Equipment for Peripheral Nerve Blocks
Ali Nima Shariat, Patrick M. Horan and Kimberly Gratenstein and Colleen McCally and Ashton P. Frulla
Introduction
Over the past several decades, regional anesthesia equipment has undergone substantial technological advances. Historically, the development and consequent introduction of the portable nerve stimulator to clinical practice in the 1970s and 1980s was a critical advance in regional anesthesia, allowing the practitioner to better localize the targeted nerve. In recent years, however, the advent of ultrasound, better needles, catheter systems, and monitoring has entirely rejuvenated, if not revolutionized, the practice of regional anesthesia.
Induction and Block Room
Regional anesthesia is ideally performed in a designated area with access to all the appropriate equipment necessary to perform blocks. Whether this area is the operating room or a separate block room, there must be adequate space, proper lighting, and equipment to ensure successful, efficient, and safe performance of peripheral nerve blocks (PNBs). Provision for proper monitoring, oxygen, equipment for emergency airway management and positive-pressure ventilation, and access to emergency drugs is of paramount importance (Figure 3-1).

FIGURE 3-1. Typical block room setup. Shown are monitoring, oxygen source, suction apparatus, ultrasound machine, and nerve block cart with equipment.
Cardiovascular and Respiratory Monitoring During Application of Regional Anesthesia
