The restricted spaces in the airway require an understanding and cooperative relationship between surgeon and anesthesiologist, and the use of specially adapted equipment suitable to these cramped areas.
 Despite only mild-to-moderate tonsillar enlargement on physical examination, children with obstructive sleep apnea have upper airway obstruction while awake and apnea during sleep. The clinician should not underestimate the severity of the problem based on tonsillar size alone.
Despite only mild-to-moderate tonsillar enlargement on physical examination, children with obstructive sleep apnea have upper airway obstruction while awake and apnea during sleep. The clinician should not underestimate the severity of the problem based on tonsillar size alone.
 Post-tonsillectomy hemorrhage may result in unappreciated large volumes of swallowed blood originating from the tonsillar fossa. These patients must be considered to have a full stomach, and anesthetic precautions addressing this situation must be taken.
Post-tonsillectomy hemorrhage may result in unappreciated large volumes of swallowed blood originating from the tonsillar fossa. These patients must be considered to have a full stomach, and anesthetic precautions addressing this situation must be taken.
 The middle ear and sinuses are air-filled, nondistensible cavities. During procedures in which the eardrum is replaced or perforation is patched, nitrous oxide should be discontinued or, if this is not possible, limited to a maximum of 50% during the application of the tympanic membrane graft to avoid pressure-related displacement.
The middle ear and sinuses are air-filled, nondistensible cavities. During procedures in which the eardrum is replaced or perforation is patched, nitrous oxide should be discontinued or, if this is not possible, limited to a maximum of 50% during the application of the tympanic membrane graft to avoid pressure-related displacement.
 Systemic absorption of vasoconstrictive agents during FESS surgical procedures may cause hypertension, bradycardia, tachycardia, and arrhythmias. Preoperative evaluation should include a thorough investigation of the patient’s cardiovascular status. Rapid response by the anesthesiologist to these effects is necessary in preventing complications.
Systemic absorption of vasoconstrictive agents during FESS surgical procedures may cause hypertension, bradycardia, tachycardia, and arrhythmias. Preoperative evaluation should include a thorough investigation of the patient’s cardiovascular status. Rapid response by the anesthesiologist to these effects is necessary in preventing complications.
 Prior radiation therapy may lead to fibrosis and ankylosis in the temporomandibular joint, rendering orotracheal intubation difficult.
Prior radiation therapy may lead to fibrosis and ankylosis in the temporomandibular joint, rendering orotracheal intubation difficult.
 Prior to extubation after temporomandibular arthroscopy, the oral cavity and neck must be examined carefully to rule out the presence of extracapsular extravasation of irrigation fluid. Extravasation can lead to airway closure.
Prior to extubation after temporomandibular arthroscopy, the oral cavity and neck must be examined carefully to rule out the presence of extracapsular extravasation of irrigation fluid. Extravasation can lead to airway closure.
 After extensive facial trauma or resection of tumors of the upper airway, it is prudent to keep the patient’s trachea intubated until edema has subsided. Extraoral facial edema should lead the physician to suspect intraoral edema and possible airway compromise.
After extensive facial trauma or resection of tumors of the upper airway, it is prudent to keep the patient’s trachea intubated until edema has subsided. Extraoral facial edema should lead the physician to suspect intraoral edema and possible airway compromise.
Multimedia
 Airway Abscess
Airway Abscess
 Facial Nerve
Facial Nerve
 Jet Ventilation
Jet Ventilation
 Epiglottis
Epiglottis
 Laser ENT
Laser ENT
 Tracheostomy
Tracheostomy
EVALUATING THE AIRWAY
Air flows through the upper respiratory passages, into the trachea, bronchi, bronchioles, and into alveoli in the healthy human. Air flow occurs seemingly without either thought or effort, and the actual work of respiration in the unobstructed airway is minimal. However, airway obstruction due to malformation, tumor, infection, or trauma may significantly alter the clinical presentation and make gas exchange a laborious, energy-consuming process. The increased work of breathing can leave the patient exhausted, incapable of maintaining adequate gas exchange, and finally succumbing to ventilatory failure. Significant obstruction and anatomic distortion may be present in a patient with minimal evidence of disease because clinically evident upper airway obstruction is a late sign. It is a most unwelcome experience for the anesthesiologist to unexpectedly discover an obstructed upper airway at the time of attempted tracheal intubation.
