There are certain principles that are common to all such events, independent of their etiology, and as a group anesthesiologists are as well prepared if not better prepared to assist their communities in planning for and in caring for patients from a disaster.
 Any time a situation arises in which medical capability is significantly below standards to which we are accustomed in the United States the anesthesiologist is indeed practicing in an austere environment.
Any time a situation arises in which medical capability is significantly below standards to which we are accustomed in the United States the anesthesiologist is indeed practicing in an austere environment.
 If one has a pet, family or friends living with them, or has legal responsibility for a loved one (elderly parents, disabled person) one must have a plan for these individuals that provides care for them.
If one has a pet, family or friends living with them, or has legal responsibility for a loved one (elderly parents, disabled person) one must have a plan for these individuals that provides care for them.
 Despite the best effort of law enforcement, fire and rescue teams, and emergency medical agencies, hospitals will continue to play a vital role in helping communities respond to catastrophic events.
Despite the best effort of law enforcement, fire and rescue teams, and emergency medical agencies, hospitals will continue to play a vital role in helping communities respond to catastrophic events.
 Anesthesiologists’ basic understanding of physiology and pharmacology, their airway skills, their fluid resuscitation expertise, their ability to manage ventilators and to provide anesthesia in the field environment, in the emergency department, in the operating room, and in intensive care units (ICUs) will be invaluable.
Anesthesiologists’ basic understanding of physiology and pharmacology, their airway skills, their fluid resuscitation expertise, their ability to manage ventilators and to provide anesthesia in the field environment, in the emergency department, in the operating room, and in intensive care units (ICUs) will be invaluable.
 If assigned to triage patients, the anesthesiologist will be expected to classify patients into four groups—those requiring immediate care, delayed care, first aid, and expectant.
If assigned to triage patients, the anesthesiologist will be expected to classify patients into four groups—those requiring immediate care, delayed care, first aid, and expectant.
 Anesthesiologists should position themselves at the head of the bed and assume responsibility for the airway and venous access. For the former it would be ideal to have two or three assistants (one providing in-line C-spine stabilization, another individual applying cricoid pressure, and a third individual administering medications).
Anesthesiologists should position themselves at the head of the bed and assume responsibility for the airway and venous access. For the former it would be ideal to have two or three assistants (one providing in-line C-spine stabilization, another individual applying cricoid pressure, and a third individual administering medications).
 The toxicity of the nerve agents depends on the compound delivered, the dose that is delivered (LC), and the time (t) that an individual is exposed to that dose.
The toxicity of the nerve agents depends on the compound delivered, the dose that is delivered (LC), and the time (t) that an individual is exposed to that dose.
 There are three categories of biologic weapons (Table 53-1). Category A are those weapons which are highly contagious and fit all the characteristics of a relatively ideal biologic agent.
There are three categories of biologic weapons (Table 53-1). Category A are those weapons which are highly contagious and fit all the characteristics of a relatively ideal biologic agent.
Multimedia
 Disaster Preparedness
Disaster Preparedness
INTRODUCTION
Preparing to manage, to deal with the sequelae of, and to mitigate future disasters originating from natural events, industrial accidents or, of more interest recently, caused intentionally by terrorists using chemical, biologic, radiologic, nuclear, or high-yield explosive (CBRNE) agents is a high priority for the majority of governments the world over. Even large multinational corporations recognize the need for planning to assist during disasters and to decrease future risk of disasters. Two thousand such corporations, each with $5 billion or more in assets, participate in the World Economic Forum, a private not-for-profit foundation established in Switzerland. Through its Global Agenda Council on Humanitarian Assistance, partnering with the United Nations, humanitarian aid is provided throughout the world following natural disasters wherever there is a need. The resulting public–private collaboration has a distinguished track record; however, the Council recognizes the need to do more with respect to disaster risk reduction and disaster (www.weforum.org/issues/disaster-management). Money may also play a role—natural disasters that occurred in 2011 caused more than 350 billion dollars in losses (www.weforum.org/content/global-agenda-council-catastrophic-risks-2012). Whatever the reason, though, the aid provided is the only mechanism to mitigate the effects of disasters in many areas of the world where economic resources are inadequate. The United States also is cognizant of the benefits to its foreign policy by assisting in humanitarian missions. The