neuropathic pain syndromes, followed by opioids, tramadol, and gabapentin/pregabalin.97 If quality of life, side effects, prevention of addiction, and regulatory issues are important considerations in addition to pain relief, then gabapentin/pregabalin are the first drugs of choice. These are followed by tramadol, opioids, and the tricyclic antidepressants.97 For the allodynia that accompanies the PHN, lidocaine patch is recommended.
Interventional techniques may be performed if medications do not control the pain of PHN. Intrathecal methylprednisolone, 60 mg in lidocaine, given once a week for 4 times, was noted to be more effective in relieving PHN compared with intrathecal lidocaine or no treatment.98 The cerebrospinal fluid levels of interleukin-8, a marker of inflammation, decreased by >50% in the intrathecal methylprednisolone group and this correlated with the duration of global pain relief. It should be noted that epidural methylprednisolone is not as beneficial as intrathecal administration.99 Other interventional techniques for PHN are spinal cord stimulation (SCS) and intrathecal alcohol. When a spinal cord stimulator was placed in 28 patients with intractable PHN for 2 years, long-term pain relief was achieved in 23 patients and the median pain score decreased from 9 to 1.100 The improvements were confirmed by inactivation, followed by activation of the spinal cord stimulator at quarterly intervals. In resistant cases or when the patient cannot tolerate the medications, pain may be relieved by alcohol neurolysis of the spinal thoracic dermatomes affected by the herpes zoster.101
Diabetic Painful Neuropathy
Peripheral neuropathy may be present in approximately 65% of patients with insulin-dependent diabetes, most commonly distal symmetric polyneuropathy, followed by median nerve mononeuropathy at the wrist, and visceral autonomic neuropathy. The incidence of diabetic neuropathy increases with duration of diabetes, age, and degree of hyperglycemia; neuropathies generally develop after persistence of hyperglycemia for several years. The pathophysiology of diabetic neuropathy includes the polyol pathway, microvascular, and glycosylation end-product theories.102 All pathways result in chronic ischemia of the nerve.
The management of diabetic painful neuropathy (DPN) includes tight control of the patient’s blood glucose and pharmacologic therapy. The anticonvulsants gabapentin and pregabalin appear to be effective in the management of DPN, with the efficacy of gabapentin enhanced by the addition of controlled-release morphine or nortriptyline.95,96 The tricyclic antidepressants are also effective in DPN whereas the selective serotonin reuptake inhibitors are not as effective. The antidepressant duloxetine appears to be effective103 and, together with its favorable side effect profile compared with the tricyclics, is now widely used in treatment of DPN. The European Federation of Neurological Sciences Task Force and the International Association for the Study of Pain Neuropathic Pain Special Interest group (NeuP-SIG) now recommend the serotonin–norepinephrine reuptake inhibitors (duloxetine, milnacipran) as the first-choice drugs for the treatment of DPN.104,105 Finally, the opioids and tramadol are also effective in the treatment of DPN.
includes tight control of the patient’s blood glucose and pharmacologic therapy. The anticonvulsants gabapentin and pregabalin appear to be effective in the management of DPN, with the efficacy of gabapentin enhanced by the addition of controlled-release morphine or nortriptyline.95,96 The tricyclic antidepressants are also effective in DPN whereas the selective serotonin reuptake inhibitors are not as effective. The antidepressant duloxetine appears to be effective103 and, together with its favorable side effect profile compared with the tricyclics, is now widely used in treatment of DPN. The European Federation of Neurological Sciences Task Force and the International Association for the Study of Pain Neuropathic Pain Special Interest group (NeuP-SIG) now recommend the serotonin–norepinephrine reuptake inhibitors (duloxetine, milnacipran) as the first-choice drugs for the treatment of DPN.104,105 Finally, the opioids and tramadol are also effective in the treatment of DPN.
Complex Regional Pain Syndrome
Complex regional pain syndrome (CRPS) consists of two types. CRPS type I was originally termed reflex sympathetic dystrophy, whereas CRPS type II represents causalgia. The risk factors for the development of CRPS include previous trauma, nerve injury (for causalgia), previous surgery, work-related injuries, and female sex. The signs and symptoms of CRPS include spontaneous pain, hyperalgesia, allodynia, plus trophic, sudomotor, vasomotor abnormalities, and finally, active and passive movement disorders. There may be a discrepancy between the severity of the symptoms and intensity of the inciting injury. The clinical features of CRPS type II are the same as in CRPS type I except there is a preceding nerve injury in CRPS II. The International Association for the Study of Pain (IASP) has proposed standardized diagnostic consensus-based criteria for CRPS. Studies on the validity of the IASP criteria suggest that patients should have (1) at least one symptom in each of the following general categories: Sensory (hyperesthesia-increased sensitivity to a sensory stimulation), vasomotor (temperature abnormalities or skin color changes), sudomotor–fluid balance (sweating abnormalities or edema), or motor (decreased range of movement, weakness, tremor, or neglect); and (2) at least one sign within two or more of the following categories: Sensory (allodynia or hyperalgesia), vasomotor (objective temperature abnormalities or skin color changes), sudomotor–fluid balance (sweating abnormalities or objective edema), or motor (objective decreased range of motion, weakness, tremor or neglect).