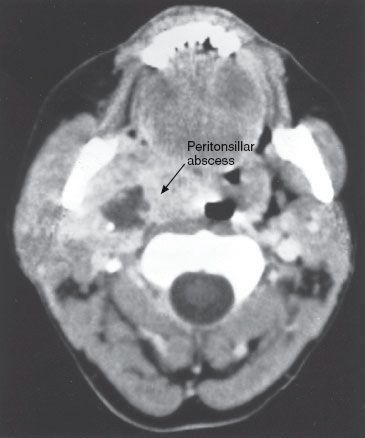
In the presence of tumor, other mass lesions, or infection in the airway, it may be useful to obtain radiologic evaluation of the airway with plain films of the tracheal and laryngeal air columns or computed tomography and MRI studies of the airway. Significant anatomic distortion is usually evident and may help the anesthesiologist determine the most appropriate technique for securing the airway.
ANESTHESIA FOR PEDIATRIC EAR, NOSE, AND THROAT SURGERY
 The safe management of the pediatric patient undergoing surgery of the ear, nose, and throat is particularly challenging to the anesthesiologist. The restricted spaces in the airway of the child require an understanding and cooperative relationship between surgeon and anesthesiologist, and the use of specially adapted equipment suitable to these cramped areas.
The safe management of the pediatric patient undergoing surgery of the ear, nose, and throat is particularly challenging to the anesthesiologist. The restricted spaces in the airway of the child require an understanding and cooperative relationship between surgeon and anesthesiologist, and the use of specially adapted equipment suitable to these cramped areas.
Tonsillectomy and Adenoidectomy
Untreated adenoidal hyperplasia may lead to nasopharyngeal obstruction, causing failure to thrive, speech disorders, obligate mouth breathing, sleep disturbances, orofacial abnormalities with a narrowing of the upper airway, and dental abnormalities. Surgical removal of the adenoids is usually accompanied by tonsillectomy; however, purulent adenoiditis, despite adequate medical therapy, and recurrent otitis media with effusion secondary to adenoidal hyperplasia are improved with adenoidectomy alone.
Tonsillectomy is one of the more commonly performed pediatric surgical procedures.1 Chronic or recurrent acute tonsillitis, peritonsillar abscess, tonsillar hyperplasia, and obstructive sleep apnea syndrome are the major indications for surgery.2–4 In addition, patients with cardiac valvular disease are at risk for endocarditis from recurrent streptococcal bacteremia secondary to infected tonsils. Tonsillar hyperplasia may lead to chronic airway obstruction resulting in sleep apnea, carbon dioxide (CO2) retention, cor pulmonale, failure to thrive, swallowing disorders, and speech abnormalities. These risks are eliminated with removal of the tonsils.
Obstruction of the oropharyngeal airway by hypertrophied tonsils leading to apnea during sleep is an important clinical entity referred to as obstructive sleep apnea syndrome. Despite only mild-to-moderate tonsillar enlargement on physical examination, these patients have upper airway obstruction while awake and apnea during sleep. The goals of treatment are to relieve airway obstruction and increase the cross-sectional area of the pharynx, which is successful in two-thirds of pediatric cases.5 Some patients require the use of nasal continuous positive airway pressure during sleep, whereas others may require a tracheostomy to bypass the chronic upper airway obstruction that is present. The two most frequent levels of obstruction during sleep are at the soft palate and the base of the tongue.6 Most children have tremendous improvement in their symptoms after tonsillectomy.
In children with long-standing hypoxemia and hypercarbia, increased airway resistance can lead to cor pulmonale (Fig. 47-1). Patients have electrocardiographic evidence of right ventricular hypertrophy, with one-third of them having chest radiographs consistent with cardiomegaly. Each apneic episode causes progressively increasing pulmonary artery pressure with significant systemic and pulmonary artery hypertension, leading to ventricular dysfunction and cardiac dysrhythmias.7 These patients often have dysfunction in the medulla or hypothalamic areas of the central nervous system causing persistently elevated CO2, despite relief of airway obstruction. This group of patients has a hyperreactive pulmonary vascular bed, and the increased pulmonary vascular resistance and myocardial depression in response to hypoxia, hypercarbia, and acidosis are far greater than what is expected for that degree of physiologic alteration in the normal population. Cardiac enlargement is frequently reversible with digitalization and surgical removal of the tonsils and adenoids.
FIGURE 47-1. Events leading to cor pulmonale.

