CHAPTER 27. Cold-Related Emergencies
Reneé Semonin Holleran
Competencies




1. Describe thermoregulation and mechanisms of heat loss.
2. Define mild, moderation, and severe hypothermia.
3. Identify methods to prevent heat loss during patient transport.
Hannibal started over the Pyrenean Alps in 218 bc with an army of 46,000, but in 15 days, he lost more than 20,000 men to the cold. 8 Statistics have not significantly improved since Hannibal’s time. US soldiers sustained 90,000 cold-related injuries in World War II, and Germany suffered 100,000. During two winter months in 1942, the Germans performed 15,000 cold-related amputations. 57 During the Korean War, the United States had a 10% cold-related casualty rate. 35,41,42
Transport personnel must be aware of the risk of hypothermia regardless of the climate or terrain in which they practice. A hiker on a summer day in the Rocky Mountains, an older person in an unheated home in the Sun Belt, and a sailor stranded off the warm Florida coast are all at equal risk of hypothermia. Studies have shown that cold contributes to 16% of all recreational boating fatalities and 20% of all scuba diving fatalities. 33,34,36,52
HYPOTHERMIA DEFINED
Hypothermia, defined as a core body temperature of less than 35 °C, occurs because the body can no longer generate sufficient heat to maintain body functions. 7Accidental hypothermia, in contrast to iatrogenic hypothermia, is the unintentional decrease in core temperature associated with trauma or exposure to the environment. 1,6,7,13,14,28 Core body temperature can be measured in the rectum, the esophagus, the tympanic membrane, or the bloodstream. Rectal thermometers provide the least reliable measurement of core body temperature. The esophageal and tympanic thermometers are more reliable. Table 27-1 lists thermometric equivalents for Fahrenheit and Celsius temperatures. 20
| Degrees Celsius | Degrees Fahrenheit |
|---|---|
| 15.0 | 59.0 |
| 16.0 | 60.8 |
| 17.0 | 62.6 |
| 18.0 | 64.4 |
| 19.0 | 66.2 |
| 20.0 | 68.0 |
| 21.0 | 69.8 |
| 22.0 | 71.6 |
| 23.0 | 73.4 |
| 24.0 | 75.2 |
| 25.0 | 77.0 |
| 26.0 | 78.8 |
| 27.0 | 80.6 |
| 28.0 | 82.4 |
| 29.0 | 84.2 |
| 30.0 | 86.0 |
| 31.0 | 87.8 |
| 32.0 | 89.6 |
| 33.0 | 91.4 |
| 34.0 | 93.2 |
| 35.0 | 95.0 |
| 36.0 | 96.8 |
| 37.0 | 98.6 |
| 38.0 | 100.4 |
| 39.0 | 102.2 |
| 40.0 | 104.0 |
Classification
Hypothermia can be both a clinical symptom and a disease. 8 It can be classified as primary, with simple environmental exposure in a healthy person, or secondary, with hypothermia as a part of a disease process or caused by a predisposing condition. 8 Multiple predisposing factors can place a person at risk of hypothermia. Age, diseases, medications, and type and length of exposure can all contribute to the development of hypothermia. The transport environment can especially place a patient at risk for hypothermia from loss of clothing, wet clothing, lack of protection from the environment, medications, diseases and injuries, and lack of environmental control within the transport vehicle itself. 14,22.23.24. and 25.Box 27-1 contains a summary of predisposing factors to hypothermia.
BOX 27-1
Predisposing Factors for Hypothermia
Diabetes
Malnutrition
Hemorrhagic shock
Stroke
Thermal injuries
Elderly
Infants
Emergency childbirth
Environmental exposure
Immersion in cold water
Fluid resuscitation with cold infusions
Aircraft frame
Failure to remove wet clothing
Lack of environmental control in the transport vehicle
Modified from Danzl D: Accidental hypothermia. In Auerbach P, editor: Wilderness medicine, ed 5, St Louis, 2007, Mosby.