U.S. Agency for International Development (USAID) spends a significant portion of its budget each year to provide humanitarian assistance in the wake of natural disasters such as floods, volcanic eruptions, and earthquakes but spends just as much to mitigate the effects of future catastrophes. The American Society of Anesthesiologists has recognized the importance of such activities and in the past decade has established a Committee on Emergency Preparedness and Trauma (COTEP) and a Global Health Initiative. While no one can doubt the altruistic motives for these actions, as a member-driven organization it has been driven in these endeavors from requests from members during this same time frame: After 9-11 strike, after Hurricanes Katrina and Ike, after the tornados that struck the central and southeast part of the country over the last couple years, and most recently after the earthquake that struck Haiti in 2010. ASA members who have been involved in relief efforts, members who have either been in the military or are in the military, and international members who have experienced terrorism on a more frequent basis have created a cacophony of voices calling for more education and training on how to prepare for a disaster and how to manage the victims of such disasters. Most residency program directors would agree that anesthesiologists are well prepared to manage individual patients but are lacking when it comes to education in managing the numbers of patients that might arise from a mass casualty event. Books have been written on such topics and governments have created large bureaucracies to address such events, so it would be naïve to think that a chapter in a book could adequately prepare one to cope with all contingencies . However, there are certain principles that are common to all such events, independent of their etiology, and as a group anesthesiologists are as well prepared if not better prepared to assist their communities in planning for and in caring for patients from a disaster. We must expend the energy to be better educated as the initial response to any disaster always occurs at the local level; therefore, as anesthesiologists we must be prepared to provide assistance during such emergencies. Other physicians, hospital administrators, and nongovernment organizations (NGOs) all place anesthesia providers at the top of the list of healthcare workers who are needed to manage the sequelae of natural disasters and mass casualty events. We are in such demand that the NGO, Doctors Without Borders (Medicins san Frontiers), waives its policy that clinicians commit for 9- to 18-month rotations; there is an option for anesthesia providers of 1- to 3-month assignments (www.doctorswithoutboarders.org/work/field/recruitment.cfn). Whether it is providing anesthesia so that an extremity can be amputated allowing someone trapped in the rubble of a building following an earthquake can be extracted, starting an intravenous infusion in a child or adult debilitated by diarrhea, treating the effects of a chemical agent, managing a ventilator in someone with anthrax, or providing anesthesia to a casualty from an explosion, anesthesia providers have the requisite skills to assist in all these scenarios—these are services we provide on a daily basis.
. However, there are certain principles that are common to all such events, independent of their etiology, and as a group anesthesiologists are as well prepared if not better prepared to assist their communities in planning for and in caring for patients from a disaster. We must expend the energy to be better educated as the initial response to any disaster always occurs at the local level; therefore, as anesthesiologists we must be prepared to provide assistance during such emergencies. Other physicians, hospital administrators, and nongovernment organizations (NGOs) all place anesthesia providers at the top of the list of healthcare workers who are needed to manage the sequelae of natural disasters and mass casualty events. We are in such demand that the NGO, Doctors Without Borders (Medicins san Frontiers), waives its policy that clinicians commit for 9- to 18-month rotations; there is an option for anesthesia providers of 1- to 3-month assignments (www.doctorswithoutboarders.org/work/field/recruitment.cfn). Whether it is providing anesthesia so that an extremity can be amputated allowing someone trapped in the rubble of a building following an earthquake can be extracted, starting an intravenous infusion in a child or adult debilitated by diarrhea, treating the effects of a chemical agent, managing a ventilator in someone with anthrax, or providing anesthesia to a casualty from an explosion, anesthesia providers have the requisite skills to assist in all these scenarios—these are services we provide on a daily basis.
However, disasters and mass casualty events are not something in which we participate on a daily basis so therefore education and training for these situations is critically important, beginning with preparation to respond to the most likely disasters to occur in our respective geographic location, for example, hurricanes on the Atlantic Seaboard and Gulf of Mexico, earthquakes on the West Coast of North America or tornadoes in the Midwest and Southeast of the United States. Even though natural and industrial disasters have occurred for millennia, the use of CBRNE agents and devices by terrorists in recent decades has emphasized the need for increased preparedness.