Preoperative Evaluation
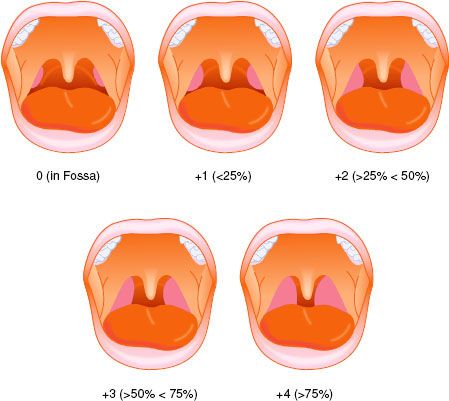
A thorough history is the basis for the preoperative evaluation. Because patients requiring tonsillectomy and adenoidectomy have frequent infections, the parent should be questioned for current use of antibiotics, antihistamines, or other medicines. A history of sleep apnea should be sought. The physical examination should begin with observation of the patient. The presence of audible respirations, mouth breathing, nasal quality of the speech, and chest retractions should be noted. Mouth breathing may be the result of chronic nasopharyngeal obstruction. An elongated face, retrognathic mandible, and a high-arched palate may be present.8 The oropharynx should be inspected for evaluation of tonsillar size to determine the ease of mask ventilation and tracheal intubation (Fig. 47-2). The presence of wheezing or rales on auscultation of the chest may be a lower respiratory manifestation of pharyngitis or tonsillitis. The presence of inspiratory stridor or prolonged expiration may indicate partial airway obstruction from hypertrophied tonsils or adenoids.
FIGURE 47-2. Classification of tonsil size, including percentage of oropharyngeal area occupied by hypertrophied tonsils.
Measurement of hematocrit and coagulation parameters is suggested. Many nonprescription cold medications and antihistamines contain aspirin, which may affect platelet function, and this potential anticoagulation should be taken into consideration. Chest radiographs and electrocardiograms (ECGs) are not required unless specific abnormalities are elicited during the history, such as recent pneumonia, bronchitis, upper respiratory infection (URI), or history consistent with cor pulmonale, which is seen in children with obstructive sleep apnea syndrome. In those children with a history of cardiac abnormalities, an echocardiogram may be indicated.
Sleep Disordered Breathing and Obstructive Sleep Apnea
Sleep disordered breathing (SDB) is a spectrum of disorders ranging from primary snoring to obstructive sleep apnea syndrome (OSAS). SDB affects 10% of the population but only 1% to 4% will progress to OSAS. OSAS is characterized by periodic, partial, or complete obstruction of the upper airway during sleep.9–11 Proper screening and diagnosis of obstructive sleep apnea prior to surgery for both children and adults is essential in reducing the associated risks. The STOP questionnaire has been developed as a tool to screen adult patients for obstructive sleep apnea and includes information on Snoring, daytime somnolence and Tiredness, Observation of apnea during sleep and elevations in blood Pressure. Predicting risk in children, however, is far more complicated.12,13
Repetitive arousal from sleep to restore airway patency is a common feature as are episodic sleep-associated oxygen desaturation, hypercarbia, and cardiac dysfunction as a result of airway obstruction. Individuals who experience obstruction during sleep may have snoring loud enough to be heard through closed doors or observed pauses in breathing during sleep. They may awaken from sleep with a choking sensation. Parents report restless sleep in affected children and frequent somnolence or fatigue while awake despite adequate sleep hours. These children fall asleep easily in nonstimulating environments and are difficult to arouse at usual awakening time. Type 1 OSAS is characterized by lymphoid hyperplasia without obesity whereas type 2 OSAS patients are obese with minimal lymphoid hyperplasia. Approximately 10% of OSAS is present in preschool and school-aged children and is thought to decline after 9 years of age.
 Obesity changes craniofacial anthropometric characteristics. Therefore, a body mass index of 95% for age or greater is a predisposing physical characteristic that increases the risk of developing OSAS.14 Children with craniofacial abnormalities including a small maxilla and mandible, a large tongue for a given mandibular size, and a thick neck have a similar increased risk. Many of these children have syndromes which are associated with additional comorbidities. Anatomic nasal obstruction and Class 4 touching tonsils reduce oropharyngeal cross-sectional area which constitutes an additional risk. Pharyngeal size is determined by the soft-tissue volume inside the bony enclosure of the mandible; an anatomic imbalance between the upper airway soft-tissue volume and craniofacial size will result in obstruction. The magnitude of pharyngeal muscle contraction is controlled by neural mechanisms and the interaction between the anatomical balance and neural mechanisms determines pharyngeal airway size. Increased neural mechanisms can compensate the anatomical imbalance in obstructive sleep apnea patients during wakefulness. When these neural mechanisms are suppressed during sleep or anesthesia, pharyngeal dilator muscles do not contract maximally and therefore the pharyngeal airway severely narrows because of the anatomical imbalance. Increasing bony enclosure size will provide relief of airway obstruction. This is only accomplished surgically by mandibular advancement. Increasing the distance between the mentum and the cervical column by positioning will transiently relieve the obstruction as long as the sniffing position is maintained. Similarly, the sitting position displaces excessive soft tissue outside the bony enclosure through the submandibular space.