Patients receiving regional anesthesia should be monitored with the same degree of vigilance as patients receiving general anesthesia. Local anesthetic toxicity due to intravascular injection or rapid absorption into systemic circulation is a relatively uncommon but potentially life-threatening complication of regional anesthesia. Likewise, premedication, often necessary before many regional anesthesia procedures, may result in respiratory depression, hypoventilation, and hypoxia. For these reasons, patients receiving PNBs should have vascular access and be appropriately monitored. Routine cardio-respiratory monitoring should consist of pulse oximetry, noninvasive blood pressure, and electrocardiogram. Respiratory rate and mental status should also be monitored. The risk of the local anesthetic toxicity has a biphasic pattern and should be anticipated (1) during and immediately after the injection and (2) 10 to 30 minutes after the injection. Signs and symptoms of toxicity occurring during or shortly after the completion of the injection are due to an intravascular injection or channeling of local anesthetics to the systemic circulation (1–2 minutes). In the absence of an intravascular injection, the typical absorption rate of local anesthetics after injection peaks at approximately 10 to 30 minutes after performance of a PNB1; therefore patients should be continuously and closely monitored for at least 30 minutes for signs of local anesthetic toxicity.
Regional Anesthesia Equipment Storage Cart
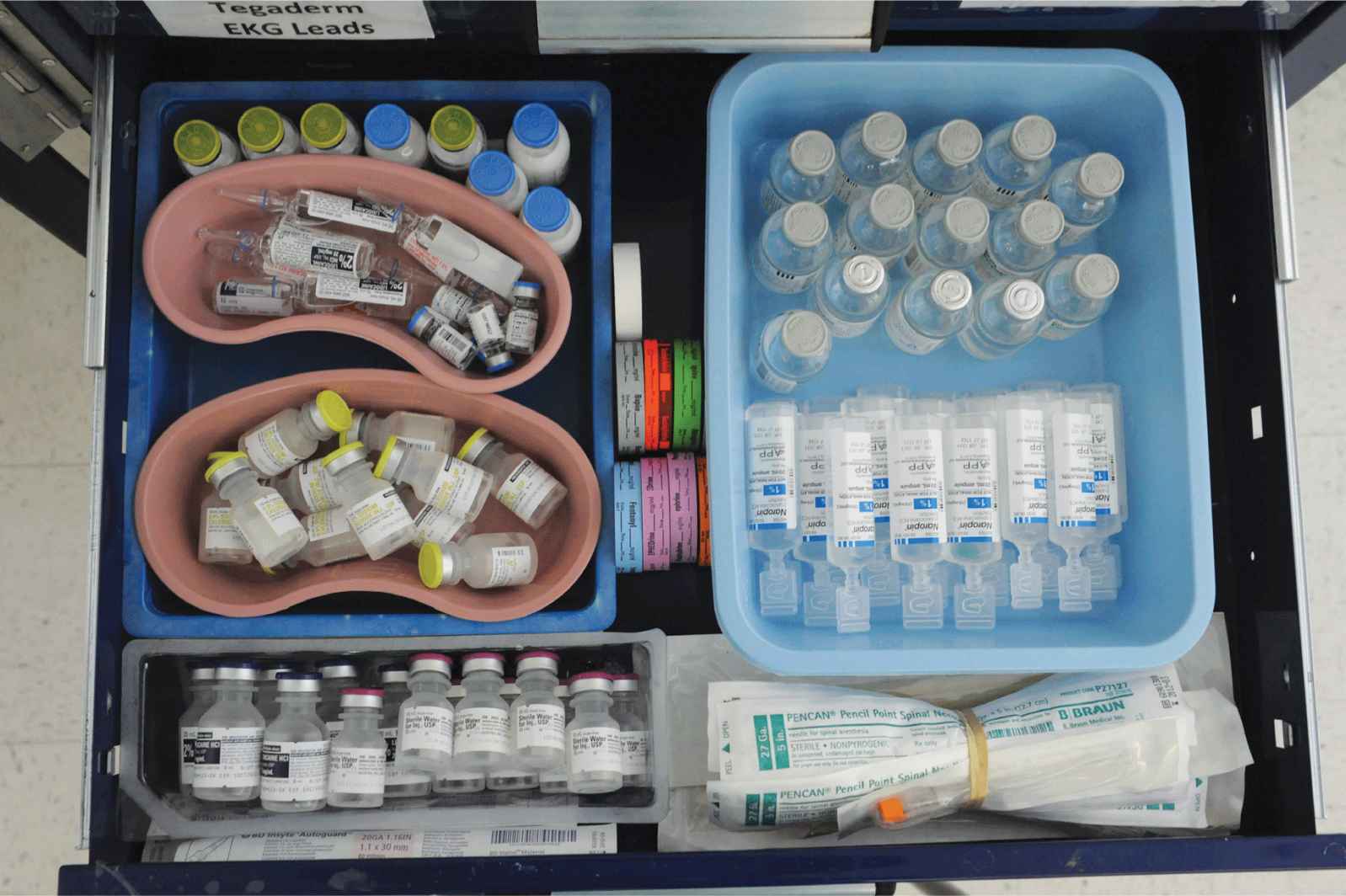
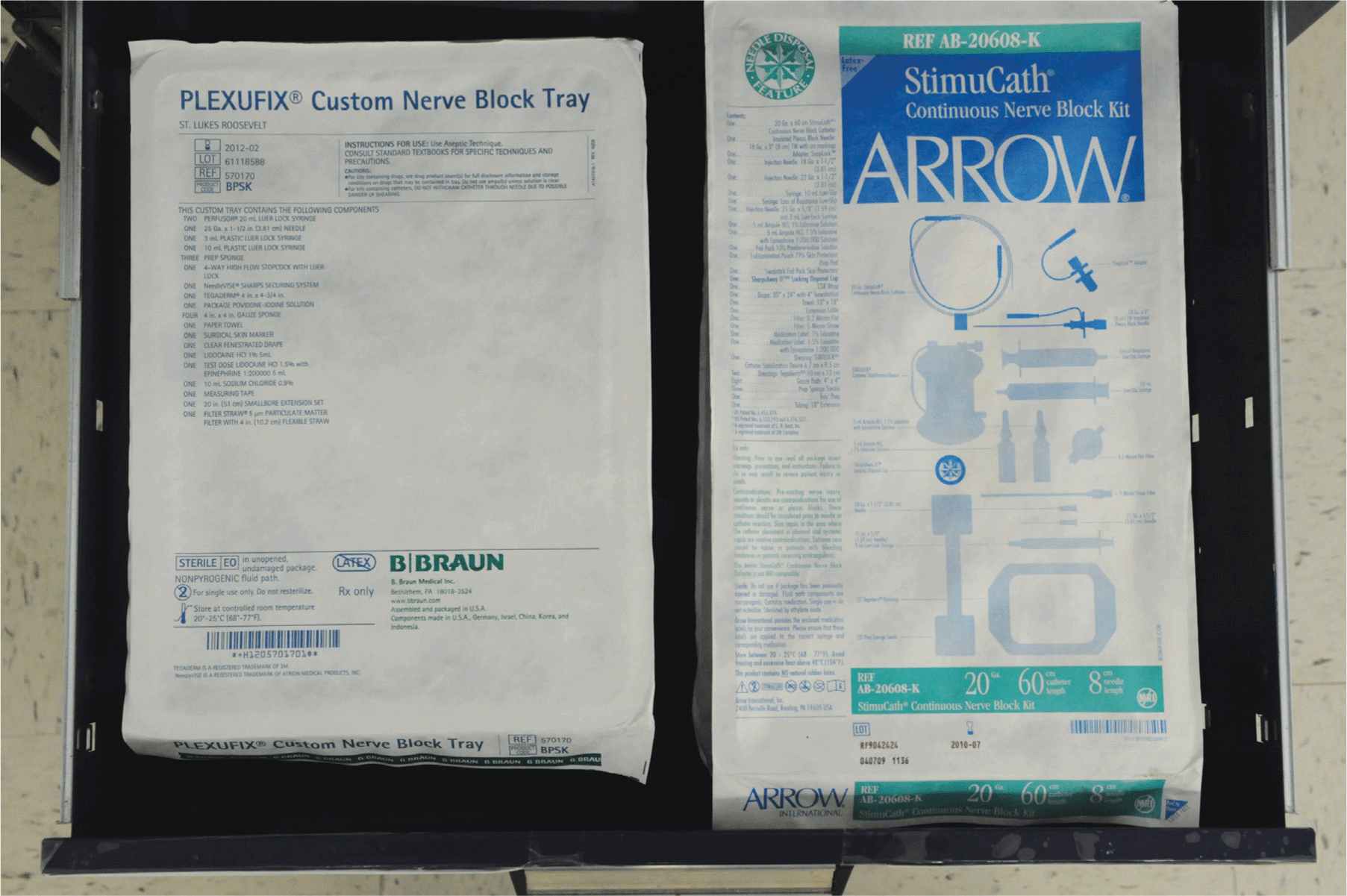