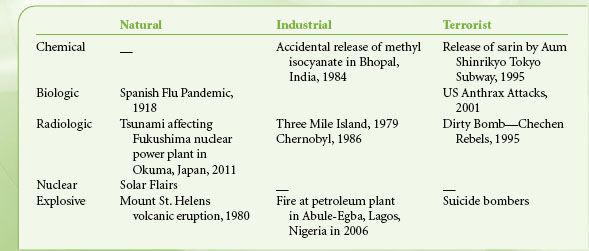
However, time and time again history shows that enthusiasm for education is high after an event and then tapers off; maintaining that enthusiasm is difficult,1 and therefore most if not all healthcare facilities2 are not prepared to deal with mass casualty incidents the exception being those facilities staffed by physicians with prior military training.3 In dealing with acts of terrorism geography is not helpful in anticipating what might occur, but that is not to say that one cannot anticipate what to expect. One can learn from experience; terrorists have been successful in their minds’ eyes with improvised explosive devices (IEDs), and even in those situations in which IEDs were not used, terrorists have chosen to use certain weapons of mass destruction (WMD) more often than others. For example, if they were to choose a chemical agent, a nerve agent is most likely and amongst those sarin has been the agent of choice. Similarly amongst biologic agents, anthrax, which was used in 2001, or smallpox would be the most likely choice because of the high lethality and infectivity associated with those two agents.4,5 Twice in the past 20 years “dirty” bombs have either been planned or planted (and fortunately not used) so such devices would be the most likely source of radiation used by terrorists. However, to underscore what was stated above based on past experience a natural or industrial event would be most likely (Table 53-1).
TABLE 53-1. EXAMPLES OF CBRNE EVENTS
To prepare for the kinds of scenarios described above, there are certain terms with which one must be familiar. A mass casualty incident is one that results in a number of patients that a community healthcare system has the resources to treat, despite turmoil and confusion. A mass casualty event is one that overwhelms the hospital or the community’s healthcare system. One also must be cognizant of the fact that though she or he might never plan to participate in a humanitarian mission overseas and therefore think that there is no need to train to work in an austere environment, depending on the circumstances of the disaster in which one finds one’s self the environment may be very austere indeed. Any time a situation arises in which medical capability is significantly below standards to which we are accustomed in the United States the anesthesiologist is indeed practicing in an austere environment . This austerity might occur in a:
. This austerity might occur in a:
 Mass casualty event in which the number of cases overwhelms capacity
Mass casualty event in which the number of cases overwhelms capacity
 Natural disaster in which the hospital is damaged or loses electricity or water
Natural disaster in which the hospital is damaged or loses electricity or water
 Disaster (natural/industrial/terrorist) in which care is provided on site
Disaster (natural/industrial/terrorist) in which care is provided on site
As described above, graduates of anesthesia training programs in North America can cope well in such situations, provided that they understand the basic requisites of disaster management, the focus of this chapter.
PREPARATION—PERSONAL PREPAREDNESS
Family Plan
In order to manage the numbers of casualties that would be expected during a mass casualty one must be prepared.6,7 Often overlooked during emergency preparedness and disaster management training is the development of a family plan and a personal preparedness plan. The former is important whether one is single or lives alone. Whether or not one has a pet, family, or friends living with them, or has legal responsibility for a loved one (elderly parents, disabled person) one must have a plan for these individuals that provides care for and information to loved ones . There are a number of websites that guide one through the creation of such a plan (Appendix I). During hurricane Katrina ∼35% of policemen and firemen did not show up for work—this should not come as a surprise to anyone.8 These individuals may have had to evacuate a parent in an assisted living facility or children in a day care center. Just as the military requires service members to have a family care plan (and a Will and Last Testament!), as a critically important healthcare provider we must have family care plans as well. However, if you know that you will be unavailable during a disaster then you have a responsibility to inform your employer or group of your personal situation. Even evacuation requires a plan. All family plans should include periodic family drills and updates. Plans might include situations such as what to do if there is a fire, what to do if parents do not make it home, the location of second copies of all important documents, where to meet if the house or neighborhood is destroyed or not accessible. Many assume that they will be able to communicate with loved ones during a disaster but often cell phone towers are damaged or so many people are trying to use the system that the network is overwhelmed. Plan in advance so that you are prepared for these contingencies.
. There are a number of websites that guide one through the creation of such a plan (Appendix I). During hurricane Katrina ∼35% of policemen and firemen did not show up for work—this should not come as a surprise to anyone.8 These individuals may have had to evacuate a parent in an assisted living facility or children in a day care center. Just as the military requires service members to have a family care plan (and a Will and Last Testament!), as a critically important healthcare provider we must have family care plans as well. However, if you know that you will be unavailable during a disaster then you have a responsibility to inform your employer or group of your personal situation. Even evacuation requires a plan. All family plans should include periodic family drills and updates. Plans might include situations such as what to do if there is a fire, what to do if parents do not make it home, the location of second copies of all important documents, where to meet if the house or neighborhood is destroyed or not accessible. Many assume that they will be able to communicate with loved ones during a disaster but often cell phone towers are damaged or so many people are trying to use the system that the network is overwhelmed. Plan in advance so that you are prepared for these contingencies.