Obesity changes craniofacial anthropometric characteristics. Therefore, a body mass index of 95% for age or greater is a predisposing physical characteristic that increases the risk of developing OSAS.14 Children with craniofacial abnormalities including a small maxilla and mandible, a large tongue for a given mandibular size, and a thick neck have a similar increased risk. Many of these children have syndromes which are associated with additional comorbidities. Anatomic nasal obstruction and Class 4 touching tonsils reduce oropharyngeal cross-sectional area which constitutes an additional risk. Pharyngeal size is determined by the soft-tissue volume inside the bony enclosure of the mandible; an anatomic imbalance between the upper airway soft-tissue volume and craniofacial size will result in obstruction. The magnitude of pharyngeal muscle contraction is controlled by neural mechanisms and the interaction between the anatomical balance and neural mechanisms determines pharyngeal airway size. Increased neural mechanisms can compensate the anatomical imbalance in obstructive sleep apnea patients during wakefulness. When these neural mechanisms are suppressed during sleep or anesthesia, pharyngeal dilator muscles do not contract maximally and therefore the pharyngeal airway severely narrows because of the anatomical imbalance. Increasing bony enclosure size will provide relief of airway obstruction. This is only accomplished surgically by mandibular advancement. Increasing the distance between the mentum and the cervical column by positioning will transiently relieve the obstruction as long as the sniffing position is maintained. Similarly, the sitting position displaces excessive soft tissue outside the bony enclosure through the submandibular space.
The long-term effects of OSAS are not limited to the airway. These children have other systemic comorbidities. Increased body mass index and obesity may lead to increased cognitive vulnerability as illustrated by the increased frequency of hyperactivity and increased levels of C-reactive protein. The duration of OSA has no relation to reversibility of neurobehavioral impairment since many believe that episodic hypoxia alters the neurochemical substrate of the prefrontal cortex causing neuronal cell loss. Metabolic syndrome consists of insulin resistance, dyslipidemia, and hypertension. It is felt that OSAS is a risk factor for metabolic syndrome in obese children but not in nonobese patients. Cardiovascular and hemodynamic comorbidities are more common in OSAS patients. These consist of altered regulation of blood pressure as well as alterations in sympathetic activity and reactivity. Also present are endothelial dysfunction and initiation and propagation of inflammatory response facilitated by increases in levels of C-reactive protein. Systemic inflammation using interleukins as a marker is a component of OSAS in both obese and nonobese children and is reversed after tonsillectomy. Systemic hypertension, changes in left ventricular geometry, and intermittent hypoxia leading to pulmonary artery hypertension are well-described comorbidities present in patients with OSAS.
The mainstay of the management is surgical removal of tonsils and adenoids which carries an 85% success rate in resolving OSAS. Recurrence may occur in children with craniofacial abnormalities and in others. If surgical intervention does not resolve the problem, nocturnal CPAP is the next treatment modality. However, many of these children may present for imaging studies or require sedation prior to removal of the tonsils or adenoids.
Anesthetic Management
The goals of the anesthetic management for tonsillectomy and adenoidectomy are to render the child unconscious in the most atraumatic manner possible, to provide the surgeon with optimal operating conditions, to establish intravenous access to provide a route for volume expansion and medications when necessary, and to provide rapid emergence so that the patient is awake and able to protect the recently instrumented airway. Premedication may be used as determined by the anesthesiologist during the preanesthetic visit. Sedative premedication should be avoided in children with obstructive sleep apnea, intermittent obstruction, or very large tonsils. Administration of opiates to patients with obstructive sleep apnea is associated with an increased risk of oxygen desaturation secondary to chronic hypoxemia and alterations in respiratory control.15 Use of an antisialagogue will minimize secretions in the operative field.
Anesthesia is commonly induced with a volatile anesthetic agent, oxygen, and nitrous oxide (N2O) by mask. Parental presence in the operating room (OR) during mask induction may be helpful in the anxious unpremedicated child. Tracheal intubation is best accomplished under deep inhalation anesthesia or aided by a short-acting nondepolarizing muscle relaxant. Many clinicians may choose to eliminate the neuromuscular blocking agent in favor of enhancing the depth of anesthesia with the use of propofol. The addition of 0.5 to 1 mg/kg of dexmedetomidine infused during the procedure may help to attenuate emergence delirium in toddlers at the conclusion of the anesthetic.16 Blood in the pharynx may enter the trachea during the surgical procedure. For this reason, the supraglottic area may be packed with petroleum gauze, or a cuffed endotracheal tube may be used. If a cuffed endotracheal tube is selected, careful attention to the inflation pressure of the cuff is essential if postextubation croup is to be avoided. Monitoring consists of precordial stethoscope, ECG, automated blood pressure, pulse oximetry, and end-tidal capnography.