A regional anesthesia cart should have all drawers clearly labeled and be portable to enable transport to the patient’s bedside. The anesthesia cart should also be well stocked with all equipment necessary to perform PNBs effectively, safely, and efficiently. Supplies such as needles and catheters of various sizes, local anesthetics, and emergency airway and resuscitation equipment should also be included (Figures 3-2,3-3, and 3-4).
FIGURE 3-2. Typical nerve block cart with labels for each drawer.

FIGURE 3-3. Drawer 1, including electrocardiogram leads, 18-gauge needles, skin adhesive and catheter securing systems, alcohol swabs, clear, occlusive dressing, tape, iodine swabs, and lubricating gel.
FIGURE 3-4. Drawer 2, including propofol, lidocaine 2%, sterile saline, and atropine, sterile saline, lidocaine 2% and sterile water, syringe labels, bupivacaine 0.5%, ropivacaine 1%, and spinal needles.
Different drawers are best organized in a logical manner to ensure quick and easy access. One drawer should be designated for emergency equipment and should include laryngoscopes with an assortment of commonly used blades, styletted endotracheal tubes and airways of various sizes (Figure 3-5). Emergency drugs that should be present include atropine, ephedrine, phenylephrine, propofol, succinylcholine, and intralipid 20%. The latter can alternatively be stored in a nearby drug cart or drug-dispensing system that is immediately available and in close proximity to the block room. This way, it can be prepared within minutes in case of emergency (Figures 3-6, 3-7, and 3-8).