And just as service members have a duffel bag or sea bag packed with toiletries, bedding, change of clothes, money, flash lights, and battery operated radio, those with such important roles as ours ideally should have a packed duffel bag as well. In a hurricane, earthquake, flood, tornado, or huge solar flair, loss of electric power is very likely. ATMs, gas pumps, toll booths and so on do not function without electricity—hence the need for some cash, flash lights, battery controlled radio (to stay abreast of the news)—and a vehicle that has a fuel tank that is not on empty!
Government Plan
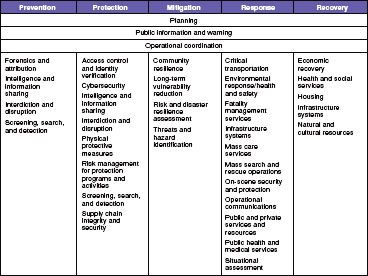
In September 2011, the United States Department of Homeland Security published its first edition of a 111-page document National Preparedness Goal.9 Figure 53-1 lists the multiple issues for which FEMA  must prepare, and with which agencies it must coordinate—with the United States Departments of Justice, of Health and Human Services, of Agriculture, of Commerce, and of Defense. Of note is that within the “Response” section, medical response is one of eleven for which the government has planned—a response which is under the auspices of the Department of Health and Human Services (DHHS). DHHS created and maintains a National Disaster Medical System (NDMS). Unfortunately, the system has not been adequately established and maintains. As highlighted by the US response to the earthquake in Haiti in 2010 the DHHS maintains only three International Medical Surgical Response Teams (IMSuRT), teams that were established with the idea that they would provide care to US citizens injured in areas of conflict. Unfortunately only one is funded and equipped and prior to Haiti, it had only been activated and used once—for the earthquake that occurred in 2003 in Bam, Iran.
must prepare, and with which agencies it must coordinate—with the United States Departments of Justice, of Health and Human Services, of Agriculture, of Commerce, and of Defense. Of note is that within the “Response” section, medical response is one of eleven for which the government has planned—a response which is under the auspices of the Department of Health and Human Services (DHHS). DHHS created and maintains a National Disaster Medical System (NDMS). Unfortunately, the system has not been adequately established and maintains. As highlighted by the US response to the earthquake in Haiti in 2010 the DHHS maintains only three International Medical Surgical Response Teams (IMSuRT), teams that were established with the idea that they would provide care to US citizens injured in areas of conflict. Unfortunately only one is funded and equipped and prior to Haiti, it had only been activated and used once—for the earthquake that occurred in 2003 in Bam, Iran.
FIGURE 53-1. Lists the multiple issues for which FEMA must prepare, and with which agencies it must coordinate.
Other teams that DHHS maintains in its NDMS in addition to the IMSuRTs are as follows:
Disaster Medical Assistance Team (DMAT)—a team that supposedly can rapidly mobilize and whose goal is to set up and staff with physicians, nurses and other support personnel emergency facilities and pharmaceutical dispensaries geographically as close as possible to a disaster. The teams are supposed to be self-sustaining for at least 72 hours before they require outside logistics. Just as the reserve military forces do, a DMAT is supposed to train 1 week-end a month. Not many surgeons and not many anesthesiologists have joined a DMAT as the team does not have the capacity to perform surgical procedures! Disaster Mortuary Team (DMORT) as the name implies is a team that would manage large numbers of dead following a mass casualty event with capacity to conduct forensic examinations. National Veterinary Response Team (NVRT) is a team established to provide veterinary services as well as zoonotic disease surveillance.
Most recently, the DHHS through its NDMS is planning and creating 15 Medical Specialty Enhancement Teams (MSETs). MSETsare going to consist of a group of precredentialed anesthesiologists and surgeons (30 of each), along with a few pediatricians. The concept is that there would be a pool of specialists who would be activated during a crisis, whether domestic or international, and would have sufficient logistic support that the team could deploy to either a fixed facility or a field site. Once activated MSET members would be federal employees during their deployments for a minimum of 2 weeks and would be protected by workers’ compensation laws, the federal tort claims act, and the Uniformed Services Employment and Reemployment Rights Act (USERRA). DHHS knows that many anesthesia providers do not have time for monthly drills or frequent call ups that the DMATs have. Although MSET members would be encouraged to train with DMATs, participation in an MSET will require far less of an investment in time. However, if activated, members of the teams would be expected to deploy or risk being dropped from the team and program. MSETs are a work in progress and many of the details of logistics and training are unanswered. It is hoped that once successfully established the size and number of teams could be expanded and the teams better developed to respond to future disasters, whether they be acts of nature or of terrorists. Please note however that as mentioned above, the initial response is local—such teams might take 2 or 3 days or longer to mobilize and deploy.