Emergence from anesthesia should be rapid, and the child should be alert before transfer to the recovery area. The child should be awake and able to clear blood or secretions from the oropharynx as efficiently as possible before removal of the endotracheal tube. Maintenance of airway and pharyngeal reflexes is essential in the prevention of aspiration, laryngospasm, and airway obstruction. There is no difference in the incidence of airway complications on emergence between patients who are extubated awake or deeply anesthetized.17
The use of the laryngeal mask airway (LMA) for adenotonsillectomy was described in 1990; however, it was not until the widespread availability of a streamlined flexible model that it was routinely used for this purpose.18,19 There is an emerging trend to use the flexible LMA for tonsillectomy, which protects the vocal cords from blood or secretions that may be present in the oropharynx.20 The wide, rigid tube of the standard LMA model does not fit under the mouth gag and is easily compressed or dislodged during full mouth opening. The flexible model has a soft, reinforced shaft that easily fits under the mouth gag without becoming dislodged or compressed. Adequate surgical access can be achieved, and the lower airway is protected from exposure to blood during the procedure.21,22 Since the cuff is larger and occupies a greater percentage of the posterior hypopharynx, there is a greater risk of airway fire if the electrocautery touches the LMA. Insertion is possible after either the intravenous administration of 3 mg/kg of propofol or when sufficient depth of anesthesia is achieved using a volatile agent administered by face mask. The same depth of anesthesia should be obtained during insertion of the LMA as would be required for performing laryngoscopy and endotracheal intubation. Positive-pressure ventilation should be avoided when the LMA is used during tonsillectomy, although gentle assisted ventilation is both safe and effective if peak inspiratory pressure is kept below 20 cm H2O.
Tonsillar enlargement can make LMA insertion difficult; care in placement is essential.23 Maneuvers to overcome this difficulty include increased head extension, lateral insertion of the mask, anterior displacement of the tongue, pressure on the tip of the LMA using the index finger as it negotiates the pharyngeal curve, or use of the laryngoscope if all else fails. Dislodgment of the device does not occur during extreme head extension, assuming good position and ventilation were obtained before changes in head position.24
Advantages of the LMA over traditional endotracheal intubation are a decrease in the incidence of postoperative stridor and laryngospasm and an increase in immediate postoperative oxygen saturation. If the child is breathing spontaneously at a regular rate and depth, the LMA may be removed before emergence from anesthesia. The oropharynx should be gently suctioned with a soft, flexible catheter, the LMA deflated and removed, an oral airway inserted, and the respirations assisted with 100% oxygen delivered by face mask. It is often distressing for young children to awaken with the LMA still in place. Although the device is an appropriate substitute for an oral airway in the adult population, this is not so in children. If the practitioner wants to remove the LMA when the child has emerged from anesthesia, it should be deflated and removed as soon as possible after the return to consciousness. In addition, because it is not possible to pass a nasogastric tube beyond the LMA cuff even when deflated, the stomach cannot be emptied at the conclusion of surgery.
Complications
The incidence of emesis after tonsillectomy ranges from 30% to 65%.25 Whether emesis is due to irritant blood in the stomach or stimulation of the gag reflex by inflammation and edema at the surgical site remains unclear. Central nervous system stimulation from the gastrointestinal tract, as may be seen with gastric distention from the introduction of swallowed or insufflated air, may trigger the emetic center. Decompressing the stomach with an orogastric tube may be helpful in preventing this response. Treatment with ondansetron, 0.10 to 0.15 mg/kg, either with or without dexamethasone, 0.5 mg/kg, has been shown to be very effective in reducing post-tonsillectomy nausea and vomiting.26–28 Postoperative administration of meperidine increases the probability of emesis, and alternative analgesic agents should be administered. Dehydration secondary to poor oral intake as a result of nausea, vomiting, or pain can occur after tonsillectomy in 1% of cases. Vigorous intravenous hydration during surgery can offset the physiologic effects of lower postoperative fluid intake.
 The most serious complication of tonsillectomy is postoperative hemorrhage, which occurs at a frequency of 0.1% to 8.1%. The recent utilization of coblation tonsillectomy may result in an incidence of post-tonsillectomy hemorrhage up to 11.1%.4,29,30 Approximately 75% of postoperative tonsillar hemorrhage occurs within 6 hours of surgery. Most of the remaining 25% occurs within the first 24 hours of surgery, although bleeding may be noted until the sixth postoperative day.31,32 Sixty-seven percent of postoperative bleeding originates from the tonsillar fossa, 26% in the nasopharynx, and 7% in both. Initial attempts to control bleeding may be made using pharyngeal packs and cautery. If this fails, patients must return to the OR for exploration and surgical hemostasis.