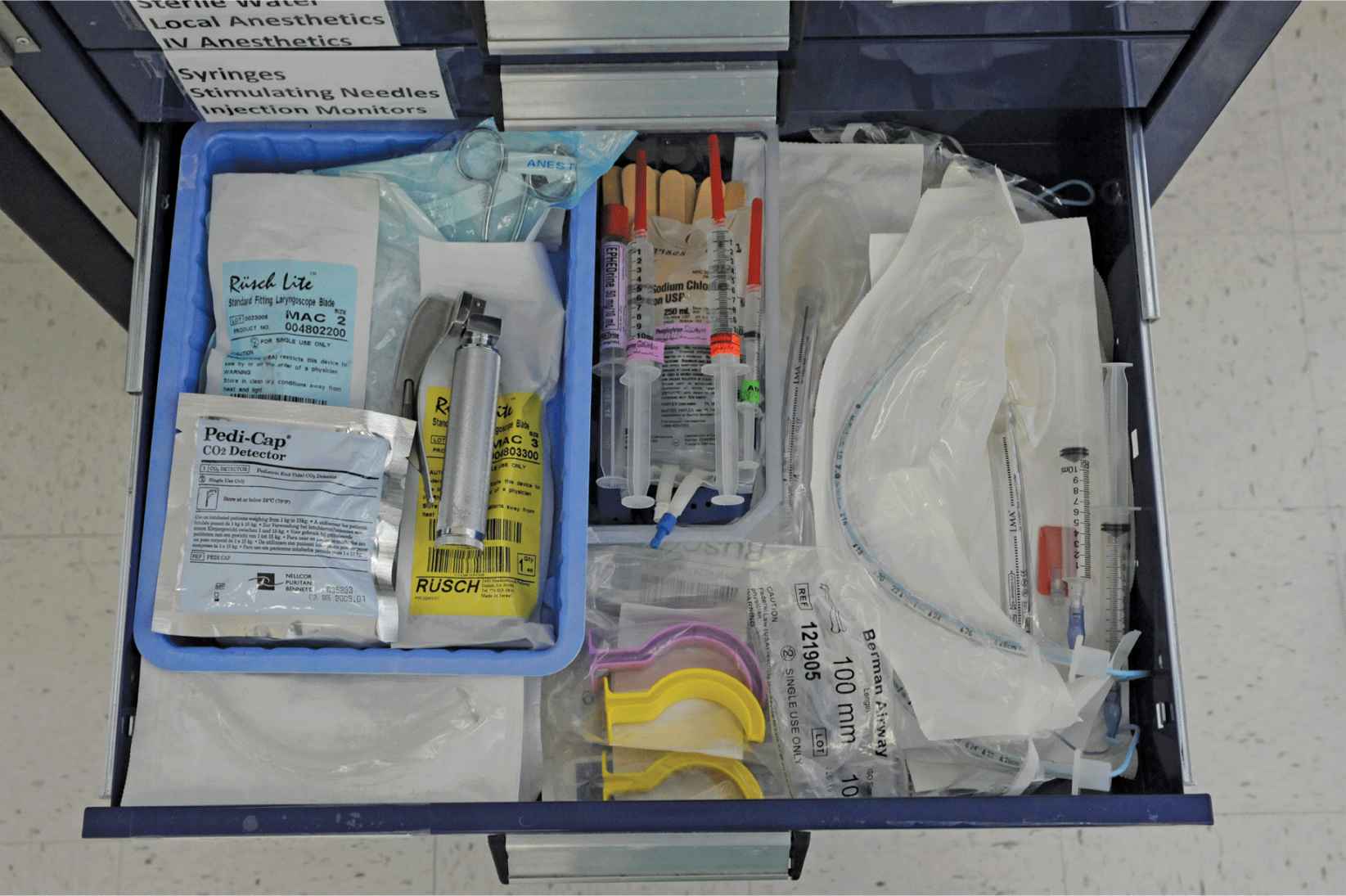
FIGURE 3-5. Drawer 3, including laryngoscope, assorted blades, and Magill forceps, emergency medications, stylleted endotracheal tubes, and laryngeal mask airways of assorted sizes, nasal airways, and oral airways.
FIGURE 3-6. Drawer 4, including syringes of assorted sizes, pressure monitors, stimulating needles, and nonstimulating catheters.