Hypothermia is classified into four stages. Mild hypothermia is defined as a core body temperature greater than 32 °C and less than 35 °C (90 °F to 95 °F) and is associated with low morbidity and mortality rates. The patient may display symptoms of ataxia, slurred speech, apathy, and even amnesia. Thermoregulatory mechanisms continue to operate. 16Moderate hypothermia occurs when the core body temperature is greater than 28 °C but less than 32 °C (82 °F to 90 °F). Thermoregulatory actions such as shivering continue but begin to decrease and eventually fail. The patient’s level of consciousness continues to decrease, and cardiac arrhythmia may develop. Severe hypothermia is defined as a core body temperature of 28 °C (82 °F) or less and is associated with a higher morbidity and mortality rates. 2,6,26,27Profound hypothermia occurs at a temperature of 20.0 °C to 9.0 °C (68.0 °F to 48.2 °F). These zones and characteristics are summarized in Table 27-2. 7
| Degrees Celsius | Degrees Fahrenheit | Characteristics |
|---|---|---|
| 38.0 | 99.6 | Normal rectal temperature |
| 37.0 | 98.6 | Normal oral temperature |
| Mild | ||
| 36.0 | 96.8 | Increased basal metabolic rate in an attempt to balance heat loss, tachycardia, increased cardiac output |
| 35.0 | 95.0 | Shivering at the maximum, usually still responsive, but level of consciousness beginning to decrease, regulatory systems beginning to falter |
| 34.0 | 93.2 | Dysarthria, amnesia, blood pressure still normal, oxyhemoglobin curve begins to shift to the left |
| 32.0 | 91.4 | Heart rate decreases to 50 to 60 bpm, ataxia, poor coordination, apathy, lethargy |
| Moderate | ||
| 32.0 | 89.6 | Vasoconstriction, level of consciousness progressively falls |
| 31.0 | 87.8 | Shivering stops, respirations and blood pressure may be difficult to obtain |
| 30.0 | 86.0 | Mental confusion, delirium, increased muscle rigidity; heart rate and cardiac output begin to decrease, arrhythmias begin to develop (atrial fibrillation) |
| 29.0 | 84.2 | Acidosis, hyperglycemia, metabolic rate decreased by 50%, decreased respirations, bradycardia, decreased stroke volume, decreased cardiac output, pupils dilated, paradoxical undressing |
| Severe | ||
| 28.0 | 82.4 | Hypotension, loss of vasoconstrictive capabilities, ventricular fibrillation if patient handled roughly, increased myocardial irritability |
| 27.0 | 80.6 | Prolonged PR, QRS, and QT intervals; muscle flaccidity; no voluntary movement (appears dead); no pupillary reactions |
| 26.0 | 78.8 | Seldom conscious, areflexia |
| 25.0 | 77.0 | Stuporous, hypoventilation, ventricular fibrillation may appear spontaneously, cerebral blood flow one third of normal, cardiac output 45% of normal |
| 24.0 | 75.2 | Coma, pulmonary edema, respiratory arrest |
| 23.0 | 73.4 | No spontaneous movement, rigor mortis appearance, no corneal reflexes |
| 22.0 | 71.6 | Maximal risk of ventricular fibrillation, 75% decrease in oxygen consumption |
| 21.0 | 69.8 | Apnea |
| Profound | ||
| 20.0 | 68.0 | Pulse is 20% of normal |
| 18.0 | 64.4 | Asystole |
| 10.0 | 50.0 | 92% decrease in oxygen consumption |
Mortality
Many factors influence the mortality from hypothermia, including degree and duration of hypothermia, age, poverty, predisposing disease, and complications. Hypothermia in a trauma patient can be deadly. 1,2 Most victims die of cardiac arrhythmia. The presence of a severe underlying disease is almost always associated with increased mortality. Rankin and Rae47 noted no correlation between the severity of hypothermia or the rate of rewarming and the clinical outcome but did note, rather, that mortality was correlated with the presence or absence of severe underlying disease.
The old adage “the patient is not dead until they are warm and dead” still directs the medical management of the patient with hypothermia. Transport programs, particularly those that provide service in cold weather or rescue environments, must have policies and procedures that control when and how a patient with severe hypothermia is resuscitated and transported.