NGOs’ Plans
Ever since the anthrax attacks of 2000 and 2001, the destruction of the World Trade Center Towers on September 11, 2001, the SARS epidemic of 2004, and the continued devastation caused by nature (hurricanes, earthquakes, tornadoes, floods, and fires), The Joint Commission (TJC), the American Hospital Association, and state and county health departments have more closely monitored and evaluated hospitals’ and communities’ emergency preparedness. In 2003, TJC published its “Health Care at the Crossroads: Strategies for Creating and Maintaining Community-Wide Emergency Preparedness Systems”.10 The white paper has not been updated but emergency preparedness is one of the “standards” TJC uses to certify hospitals. Since 2003 it has hosted annual conferences, the most recent addressing how the two hospitals and their employees responded to the tornado that struck Joplin on May 20, 2011.11
TJC recognizes that there has been a change in healthcare delivery in the United States over the last several years and decades, reflective of similar problems faced worldwide, that has left the healthcare system under-funded with limited resources and ever increasing demand. Despite the best effort of law enforcement, fire and rescue teams, and emergency medical agencies, hospitals will continue to play a vital role in helping communities respond to catastrophic events , whether natural, unintentional, or terrorist-initiated. TJC was proactive in recognizing that, “It is no longer sufficient to develop disaster plans and dust them off if a threat appears imminent. Rather a system of preparedness across communities must be in place everyday”.10 The TJC acknowledged the need, despite decreasing healthcare resources, for what it describes as “surge capacity” within healthcare systems to handle the potentially hundreds, if not thousands or more, of patients who might be victims of catastrophic events. By planning and drilling, TJC hopes to reduce the appeal to terrorists of using WMD as an effective means of terrorism, and to help communities better respond to natural disasters. The white paper TJC published focused on three major areas:
, whether natural, unintentional, or terrorist-initiated. TJC was proactive in recognizing that, “It is no longer sufficient to develop disaster plans and dust them off if a threat appears imminent. Rather a system of preparedness across communities must be in place everyday”.10 The TJC acknowledged the need, despite decreasing healthcare resources, for what it describes as “surge capacity” within healthcare systems to handle the potentially hundreds, if not thousands or more, of patients who might be victims of catastrophic events. By planning and drilling, TJC hopes to reduce the appeal to terrorists of using WMD as an effective means of terrorism, and to help communities better respond to natural disasters. The white paper TJC published focused on three major areas:
I. Enlisting the community to develop the local response.
II. Focusing on the key aspects of the system that prepares the community to mobilize to care for patients, protect its staff, and serve the public.
III. Establishing the accountabilities, oversight, leadership, and sustainment of a community-preparedness system.
While the guidelines are just that—guidelines that are not mandatory nor required by law, all hospitals aspire to have TJC accreditation and from that perspective, the white paper was important in that hospitals do have biannual drills of their emergency preparedness and disaster management plans, sometimes coordinating with local law enforcement agencies and health departments and emergency medical response teams to create as realistic scenarios as possible. Unfortunately, the participation of anesthesia departments in these drills is often minimal. Drills are usually held on week days during working hours—because anesthesia departments are fully staffed and completely operational during those hours hospital administrators certify that they can handle the number of casualties coming through their ED; for financial reasons, the drills are not very realistic—surgical procedures are never canceled and the system is never tested at night or on weekends. At night when there is minimal telecommunications personnel in place how would a hospital mobilize its staff? Many have telephone “trees” but again because they are not tested many anesthesia providers have long since misplaced their contact information. Even if tested, how operational would the plan be during a major disaster when communication systems are overwhelmed? Short text communication would be the best way for departments to alert personnel to the disaster. Other advantages to having anesthesia departments actually participate in drills would be the establishment of trust with liaisons in the emergency response community and with local law enforcement agencies. How much better the outcome would have been if that had been the case in Moscow during the 2002 Nord-Ost siege when the Spetsnaz forces most likely used carfentanil against Chechen rebels without informing emergency response or hospital personnel resulting in 170 deaths.12