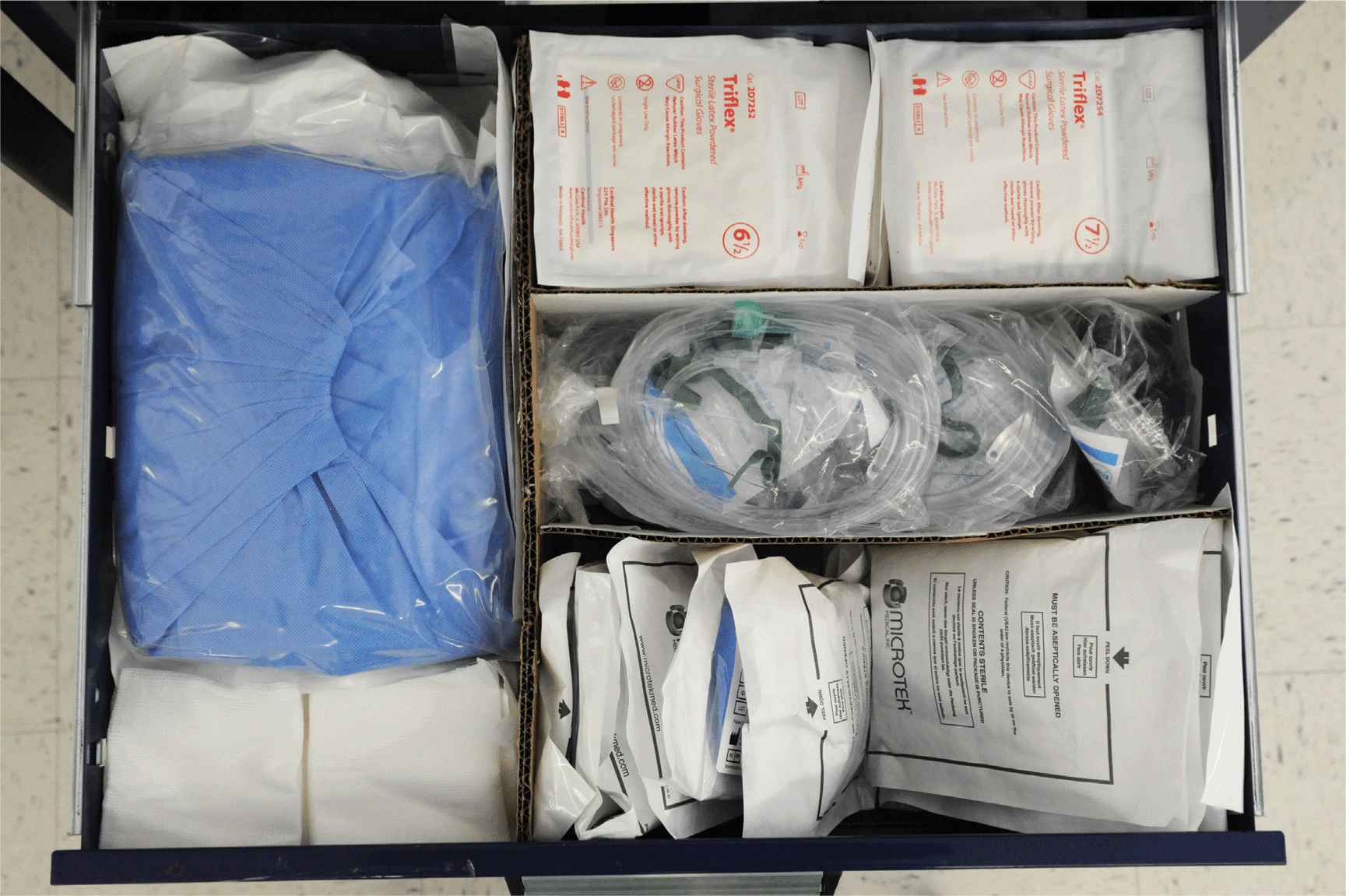
FIGURE 3-7. Drawer 5, including sterile drape, sponges, sterile gloves, oxygen masks, and sterile transducer coverings.
FIGURE 3-8. Drawer 6, including custom nerve block tray and continuous nerve block kit with stimulating catheters.
Suggested Emergency Drugs Required During Nerve Block Procedures
See Table 3-1.