NORMAL TEMPERATURE REGULATION
Humans become uncomfortable with even a small deviation in core body temperature from 37.6 °C. In De Re Medicina, Aurelius Cornelius Celsus described in 25 ad the universal discomfort of cold temperatures as “hurtful to an old or slender man, to a wound, to the precordia, intestines, bladder, ears, hips, shoulders, private parts, teeth, bones, nerves, womb and brain. It also renders the surface of the skin pale, dry, hard and black. From this proceed shudderings and tremors.”7,25 Normal body temperature is maintained in a narrow range by a delicate balance of heat loss and heat production regulated by a “thermostat” in the preoptic anterior hypothalamus. The hypothalamus is sensitive to temperature changes as small as 0.5 °C. 4 Stimuli sent from the hypothalamus to the sympathetic nervous system increase heart rate and dilate muscle blood vessels to increase heat production. In addition, shivering generates heat by increasing muscle activity. At the same time, cutaneous vasoconstriction reduces heat loss by shunting blood from the periphery to the core. 50.51.52.53.54.55. and 56.58,61,65
The ability to shiver is affected by hypoglycemia, hypoxia, fatigue, alcohol, and drugs. Shivering is the body’s main mechanism of heat production and its strongest defense against hypothermia. However, shivering requires increased blood flow to peripheral muscles and consequently results in a 25% heat loss. Preshivering increases heat production by 50% to 100%. Visible shivering increases heat production by 500%. An average 70-kg person produces about 100 kcal/h of heat under basal conditions and up to 500 kcal/h when shivering. 7 This degree of heat production, however, cannot be sustained for long because the patient becomes fatigued once glycogen stores are depleted. Maximal shivering occurs at 35 °C and stops below 32 °C. Cessation of shivering is a sign that the patient has made the transition from mild to severe hypothermia.
Hypothermia results when the thermoregulation system becomes overwhelmed or damaged centrally at the hypothalamic level or systemically by a decrease in heat production or an increase in heat loss. Thermoregulation is disrupted at the hypothalamic level by head trauma, cerebral neoplasm, cerebrovascular accident, acute poisoning, acid-base imbalance, Parkinson’s disease, and Wernicke’s encephalopathy. Acute spinal injury can eliminate vasoconstrictive control by the hypothalamus. Heat production is decreased by malnutrition, hypothyroidism, hypopituitarism, and rheumatoid arthritis. Normally, 90% of the heat produced by the body is lost to the environment by way of conduction, convection, radiation, and evaporation.
Methods of Heat Loss7
Conduction together with convection each account for 15% of heat loss. 16Conduction occurs when the body comes into direct contact with a heat conductor. Examples of good conductors are water, snow, metal, and damp ground. Normally, conduction plays a minor role in heat loss, but it is an important factor when the patient has been immersed in cold water, is lying in a snow bank, or is wandering without shoes for an extended period. Heat loss in water is approximately 24 times faster than heat loss in air of the same temperature. 17,19 Immersion in water in temperatures less than 10 °C causes hypothermia in only a few minutes, 7 in contrast to more than an hour in air. 58
Heat loss by convection occurs when either air or water moves over the patient or the patient moves through air or water. Heat loss is accelerated by increasing air movement (forced convection). The wind, the rotating blades of the helicopter, and the movement required to transport the patient to the transport vehicle all contribute to forced convective heat loss. Figure 27-1 lists temperature differences related to wind chill factors.