Impediments to the establishment of effective response plans are not only financial but also based on a lack of awareness of what occurs during a disaster. As Israelis know from their years of dealing with suicide bombers, and as the Japanese found out during the release of sarin by Aum Shinrikyo terrorist group in the Tokyo subway system in 1996, victims do NOT go to level I trauma centers, nor do they wait to be transported by emergency medical teams––they fan out in all directions to whatever healthcare facility they can find and they do so on foot, by private vehicles, by whatever means available.13 St. Luke’s hospital in Tokyo found itself inundated with close to 900 patients after the subway sarin attacks—its ED, lobby entrance—almost the entire first floor of the hospital was crammed with patients—none of whom had been decontaminated, and all of whom created a chaotic situation that was difficult to manage, and which delayed treatment for those who needed it most. The affected patients required treatment best understood by anesthesiologists who use cholinesterase inhibitors daily and best administered by intravenous lines inserted by these same providers. Furthermore, because of the size of most anesthesia departments, assuming 70% of providers will actually respond to a mass casualty event or disaster, there will be sufficient personnel for the providers to cover all the healthcare facilities operating suites (including obstetrical suites—a disaster has yet to occur that prevents pregnant women from going into labor and delivering). Other places anesthesia providers can assist in management of healthcare delivery during a disaster include:
 to assist in triage outside the hospital (who better to manage the pain or labored respiration of the expectant patient?),
to assist in triage outside the hospital (who better to manage the pain or labored respiration of the expectant patient?),
 to assist in decontamination (who better to evaluate for the presence of anticholinesterase (nerve) agents or cyanide toxicity),
to assist in decontamination (who better to evaluate for the presence of anticholinesterase (nerve) agents or cyanide toxicity),
 to assist with vascular access or airway management (made more difficult if wearing a HAZMAT suit and even more difficult if one has never worn such a suit), or to assist in ventilator management in the ICU or in overflow areas of the hospital such as the PACU of patients with respiratory failure caused by a nerve agent or biologic agent.
to assist with vascular access or airway management (made more difficult if wearing a HAZMAT suit and even more difficult if one has never worn such a suit), or to assist in ventilator management in the ICU or in overflow areas of the hospital such as the PACU of patients with respiratory failure caused by a nerve agent or biologic agent.
ROLE OF ANESTHESIOLOGIST IN MANAGING MASS CASUALTIES
It is difficult to anticipate every situation in which anesthesiologists could be asked to assist in managing mass casualty situations. For example, on October 26, 2002, terrorists held 750 hostages at the Nord-Ost Theater in Moscow. Many believe that the authorities instilled nebulized or volatile carfentanil into the air ducts of the opera house, thereby immobilizing the terrorists.12 Unfortunately, because of the incapacitating effect of carfentanil, the hostages became victims too. Patients were transported from the theater to hospitals without any treatment prior to arrival. Ideally, anesthesiologists or other healthcare providers with an opioid antagonist such as naloxone should have been readily available and present at the site to manage both hostages and the terrorists. Unfortunately, this was not the case.
Anesthesiologists’ basic understanding of physiology and pharmacology, their airway skills, their fluid resuscitation expertise, their ability to manage ventilators and to provide anesthesia in the field environment, in the emergency department, in the operating room, and in intensive care units (ICUs) will be invaluable . In these mass casualty situations, many patients suffer burns, fractures, lacerations, soft tissue trauma, and amputations that will require triage, stabilization in the emergency room or in some other facility near the emergency room, and either more definitive treatment in the operating room or in the ICU.
. In these mass casualty situations, many patients suffer burns, fractures, lacerations, soft tissue trauma, and amputations that will require triage, stabilization in the emergency room or in some other facility near the emergency room, and either more definitive treatment in the operating room or in the ICU.
During a mass casualty incident an anesthesiologist may well be asked to provide anesthetic services in an area other than the operating room or ICU. One will not know where one will be working until reporting to the hospital and the command and control center established to manage the incident.14 The site of the command and control center is pre-established and outlined in the hospital’s emergency preparedness plan, but typically within the hospital’s emergency department or in close proximity. Other entrances to the hospital are typically closed during a mass casualty incident for the purposes of maintaining control of the numbers of patients that might present and to allow for decontamination of patients if necessary avoiding exposure of hospital personnel to contagious agents or transferrable substances such as nerve agents. The lack of such control and decontamination of the Tokyo subway sarin attack victims in 1995 resulted in a number of healthcare workers becoming ill by absorbing sarin from patients who had not been properly decontaminated.13 Not only were they unable to work but they became patients themselves, increasing the number of patients requiring care and consuming resources.