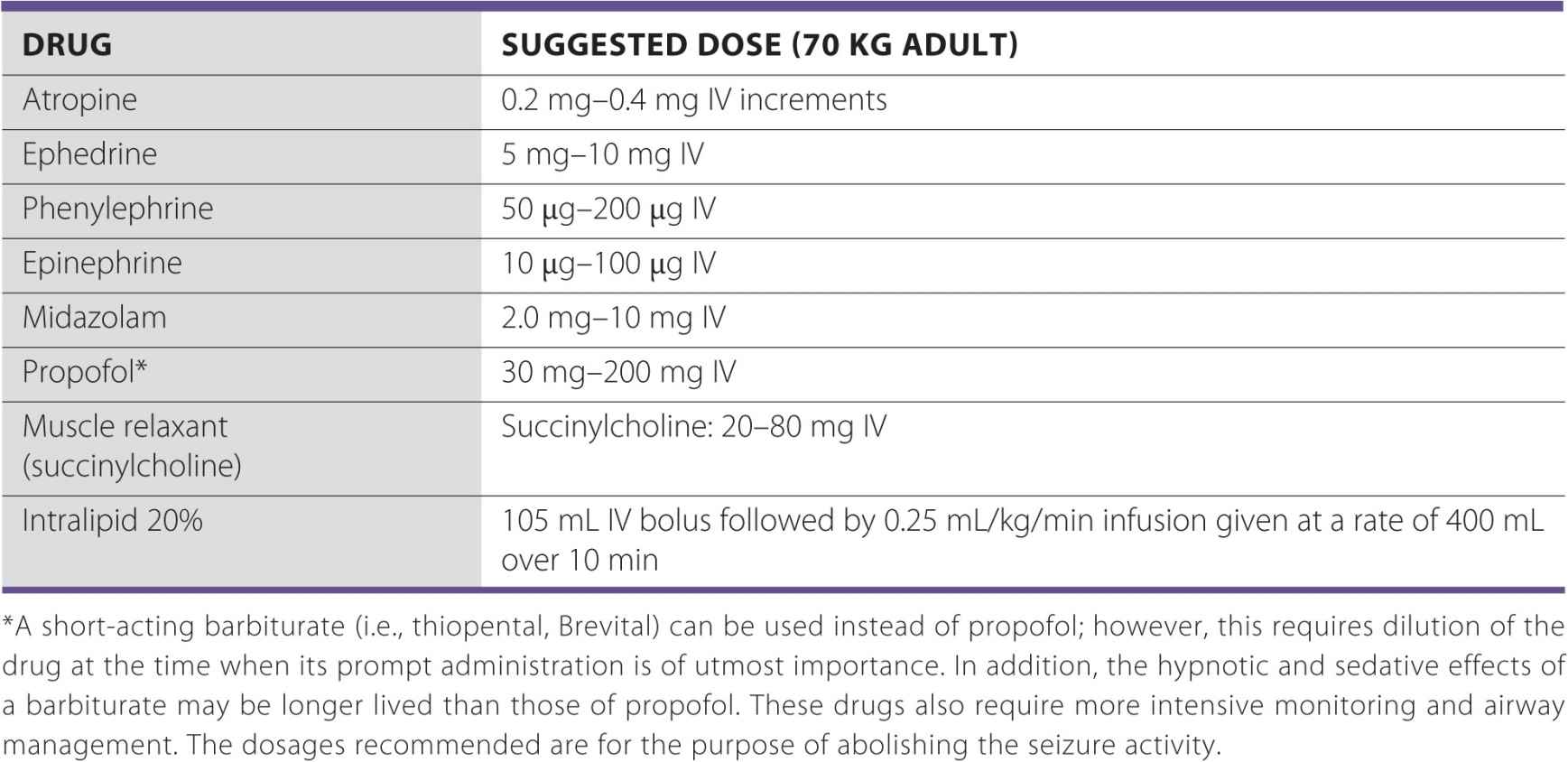
TABLE 3-1 Suggested Emergency Drugs Required During Nerve Block Procedures
Treatment of Severe Local Anesthetic Toxicity
A 1998 study heralded the clinical utility of intralipid therapy in the treatment of local anesthetic toxicity. Administration of 20% intralipid solution to rats increased the lethal dose of bupivacaine by 48% when compared with untreated controls. The same study also showed increasing survival rates when used as part of a resuscitation protocol. The results were explained by the portioning of bupivacaine into the newly created lipid phase.2 In follow-up studies, dogs that had bupivacaine-induced cardiovascular collapse were successfully resuscitated after receiving lipid infusion, demonstrating the utility of intralipid in a large animal model that more closely approximates human physiology.3 In 2006, Rosenblatt et al published the first use of intralipids in a patient to reverse bupivacaine-induced cardiotoxicity.4 Soon thereafter, additional case reports of successful resuscitation from local anesthetic-induced toxicity with intralipid were published5–8 establishing intralipid infusion as an important emergency intervention in the practice of regional anesthesiology. Based on laboratory evidence and a growing body of anecdotal reports in clinical practice, it appears prudent to keep intralipid solution 20% in close proximity to locations where regional anesthesia is administered.9
Peripheral Nerve Block Trays
Commercially available, specialized nerve block trays are useful for time-efficient practice of PNBs. An all-purpose tray that can be adapted to a variety of blocks may be the most practical, given the wide array of needles and catheters that may be needed for specific procedures. Appropriate needles, catheters, and other specialized equipment are simply opened and added to the generic nerve block tray as needed (Figure 3-9).