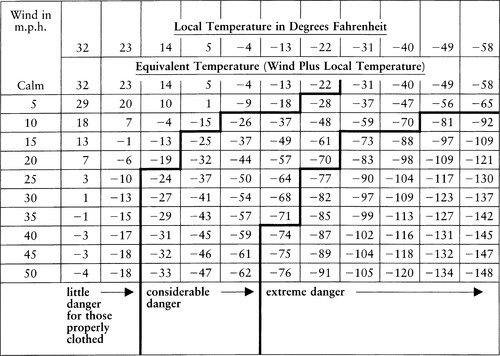 |
| FIGURE 27-1 Chill factor: temperature plus wind. (From Vaughn PB: Local cold injury-menance to military operations: a review Milit Med 5:307, 1980.) |
Body heat lost by radiation is 45%. 7,9Radiant heat transfer occurs when a difference exists between body temperature and ambient temperature. The body absorbs heat when the ambient temperature is higher and emits heat when the ambient temperature is lower. Radiant heat loss, as convection, is directly related to dermal blood flow and percentage of skin surface exposed. Radiant heat loss is accelerated at night or when the sky is overcast.
Evaporation occurs when water on the body surface is converted from a liquid state to a gaseous state. 7,9 The body is cooled as the vapor moves off the body into the air. The evaporative process accounts for about 25% of heat loss7,9 and occurs normally through the skin, lungs, and upper airway. Burns and various skin lesions expose more open moist surface area and thereby increase evaporative losses. In addition, evaporation increases when the patient is wearing damp clothing or is covered with blood.
Heat loss is inversely proportional to body size and body fat. White fat insulates because it has less blood flow and consequently has less ability to vasodilate and lose heat. Consequently, large people conserve heat better than small people, obese people better than thin people, and adults better than children.
As newborns, about 5% of our body weight is made up of heat-producing brown fat cells, but as we age, the proportion of brown fat cells drops dramatically, giving way to more white fat cells. Brown fat cells are relatively abundant in races that are highly cold-adapted, such as the Inuit, and in most mammals, including humans as neonates. 50
Brown (heat-producing) fat is typically located between the shoulder blades and wrapped around the internal organs close to the heart. People who live outdoors, such as the homeless or Inuit, have a lot more of this fat, and those people burn a lot of fat to keep warm. Urban humans who are usually reared in warm tightly temperature-controlled environments tend to have reduced populations of brown fat and hence reduced capacity for nonshivering thermogenesis, which has high survival value in cold environments. Long-term cold adaptation increases the amount of brown adipose tissue. 50
Lipolysis with oxidation of fatty acids requires oxygen and can produce quite large amounts of heat. Brown fat cells are especially adapted to thermogenesis; it appears that they produce heat with little production of ATP. Norepinephrine release triggers lipolysis, oxidation of fatty acids, and heat production in both white and brown fat deposits. Nonshivering thermogenesis typically uses mitochondria in brown fat and is stimulated by the sympathetic nervous system, releasing norepinephrine. Mammals that acclimatize to cold temperatures build up brown fat stores mediated by the thyroid hormones. 50
The transport team must carefully consider risk factors that may place the patient at risk for development of hypothermia. These risk factors include2,4,16,22:
Age: The pediatric patient has less fat, and shivering provides limited heat production. Elderly people may also have similar inabilities to generate heat.
Medications: Antidepressants, phenothiazines, narcotics, neuromuscular blocking agents, and nonsteroidal antiinflammatory drugs (NSAIDs) are only a few examples of the pharmacologic agents that may interfere with the patient’s ability to maintain body heat.
Preexisting medical problems: Conditions such as Parkinson’s disease, head injury, malnutrition, hypoglycemia, and shock place the patient at risk of hypothermia.
Prolonged exposure and weather conditions: Factors such as high humidity, brisk winds, and rain or snow may increase heat loss.
PHYSIOLOGIC RESPONSE TO HYPOTHERMIA7,13,43,44,48,59,60,62,64
Metabolic Derangements
Complications of hypothermia result mainly from the sequelae of metabolic derangements. Initially, metabolism increases to generate heat. Optimal metabolism begins to decrease at 35 °C. Symptoms of mild hypothermia consequently include shivering, hypoglycemia, and increased respiratory rate, heart rate, and cardiac output. A dramatic decrease in metabolic rate occurs between 30 °C and 33 °C as the patient makes the transition from moderate to severe hypothermia. Every 10 °C decrease in temperature decreases metabolism by half. 7 At 28 °C, all thermoregulation ceases. The metabolic functions of the liver also begin to falter at temperatures below 33 °C. The liver no longer efficiently metabolizes fats, proteins, and carbohydrates or drugs, alcohol, and lactic acid. Symptoms of severe hypothermia include absence of shivering, hyperglycemia, and decreased respiratory rate, heart rate, and cardiac output. Bowel sounds are decreased, if not absent, as a result of decreased gastric motility and gastric dilation. 27.28. and 29.