 The treatments for CRPS include sympathetic blocks, physical therapy, and oral medications. Pharmacologic therapy for CRPS includes gabapentin,106 memantine (an NMDA blocker), and ketamine infusion. Ketamine can either be given as a 4- to 5-day infusion at 1 to 7 μg/kg/min (5 to 30 mg/hr in a 70-kg patient)107 or for 4 hours daily for 10 days at an infusion rate of 0.35 mg/kg/hr (24 mg/hr in a 70-kg person).108 SCS can be entertained if the patient does not respond to these treatments.109
The treatments for CRPS include sympathetic blocks, physical therapy, and oral medications. Pharmacologic therapy for CRPS includes gabapentin,106 memantine (an NMDA blocker), and ketamine infusion. Ketamine can either be given as a 4- to 5-day infusion at 1 to 7 μg/kg/min (5 to 30 mg/hr in a 70-kg patient)107 or for 4 hours daily for 10 days at an infusion rate of 0.35 mg/kg/hr (24 mg/hr in a 70-kg person).108 SCS can be entertained if the patient does not respond to these treatments.109
Human Immunodeficiency Virus Neuropathy
Symptomatic neuropathy occurs in 10% to 35% of patients who are seropositive for human immunodeficiency virus (HIV), and pathologic abnormalities exist in almost all patients with end-stage AIDS. The sensory neuropathies associated with HIV include distal sensory polyneuropathy, the more common neuropathy related to the viral infection, and antiretroviral toxic neuropathy (ATN) secondary to the treatment. The clinical features of HIV sensory neuropathy typically include painful allodynia and hyperalgesia. The onset is gradual and most commonly involves the lower extremities. The neuropathy and dysesthesia progress from the distal to the more proximal structures. There is minimal subjective or objective motor involvement and this is generally limited to the intrinsic muscles of the foot.
The treatment of HIV sensory neuropathy is symptomatic and includes optimization of the patient’s metabolic and nutritional status. Cessation or dose reduction of treatment with nucleoside reverse transcriptase inhibitors may improve the symptoms of ATN. The anticonvulsants, particularly lamotrigine (300 mg/day), can be effective therapy for HIV sensory neuropathy as well as ATN.110,111 Gabapentin is also effective at doses of 1,200 to 3,600 mg/day.112
Phantom Pain
Nearly all patients with amputated extremities experience nonpainful sensations in the absent, phantom limb. As many as 80% of them experience pain. The onset of pain may be immediate but commonly occurs within the first few days following amputation. Approximately 50% of patients experience a decrease of their pain with time, whereas the other 50% report no change or an increase in pain over time. Phantom pain is not felt all the time, only a few days in a month. Phantom pain is caused by both peripheral and central factors. Peripheral mechanisms include neuromas, an increase in C-fiber activity, and sodium channel activation. Central mechanisms include abnormal firing of spinal internuncial neurons and supraspinal involvement secondary to the development of new synaptic connections in the cerebral cortex.
Numerous prophylactic measures have been undertaken in an attempt to reduce the incidence of phantom limb pain, including perioperative epidural infusions of opioids and local anesthetics or clonidine, and continuous brachial plexus blockade with memantine. The treatment of phantom limb pain includes pharmacologic and nonpharmacologic measures. Pharmacologic treatments include the use of opioids; gabapentin, an NMDA antagonist; and the empirical use of antidepressants. The nonpharmacologic measures include transcutaneous electrical nerve stimulation, spinal cord stimulators, and biofeedback. A combination of pharmacologic treatment with physical, psychological, or behavioral intervention is probably most effective approach.113
CANCER PAIN
Significant pain is present in up to 25% of patients with cancer who are in active treatment and in up to 90% of patients with advanced cancer. The pain of cancer can be somatic, visceral, or neuropathic. The etiology and characteristics of these pain syndromes are different and they require different treatments. Somatic pain tends to be responsive to opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), or cyclooxygenase 2 inhibitors, and is amenable to treatment with neural blockade. Visceral pain responds to sympathetic blocks, and neuropathic pain is responsive to anticonvulsants, opioids, tricyclic antidepressants, serotonin–norepinephrine reuptake inhibitors, or combinations of these drugs.