The most serious complication of tonsillectomy is postoperative hemorrhage, which occurs at a frequency of 0.1% to 8.1%. The recent utilization of coblation tonsillectomy may result in an incidence of post-tonsillectomy hemorrhage up to 11.1%.4,29,30 Approximately 75% of postoperative tonsillar hemorrhage occurs within 6 hours of surgery. Most of the remaining 25% occurs within the first 24 hours of surgery, although bleeding may be noted until the sixth postoperative day.31,32 Sixty-seven percent of postoperative bleeding originates from the tonsillar fossa, 26% in the nasopharynx, and 7% in both. Initial attempts to control bleeding may be made using pharyngeal packs and cautery. If this fails, patients must return to the OR for exploration and surgical hemostasis.
Unappreciated large volumes of blood originating from the tonsillar bed may be swallowed. These patients must be considered to have a full stomach, and anesthetic precautions addressing this situation must be taken. A rapid-sequence induction accompanied by cricoid pressure and a styletted endotracheal tube is controversial but may be of benefit in some circumstances. Because the amount of blood swallowed can be considerable, blood pressure must be checked in both the erect and supine positions to exclude orthostatic changes resulting from decreases in vascular volume. Intravenous access and hydration must be established before the induction of anesthesia. A variety of laryngoscope blades and endotracheal tubes, as well as functioning suction apparatus, should be prepared in duplicate because blood in the airway may impair visualization of the vocal cords and cause plugging of the endotracheal tube.
Pain after adenoidectomy is usually minimal, but pain after tonsillectomy is severe. This contributes to poor fluid intake and overall discomfort of patients. An increase in postoperative pain medication requirements has been noted in patients having laser or electrocautery as part of the operative tonsillectomy compared with those who have had sharp surgical dissection and ligation of blood vessels to achieve hemostasis.7,33 Intraoperative administration of corticosteroids may decrease edema formation and subsequent patient discomfort. Although infiltration of the peritonsillar space with local anesthetic and epinephrine has been shown to be effective in reducing intraoperative blood loss, it does not decrease postoperative pain.
Peritonsillar abscess, or quinsy tonsil, is a condition that may require immediate surgical intervention to relieve potential or existing airway obstruction. An acutely infected tonsil may undergo abscess formation, producing a large mass in the lateral pharynx that can interfere with swallowing and breathing (Figs. 47-3–47-5). Fever, pain, and trismus are frequent symptoms. Treatment consists of surgical drainage of the abscess, either with or without tonsillectomy, and intravenous antibiotic therapy. Although the airway seems compromised, the peritonsillar abscess is usually in a fixed location in the lateral pharynx and does not interfere with ventilation of the patient by face mask after induction of general anesthesia. Visualization of the vocal cords should not be impaired because the pathologic process is supraglottic and well above the laryngeal inlet. Laryngoscopy must be carefully performed, avoiding manipulation of the larynx and surrounding structures. Intubation should be gentle because the tonsillar area is tense and friable and inadvertent rupture of the abscess can occur, leading to spillage of purulent material into the trachea.
FIGURE 47-3. Patient with a peritonsillar abscess on the left side. Note the displacement of the uvula. (Courtesy of Michael Cunningham, MD, Boston, MA.)
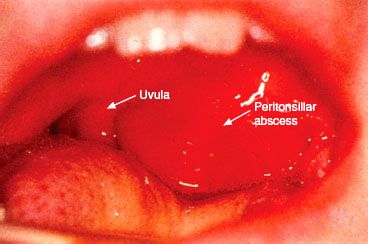
FIGURE 47-4. Neck radiograph of a patient with a peritonsillar abscess (arrow).
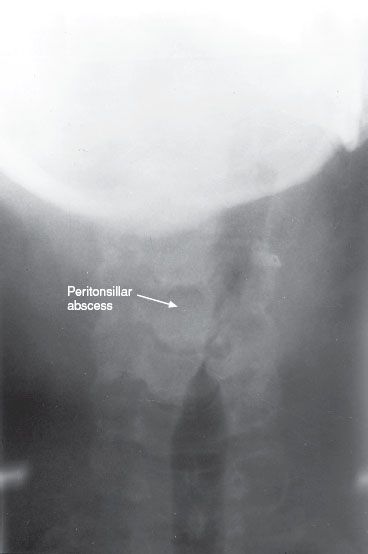
FIGURE 47-5. Computed tomography scan of a patient with a peritonsillar abscess (arrow).