FIGURE 3-9. An example of a custom nerve block tray, including lidocaine 1%, lidocaine 1% with epinephrine, sterile saline, syringes, connector, and marker, prep sponges and iodine solution, sterile occlusive dressing and drape, and extension tubing.
Regional Nerve Block Needles
A wide array of needles is available for performing PNBs (Figure 3-10). Choice of needle depends on the block being performed, the size of the patient, and preference of the clinician. Needles are typically classified according to tip design, length, gauge, and the presence or absence of electrical insulation or other specialized treatment of the needles (e.g., etching for better ultrasound visualization).
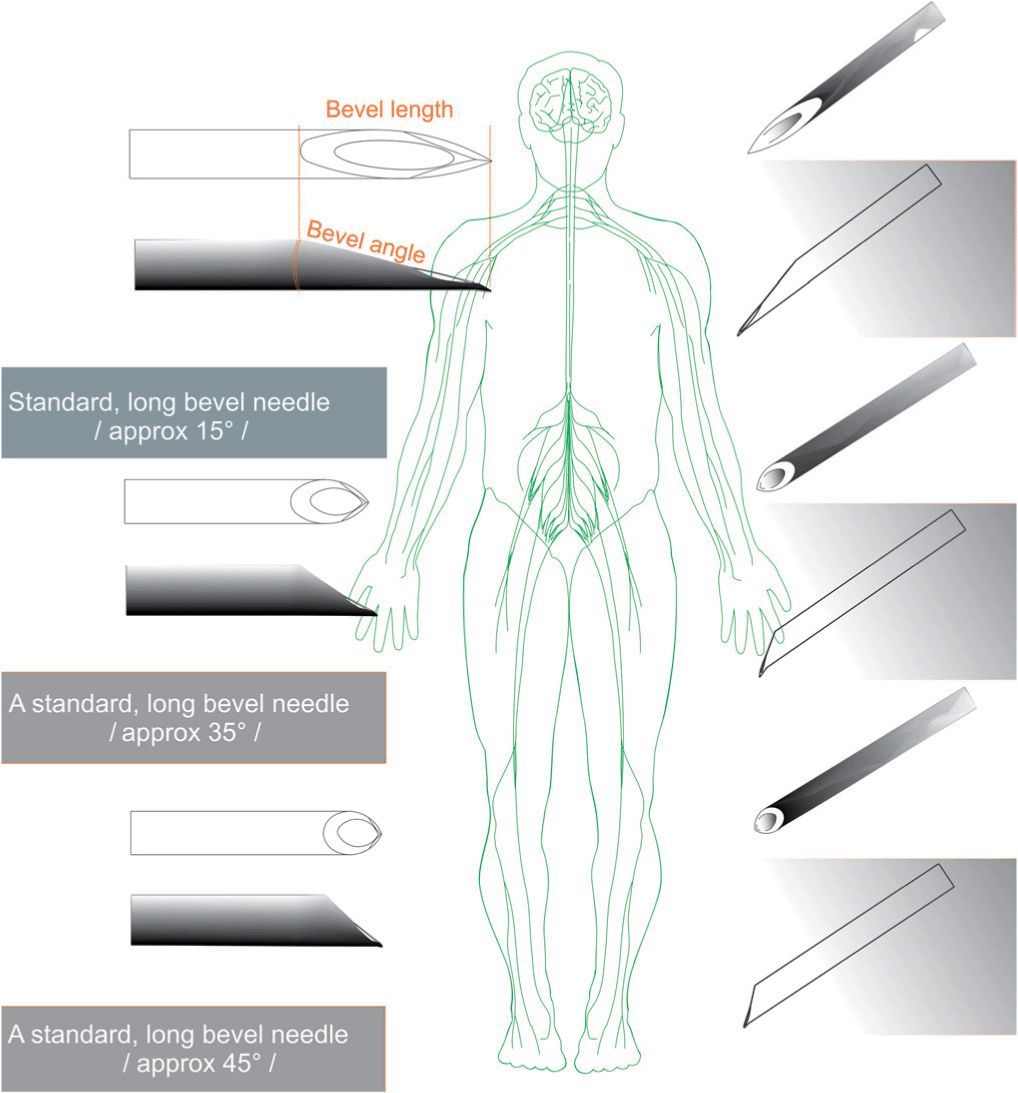
FIGURE 3-10. Common needle tip designs.