Management of cancer pain should be multifaceted and include the following: (1) Antineoplastic treatment, (2) pharmacologic management, (3) interventional management, (4) behavioral and psychological management, and ultimately (5) hospice care. Pharmacologic therapies include opioids, antidepressants, anticonvulsants, NSAIDs, corticosteroids, oral local anesthetics, and topical analgesics. Continuous intravenous opioid infusions can be infused during the later stages of life. Interventional treatments include neurolytic sympathetic blocks and intrathecal opioids; vertebroplasty or kyphoplasty is performed for vertebral compression syndromes.
 Opioids are the mainstay of treatment for cancer pain as approximately 70% to 95% of patients are responsive positively when appropriate guidelines are followed. Neurolytic blocks and intrathecal opioids should be considered when pharmacologic agents are not completely effective at maximum tolerated dosages.
Opioids are the mainstay of treatment for cancer pain as approximately 70% to 95% of patients are responsive positively when appropriate guidelines are followed. Neurolytic blocks and intrathecal opioids should be considered when pharmacologic agents are not completely effective at maximum tolerated dosages.
Neurolytic Blocks for Visceral Pain from Cancer
Celiac Plexus Block
The celiac plexus innervates all of the abdominal viscera except the left side of the colon and the pelvic viscera. The plexus contains two large ganglia that receive sympathetic fibers from the greater, lesser, and least splanchnic nerves. It also receives parasympathetic fibers from the vagus nerve. The splanchnic nerves are located retroperitoneally at the level of the T12 and L1 vertebrae, and the celiac plexus are anterior to the crura of the diaphragm and surrounds the abdominal aorta and the celiac and superior mesenteric arteries.
Blockade of the celiac plexus can be achieved by the classic retrocrural approach, anterocrural approach, or by neurolysis of the splanchnic nerves.114 For the procedure, the tip of the needle is directed toward the body of L1 (Fig. 57-7). In the retrocrural approach, the tip of the needle is advanced approximately 1 cm anterior to the anterior and upper border of L1. In anterocrural or transaortic approach, the tip of the needle is advanced through the lower portion of L1 and the aorta on the left side until blood can no longer be aspirated through the needle. For splanchnic nerve block, the tip of the needle is placed at the anterior portion of the T12 vertebral body. There appears to be no differences in efficacy between the three approaches.114 Fluoroscopy is required in the performance of the procedure. CT allows visualization of the diaphragm and aorta, and is used in the transabdominal approach when patients cannot tolerate the prone position. Some clinicians perform an initial diagnostic block with a local anesthetic while others proceed immediately to a neurolytic block since the results of the diagnostic and neurolytic blocks may not be the same. Better results are usually seen with local anesthetics because of better spread (phenol is viscous) and its vascular absorption may relieve pain. Fifty percent alcohol or 6% to 10% phenol is employed for the neurolytic block. The dosages of the neurolytic agents are 30 to 40 mL for the retrocrural and anterocrural approach, and 10 to 15 mL on each side for splanchnic nerve blockade. Complications from the celiac plexus block include orthostatic hypotension, back pain, retroperitoneal hematoma, reactive pleurisy, hiccups, hematuria, transient diarrhea, abdominal aortic dissection, transient motor paralysis, and paraplegia. The paraplegia and transient motor paralysis may be due to spasm of the lumbar segmental arteries that perfuse the spinal cord, direct vascular or neurologic injury, or retrograde spread to the nerve roots or spinal cord.
FIGURE 57-7. Retrocrural versus anterocrural approaches to neurolysis of the celiac plexus. Note that the tip of the needle is in the upper third of L1 and about 1 cm beyond the border of the vertebral body for the retrocrural technique; the spread of the contrast medium is cephalad. In contrast, the tip of the needle is the lower third of L1 and about 3 cm beyond the border of the vertebral body for the anterocrural technique; the spread of the contrast medium is caudad and in front of the aorta (arrow). (From: de Leon-Casasola OA. Neurolysis of the sympathetic axis for cancer pain management. In: Benzon HT, Rathmell J, Wu C, Turk DC, Argoff C, eds. Raj’s Practical management of Pain. 4th ed. Philadelphia, PA: Mosby Elsevier; 2008; 918, with permission.)

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