Triage
If assigned to triage patients, the anesthesiologist will be expected to classify patients into four groups—those requiring immediate care, delayed care, first aid, and expectant . The latter group includes those expected not to survive, or, because of the number of patients arriving, those for whom there are not adequate personnel or resources to adequately resuscitate without jeopardizing the lives of many more patients who would not receive the care they require and for whom the prognosis is more favorable. Experience has taught that initially triage officers are “conservative”—they try to save as many as possible, but over days, if not hours they gain experience and become better at identifying patients for whom resources exist to improve outcome. In the future, biotechnology may play a role15 but at present hospitals must rely on physicians’ experience and again because of their knowledge of the hospitals resources—in the OR and ICU they may well be the ideal triage officer. He or she will have to assess and decide if patients fall into one of the four groups. “Expectant” patients are usually transported to an area separate from the ED where they can be provided comfort care, such a site must be situated such that newly arriving patients are not exposed to the sight of dying patients. Anesthesiologists may well be assigned to provide such care because of expertise in managing airways, in establishing intravenous access for the administration of medications, and our familiarity with the available anxiolytic and analgesic medications. As emotionally difficult as the process might be of identifying or managing patients not expected to survive is the assessment of patients who may have been injured or been affected during a disaster but do not appear to require treatment, but who might require delayed care. Depending on the agent, diagnosis of those requiring therapy:
. The latter group includes those expected not to survive, or, because of the number of patients arriving, those for whom there are not adequate personnel or resources to adequately resuscitate without jeopardizing the lives of many more patients who would not receive the care they require and for whom the prognosis is more favorable. Experience has taught that initially triage officers are “conservative”—they try to save as many as possible, but over days, if not hours they gain experience and become better at identifying patients for whom resources exist to improve outcome. In the future, biotechnology may play a role15 but at present hospitals must rely on physicians’ experience and again because of their knowledge of the hospitals resources—in the OR and ICU they may well be the ideal triage officer. He or she will have to assess and decide if patients fall into one of the four groups. “Expectant” patients are usually transported to an area separate from the ED where they can be provided comfort care, such a site must be situated such that newly arriving patients are not exposed to the sight of dying patients. Anesthesiologists may well be assigned to provide such care because of expertise in managing airways, in establishing intravenous access for the administration of medications, and our familiarity with the available anxiolytic and analgesic medications. As emotionally difficult as the process might be of identifying or managing patients not expected to survive is the assessment of patients who may have been injured or been affected during a disaster but do not appear to require treatment, but who might require delayed care. Depending on the agent, diagnosis of those requiring therapy:
 Chemical (nerve) agents: If only headache, meiosis, rhinorrhea, and lacrimation after exposure, patients can be decontaminated (see later) and dismissed. Patients with dyspnea, bronchospasm, or arrhythmias will require treatment with atropine.
Chemical (nerve) agents: If only headache, meiosis, rhinorrhea, and lacrimation after exposure, patients can be decontaminated (see later) and dismissed. Patients with dyspnea, bronchospasm, or arrhythmias will require treatment with atropine.
 Biologic agents: Fever, rash, dyspnea, cough
Biologic agents: Fever, rash, dyspnea, cough
 Radiation/nuclear: Nausea within 6 hours of exposure; because of the prevalence for those with this symptom, check leukocyte count, dismiss, and have the patient return in 48 hours for repeat check—if no change in count, no therapy is indicated.
Radiation/nuclear: Nausea within 6 hours of exposure; because of the prevalence for those with this symptom, check leukocyte count, dismiss, and have the patient return in 48 hours for repeat check—if no change in count, no therapy is indicated.
 Explosive: If tympanic membranes are intact and SpO2 is within normal limits, other injuries are unlikely.
Explosive: If tympanic membranes are intact and SpO2 is within normal limits, other injuries are unlikely.
Decontamination
In most situations, people in contact with chemical agents or radioactive materials are decontaminated by those with proper training—the decontamination is normally performed first and then patients are evaluated and triaged. The process is usually fairly straightforward; clothes are removed and individuals are washed with copious amounts of water (the contaminated water and apparel can present quite a challenge!); if individuals have been exposed to a chemical agent, a dilute solution of sodium hypochlorite 0.5% (household bleach) can be used.