Hypoglycemia is associated with chronic mild hypothermia, whereas hyperglycemia is associated with acute severe hypothermia. Long-term shivering depletes glucose and glucose stored in the form of glycogen. Shivering can stop at temperatures greater than 33 °C if glucose or glycogen stores are depleted or if insulin is no longer available. Shivering begins again when the core body temperature increases to 32 °C if depleted glucose is replaced. Hyperglycemia occurs at temperatures below 30 °C because insulin no longer promotes glucose transport into cells once metabolism significantly decreases. 9,23 Hyperglycemia does not occur if glucose and glycogen stores have been previously depleted but not replaced.
Oxygenation and Acid-Base Disorders
Respiratory rate initially increases after sudden exposure to cold but then decreases as body temperature and metabolism decrease. 8 At temperatures above 32 °C, ventilation is usually adequate. At 30 °C, respirations are shallow and difficult to observe. Apnea and respiratory arrest commonly occur at temperatures between 21 °C and 24 °C. Although carbon dioxide production also decreases to about half the basal level with each 8 °C drop in temperature, 25 the decreased respiratory rate is inadequate to effectively excrete CO 2 at a temperature below 33 °C. Consequently, a respiratory acidosis develops in the hypothermia victim.
Cellular respiration is impaired by the decrease in metabolism, drop in cardiac output, and left shift on the oxyhemoglobin dissociation curve. Hypothermia decreases cardiac output by decreasing heart rate and circulating blood volume and by increasing blood viscosity and peripheral vascular resistance. Blood shifting to the core results in a perceived overhydration, and the body responds by removing the extra volume through diuresis. Prolonged hypothermia also causes plasma to leak from the capillaries, thereby increasing blood viscosity by 2% for every 1 °C decline. 8,25
Hypothermia begins to shift the oxyhemoglobin dissociation curve to the left at 34 °C. Oxygen then binds tenaciously with hemoglobin, which results in reduced tissue oxygen delivery. In addition, Biddle has noted that oxygen consumption was half of normal at 27 °C and, at 17 °C, had fallen to one quarter the normal value. 8,10 Anaerobic metabolism and lactic acid production increase from the combination of decreased cardiac output, oxygen delivery, and oxygen consumption. The increase in lactic acid leads to cardiac arrhythmia and death.
The cardiovascular system is more sensitive to the effects of acid-base disturbances than any other body system. Acidosis is commonly associated with asystole, and alkalosis is associated with ventricular fibrillation. 8,9,39,41 Hypoventilation and lactic acid production lead to respiratory and metabolic acidosis. Acidosis usually corrects itself once the patient is rewarmed. Hyperkalemia is associated with metabolic acidosis and with muscle damage and kidney failure, which may all be present in the rewarmed hypothermic patient. Iatrogenic respiratory and metabolic alkalosis is difficult to treat and should be avoided.
Central Nervous System
The central nervous system (CNS) displays some of the most impressive sequelae in the patient with hypothermia. Complete recovery is possible even after prolonged cardiac arrest. Hypothermia protects CNS integrity and may allow the brain to withstand long periods of anoxia. 15 Cerebral blood flow decreases 6% to 7% for every 1 °C decline until 25 °C is reached. 8,9 Cerebral oxygen requirements decrease to 50% of normal at 28 °C, to 25% of normal at 22 °C, 13,41 and to 12.5% of normal at 16 °C. 52 Caroline5 noted that the brain can survive without perfusion for about 10 minutes at 30 °C, whereas it can survive for up to 25 to 30 minutes at 20 °C. 52 Remarkably, Steinman54 noted that at 16 °C the brain can survive without oxygen for up to 32 to 48 minutes. 54,55
Patients with mild hypothermia are clumsy, apathetic, withdrawn, and irritable. Reflexes are hyperactive at temperatures above 32 °C. Level of consciousness begins to decrease markedly at 32 °C, and patients become lethargic or disoriented and begin to hallucinate. Hypothermia victims even remove jackets, gloves, shoes, and other protective clothing. This reaction is known as paradoxical undressing and is often one of the first signs that patients are becoming severely hypothermic. Patients can no longer ascertain whether they are cold.