 Acute postoperative pulmonary edema is an infrequent but potentially life-threatening complication encountered when airway obstruction is suddenly relieved. One proposed mechanism is that during inspiration before adenotonsillectomy, the negative intrapleural pressure that is generated causes an increase in venous return, enhancing pulmonary blood volume. In the healthy child without airway obstruction, pleural pressure ranges from −2.5 cm to −10 cm H2O during inspiration. Intrapleural pressure generated in the child with airway obstruction can be as much as −30 cm H2O, which causes disruption of the capillary walls of the pulmonary microvasculature when transmitted to the interstitial peribronchial and perivascular spaces. Concurrent with a negative transpulmonary gradient is an increase in venous return to the right side of the heart, thus increasing preload, which in the setting of “leaky capillaries” facilitates transudation of fluid into the alveolar space. To counterbalance this negative gradient, positive intrapleural and alveolar pressures are generated during exhalation, which decreases pulmonary venous return and blood volume. This phenomenon is similar to an expiratory “grunt” mechanism in which the transpleural pressures generated are similar to those present during a Valsalva maneuver.
Acute postoperative pulmonary edema is an infrequent but potentially life-threatening complication encountered when airway obstruction is suddenly relieved. One proposed mechanism is that during inspiration before adenotonsillectomy, the negative intrapleural pressure that is generated causes an increase in venous return, enhancing pulmonary blood volume. In the healthy child without airway obstruction, pleural pressure ranges from −2.5 cm to −10 cm H2O during inspiration. Intrapleural pressure generated in the child with airway obstruction can be as much as −30 cm H2O, which causes disruption of the capillary walls of the pulmonary microvasculature when transmitted to the interstitial peribronchial and perivascular spaces. Concurrent with a negative transpulmonary gradient is an increase in venous return to the right side of the heart, thus increasing preload, which in the setting of “leaky capillaries” facilitates transudation of fluid into the alveolar space. To counterbalance this negative gradient, positive intrapleural and alveolar pressures are generated during exhalation, which decreases pulmonary venous return and blood volume. This phenomenon is similar to an expiratory “grunt” mechanism in which the transpleural pressures generated are similar to those present during a Valsalva maneuver.
The rapid relief of airway obstruction results in decreased airway pressure, an increase in venous return, an increase in pulmonary hydrostatic pressure, hyperemia, and finally pulmonary edema. The all-important counterbalance of the expiratory grunt in limiting pulmonary venous return is lost when the obstruction is relieved. Contributing factors are the increased volume load on both ventricles as well as the inability of the pulmonary lymphatic system to remove acutely large amounts of fluid. The anesthesiologist may attempt to prevent this situation during induction of anesthesia by applying moderate amounts of continuous positive pressure to the airway, thus allowing time for circulatory adaptation to take place. This physiologic sequence is similar to that seen in patients with severe acute airway obstruction secondary to epiglottitis or laryngospasm.
Negative-pressure pulmonary edema is signaled by the appearance of frothy pink fluid in the endotracheal tube of an intubated patient or the presence of a decreased oxygen saturation, wheezing, dyspnea, and increased respiratory rate in the immediate postoperative period in a previously extubated patient. Mild cases may present with minimal symptoms. The differential diagnosis of negative-pressure pulmonary edema includes aspiration of gastric contents, adult respiratory distress syndrome, congestive heart failure, volume overload, and anaphylaxis. A chest radiograph illustrating diffuse, usually bilateral interstitial pulmonary infiltrates combined with an appropriate clinical history will confirm the diagnosis.7,34,35
Treatment is usually supportive, with maintenance of a patent airway, oxygen administration, and diuretic therapy in some cases. Endotracheal intubation and mechanical ventilation with positive end-expiratory pressure may be necessary in severe cases. Resolution is usually rapid and may occur within hours of inception. Most cases resolve within 24 hours without treatment. There is currently no reliable method for predicting which children will experience this clinical syndrome after their airway obstruction has been resolved.
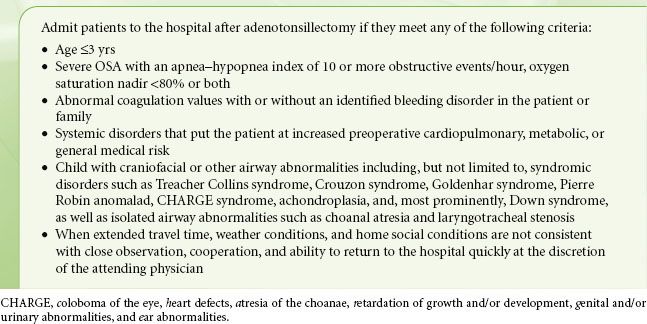
Adenoidectomy patients may be safely discharged on the same day after recovering from anesthesia. Although most tonsillectomy patients previously required postoperative admission to the hospital for observation, administration of analgesics, and hydration, many centers are discharging tonsillectomy patients on the day of surgery without adverse outcomes, and this trend will likely continue.35,36 Patients should be observed for early hemorrhage for a minimum of 4 to 6 hours and be free from significant nausea, vomiting, and pain prior to discharge. The ability to take fluid by mouth is not a requirement for discharge home. However, intravenous hydration must be adequate to prevent dehydration. Excessive somnolence and severe vomiting are indications for hospital admission. There are patients for whom early discharge is not advised, and those patients should be admitted to the hospital after tonsillectomy. The characteristics of such patients are listed in Table 47-1. Admission to an ICU is controversial and reserved for those children with very severe OSA, comorbidities that cannot be managed on the floor, and children who have demonstrated significant airway obstruction and desaturation in the initial postoperative period that required intervention beyond repositioning and oxygen supplementation.37
TABLE 47-1. TONSILLECTOMY AND ADENOIDECTOMY INPATIENT GUIDELINES: RECOMMENDATION OF THE AMERICAN ACADEMY OF OTOLARYNGOLOGY—HEAD AND NECK SURGERY
Ear Surgery
The ear and its associated structures are target organs for many pathologic conditions. General anesthesia for surgery of the ear has its own set of unique considerations that must be addressed.