However, if the patient presents with life-threatening injury, the patient is treated first and decontaminated afterward. Patients with severe chemical agent poisoning may present with acute respiratory failure requiring emergency tracheal intubation. In this scenario, an anesthesiologist would be assigned to the decontamination station. For obvious reasons the intubation would have to be performed with the anesthesiologist wearing a hazard material (HAZMAT) or a biohazard suit with multiple-layered gloves and a gas mask. The suits are not insulated and if the decontamination is performed outside the hospital the extremes of temperature can significantly hinder performance, as does the decreased manual dexterity because of the gloves and the impairment in vision from the face hoods. Ideally individuals with prior training would manage the airway intubation but depending on circumstances that may not happen. As many have learned from the past experience, it is best to anticipate the unexpected, and to be flexible if the maximum numbers of patients are to be saved. Preparation of equipment and drugs before the arrival of contaminated patients decreases the difficulties with manual dexterity that are encountered while wearing the multiple-layered or rubber gloves. Consider securing the airway with a laryngeal mask airway, when indicated, rather than with a tracheal tube.
Emergency Department
Another place where an anesthesiologist might be assigned is the emergency department. While some level I trauma centers have an anesthesia team assigned to support the emergency department, this is not the norm. Depending on the types of casualties, but especially for casualties from a violent explosion, anesthesiologists might be assigned to manage the airway and secure central venous access.  Anesthesiologists should position themselves at the head of the bed and assume responsibility for the airway and venous access. For the former, it would be ideal to have two or three assistants (one providing in-line C-spine stabilization, another individual applying cricoid pressure, and a third individual administering medications.) Sometimes it is necessary to remind emergency room physicians and trauma surgeons that “A” (airway) and “B” (breathing) come before “C” (circulation); certainly, the primary and secondary surveys can be conducted during this critical time point but ventilation and oxygenation must be assured.
Anesthesiologists should position themselves at the head of the bed and assume responsibility for the airway and venous access. For the former, it would be ideal to have two or three assistants (one providing in-line C-spine stabilization, another individual applying cricoid pressure, and a third individual administering medications.) Sometimes it is necessary to remind emergency room physicians and trauma surgeons that “A” (airway) and “B” (breathing) come before “C” (circulation); certainly, the primary and secondary surveys can be conducted during this critical time point but ventilation and oxygenation must be assured.
In previous industrial accidents and fires, appropriate management of the airway has been critical. Patients with large-area burns will require establishment of intravenous access for provision of intravascular volume resuscitation. Depending on the event (burn vs. a crush injury—protocols for fluid resuscitation vary), in patients with extensive soft tissue and skeletal muscle damage, alkalinization of the urine with volume resuscitation and diuresis may be organ-and life-saving. If chemical weapons are also used, again depending on the severity of the injury, not only may tracheal intubation be required, but ventilator management may be necessary.
The remainder of this chapter review the four major types of agents available to terrorists, recognizing that similar injuries can be caused by industrial catastrophes (thousands of deaths and injuries from methyl isocyanate in Bhopal, India, December 1984) or natural disasters (radiation exposure as a result of the tsunami that hit Japan in 2011).
CHEMICAL
Nerve Agents
Prior to the last century, it was unthinkable that rogue states or terrorists would use chemical agents. During the first World War, more than one million soldiers and civilians were exposed to chemical gas injuries with over 100,000 of them dying. In 1935, Italy invaded Abyssinia (Ethiopia) and during that invasion, sprayed mustard gas from aircrafts. When Japan invaded China in 1937, mustard gas, phosgene, and hydrogen cyanide were used. In that same year, German chemical laboratories produced the first nerve agent, tabun. During 1963 to 1967, Egypt used phosgene and mustard agents in support of South Yemen during the civil war in that country. When Iraq attacked Iran in the 1980s, mustard gas and nerve agents were used. In all these examples, chemical agents were used by the military during armed conflict. The governments mentioned above have all signed in the Chemical Weapons Convention. January 2012 marked the end of an era as the United States, in compliance with the Chemical Weapons Convention ratified by the Senate in 1997, the U.S. Army Chemical Materials Agency completed destruction of 27,000 tons of chemical weapons that it had manufactured and stored over the years.16
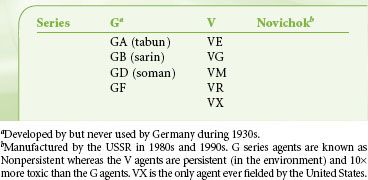
However, as one era ended another one had already begun. In 1994 and 1995, the use of the nerve agent, sarin, by the Japanese cult Aum Shinrikyo was a major turning point for it was the first time that a terrorist group had used a nerve agent in a terrorist attack. More than 5,000 persons were evaluated at hospitals of whom approximately 1,000 had been exposed to the nerve agent and 18 died. There is no doubt in anyone’s mind that chemical agents will be used again in the future. The nerve agents are so named because of their mechanism of action (Table 53-2).
TABLE 53-2. TOXICITY OF NERVE AGENTS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