The cough reflex is absent at decreased temperatures, and aspiration of stomach contents can occur. Coma develops between 28 °C and 30 °C. At temperatures below 30 °C, the pupils dilate and become nonreactive. In addition, corneal and deep-tendon reflexes may be absent. The patient with hypothermia must be carefully examined to rule out rigor mortis or death. At temperatures below 20 °C, the electroencephalographic results, if they were available, would be flat. 54,55
Cardiac Arrhythmia
The effects of hypothermia on heart rhythm were noted as early as 1912. Hyperthermia was found to produce bradycardia that progressed to asystole. 8.9. and 10. In 1923, subjects reportedly showed T-wave changes on electrocardiograms (ECGs) after drinking 600 mL of ice water. 45,46 Up to 90% of all patients with hypothermia are believed to have some electrocardiographic abnormality, including atrial fibrillation, sinus bradycardia, and junctional rhythms. 16,33.34.35. and 36.58,63
The heart initially responds to mild hypothermia with an increase in heart rate as a result of sympathetic stimulation; this response is short lived. Heart rate then decreases to 50 to 60 bpm at 33 °C and to 20 bpm at lower temperatures. 7,16 Atrial fibrillation with a slow ventricular rate is common at temperatures below 29 °C. Okada, Nishimura, and Yoshiro40 recently noted that atrial fibrillation was unusual in mild hypothermia (temperature greater than 32 °C) and was often observed in moderate (32 °C to 26 °C) and moderately deep (less than 26 °C) hypothermia. About half of the cases studied in moderately deep hypothermia remained in sinus, atrial, or junctional rhythm. Okada and colleagues39,40 also noted that atrial fibrillation usually converted to sinus rhythm spontaneously after return to normothermia.
Changes in the conduction system begin at 27 °C and may be observed as a widened QRS interval and prolonged PR and QT intervals. The Osborne, or J, wave is seen clearly at 25 °C. The J wave is described as an extra deflection at the junction of the QRS and ST segments (Figure 27-2). The origin of the J wave is unknown. According to Okada, Nishimura, and Yoshiro, 40 the prolongation of the Q-T interval and the presence of J waves are directly related to the severity of the hypothermia. Large J waves (see Figure 27-2) are seen at temperatures of less than 30 °C, whereas small J waves are seen at higher temperatures.
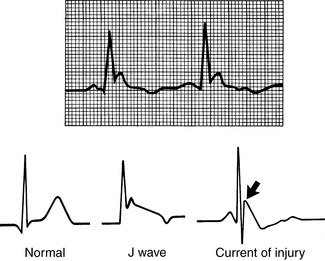 |
| FIGURE 27-2 ECG tracing showing the characteristic J, or Osborne, wave of hypothermia. |
Several theories have been offered for the presence of J waves in hypothermia. The J wave may represent hypothermia-induced ion fluxes that cause delayed depolarization or early repolarization of the left ventricle. The J wave may also be a hypothalamic or neurogenic factor. J waves may also be seen in patients with central nervous system lesions or cardiac ischemia, in patients who are septic, or even in young healthy people. 21
Ventricular irritability, which occurs at temperatures less than 30 °C, is commonly associated with alkalosis and is the most lethal cardiovascular response to hypothermia. At 28 °C, rough handling, careless intubation, or cardiac compressions can irritate the heart. Ventricular fibrillation can occur spontaneously at 25 °C. Unfortunately, arrhythmia at temperatures below 30 °C becomes increasingly refractory to drugs and defibrillation because of decreased perfusion and metabolic rate.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