Myringotomy and Tube Insertion
Chronic serous otitis in children can lead to hearing loss. Drainage of accumulated fluid in the middle ear is an effective treatment for this condition. Myringotomy, which creates an opening in the tympanic membrane for fluid drainage, may be performed alone. During healing, the drainage path may become occluded; therefore, ventilation tube placement is usually included. The insertion of a small plastic tube in the tympanic membrane serves as a vent for the ostium and allows for continued drainage of the middle ear until the tubes are naturally extruded in 6 months to 1 year, or surgically removed at an appropriate time (Fig. 47-6).
FIGURE 47-6. Two types of myringotomy tubes. Both the ventilating T-tube and the beveled-button ventilating tube are shown in full and cross-sectional views.

Myringotomy and tube insertion is a relatively short procedure, and anesthesia may be effectively accomplished with a potent inhalation agent, oxygen, and N2O administered by face mask. Premedication is not recommended because most sedative drugs used for premedication will far outlast the duration of the surgical procedure. Patients with chronic otitis frequently have accompanying recurrent URI. It is often the eradication of middle ear fluid that resolves the concomitant URI. Because tracheal intubation is not required for routine patients, the criteria for cancellation of surgery and anesthesia may be different for this procedure. Insertion of myringotomy tubes may be undertaken in most children with a concomitant URI provided that this can be completed with facemask anesthesia and endotracheal intubation is avoided. No significant difference in perioperative morbidity between asymptomatic patients and those fulfilling URI criteria has been demonstrated.38,39 It is recommended that patients with URI symptoms receive supplemental postoperative oxygen.
Middle Ear and Mastoid
Tympanoplasty and mastoidectomy are two of the most common procedures performed on the middle ear and accessory structures. To gain access to the surgical site, the head is positioned on a headrest, which may be lower than the operative table, and extreme degrees of lateral rotation may be required. Extreme tension on the heads of the sternocleidomastoid muscles must be avoided. The laxity of the ligaments of the cervical spine and the immaturity of odontoid process in children make them especially prone to C1 to C2 subluxation.
 Ear surgery
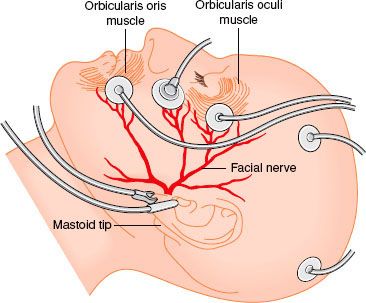
Ear surgery  often involves surgical identification and preservation of the facial nerve, which requires isolation of the nerve by the surgeon and verification of its function by means of electrical stimulation (Fig. 47-7). This is accomplished by brainstem auditory-evoked potential and electrocochleogram monitoring, which requires that complete muscle relaxation be avoided.40 If an opioid-relaxant technique is chosen, however, at least 30% of the muscle response, as determined by a twitch monitor, should be preserved. This fact suggests that it is not mandatory to avoid skeletal muscle relaxants in the anesthetic management of patients undergoing surgical procedures when monitoring of facial nerve function is necessary.
often involves surgical identification and preservation of the facial nerve, which requires isolation of the nerve by the surgeon and verification of its function by means of electrical stimulation (Fig. 47-7). This is accomplished by brainstem auditory-evoked potential and electrocochleogram monitoring, which requires that complete muscle relaxation be avoided.40 If an opioid-relaxant technique is chosen, however, at least 30% of the muscle response, as determined by a twitch monitor, should be preserved. This fact suggests that it is not mandatory to avoid skeletal muscle relaxants in the anesthetic management of patients undergoing surgical procedures when monitoring of facial nerve function is necessary.
FIGURE 47-7. Illustration of facial nerve and monitoring electrodes. (Courtesy of Steve Ronner, PhD, Boston, MA.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