Needle Tip Design
Direct evidence for an association between needle tip design and the incidence of nerve injury is scarce. In a rabbit sciatic nerves model, Selander demonstrated that the risk of fascicle injury was lower when a short bevel needle penetrated a nerve as opposed to a long bevel needle.10 However, another experiment by Rice and colleagues suggested that the reverse may be true.11 This disparity might be explained by the fact that the study of Rice et al examined the effect of needle bevel design on the severity and consequences of intrafascicular should accidental fasicular penetration occur. Therefore, although it may be more difficult to enter a nerve fascicle with a short bevel needle as compared with a long bevel needle, the short bevel needle may cause a more severe lesion should a nerve be impaled by such a needle.12 Needle design can also have a direct effect on the anesthesiologist’s ability to perceive tissue planes. Tuohy and short bevel noncutting needles provide more resistance and thus enhance the feel of the needle traversing different tissues. Long bevel cutting needles, by contrast, do not provide as much tactile information while traversing different tissues. Pencil point needles may be associated with less tissue trauma than short bevel needles when bony contact occurs during spinal anesthesia, resulting in a lower incidence of postdural puncture headache.13 It is unclear however, whether pencil point needles have any advantage over other needle designs in practice of PNBs.
Needle Length
The length of the needle should be selected according to the type of block being performed (Table 3-2). A short needle may not reach its target. Long needles have a greater risk of causing injury due to increased difficulty in their handling and possibility of being inserted too deeply. The needle lengths recommended in this text are based on the author’s experience and are intended as a general guide. Note that the needle length is often longer by 2 to 3 cm for ultrasound-guided blocks because needles are inserted further from the target to visualize the course of the needle on the image. Needles should have depth markings on their shaft to allow monitoring for the depth of placement at all times.
TABLE 3-2 Block Technique and Recommended Needle Length
Needle Gauge
The choice of the needle gauge depends on the depth of the block and whether a continuous catheter is placed. Steinfeldt et al recently demonstrated the correlation between larger needle gauge and increasing levels of nerve damage after intentional nerve perforation in a porcine model.14 Thus, a small gauge needle may theoretically reduce the tissue trauma and discomfort to patients, whereas a long gauge needle bends more easily, making it more difficult to control. The needles of smaller caliber however, may also be more likely to penetrate the fascicles. In addition, needles of smaller gauges have more internal resistance, making it more difficult to gauge injection resistance and aspirate blood. Needles of very small size (25 and 26 gauge) are most commonly used for superficial and field blocks. Larger gauge needles (20–22 gauge) may be used in deeper blocks to avoid bending of the shaft and to maintain better control over the needle path. When placing a continuous catheter, the needle gauge must be large enough to allow passage of the catheter. Consequently, 17-19 gauge needles are most commonly used with an 18- gauge catheter for continuous catheters.
Echogenic Needles
Visualization of the needle tip is one of the more challenging aspects of performing an ultrasound-guided PNB. To facilitate the ease of needle visualization, specialized needle designs are being developed that allow greater visibility of the needle when performing ultrasound-guided PNBs. One example of such needle designs is coating with a biocompatible polymer that traps microbubbles of air, thus creating specular reflectors of air.15 The design improves needle visibility and aids in the performance of sonographically guided biopsies.16 Another echogenic needle design incorporates echogenic “dimples” at the tip to improve visibility.17 Unique texturing on the needle tip also demonstrated improvement in visibility.18 The design of echogenic needles is a continuously evolving field.
Ultrasound Machines
Ultrasound technology allows visualization of the anatomic structures, the approaching needle, and the spread of local anesthetic.19 Ease of use, image quality, ergonomic design, portability, and cost are all important considerations when choosing an ultrasound machine. To curtail costs, some institutions or practices purchase a single ultrasound machine to use for several purposes such as obstetrics, regional anesthesia, abdominal scanning, or echocardiography.20 Recently, a number of newer ultrasound machine models have evolved that are portable or can be mounted on the wall, which is beneficial in a setting where there is limited space to perform a block. The ultrasound technology is continually and rapidity evolving with an increasing focus on its application in regional anesthesia.
Sterile Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree