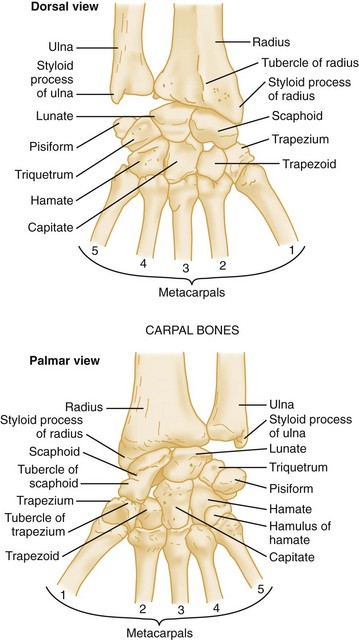
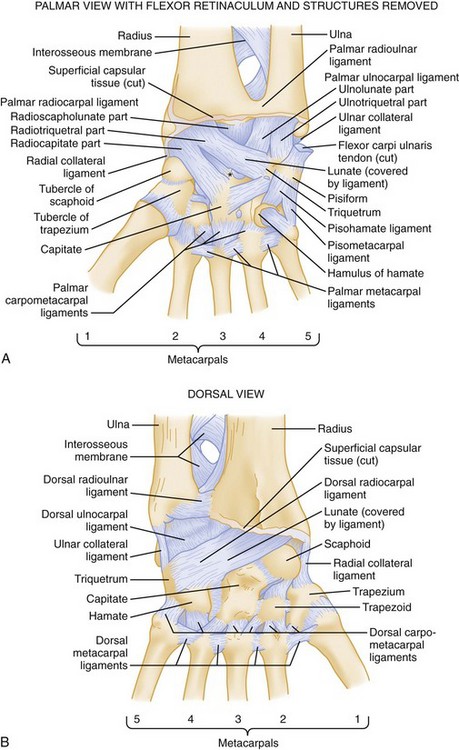
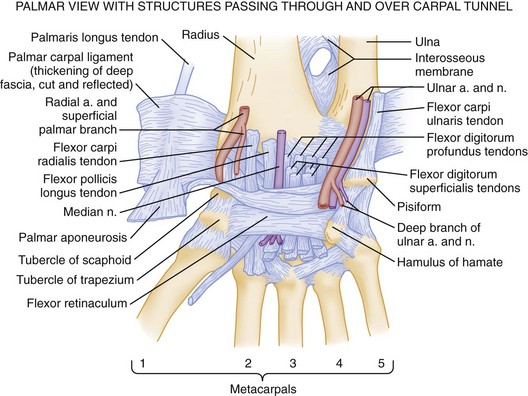
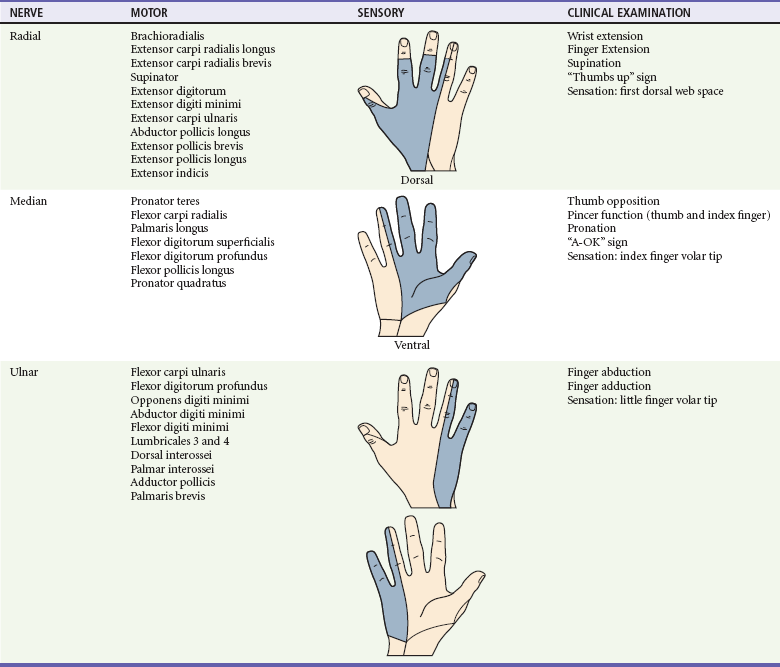
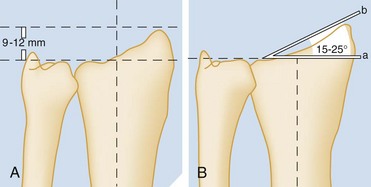
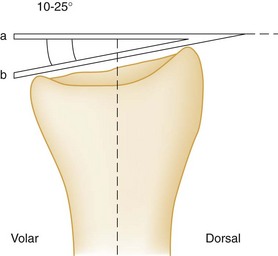
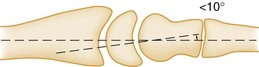
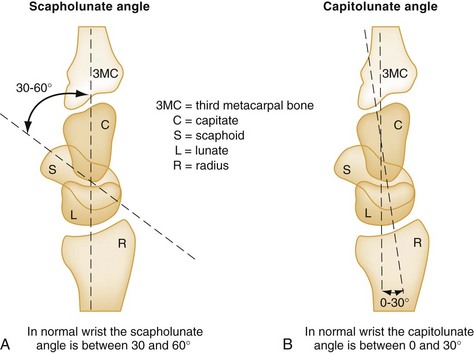
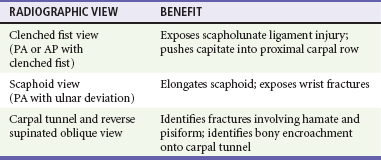
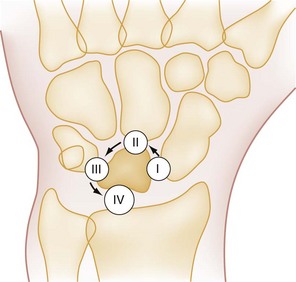
Chapter 51 The wrist includes the distal radius, ulna, and eight carpal bones, which are arranged in two transverse rows and commonly referred to as the carpus (Fig. 51-1). Each carpal row contains four bones. The more mobile, proximal row, listed radial to ulnar, consists of the scaphoid, lunate, triquetrum, and pisiform, whereas the distal row consists of the trapezium, trapezoid, capitate, and hamate bones. The stabilizing ligaments of the wrist joint are divided into two major groups: the intrinsic ligaments and the extrinsic ligaments. The intrinsic ligaments interconnect the individual carpal bones, and the extrinsic ligaments link the carpal bones to the distal radius, the ulna, and the metacarpals. The intrinsics are named for the adjacent bones they connect, and the most important for maintaining carpal stability are the scapholunate and lunotriquetral ligaments. The extrinsics are divided into a volar and dorsal group. The volar extrinsic ligaments are divided into two V-shaped ligamentous bands called the proximal and distal arcades, which generally are thicker and stronger than the dorsal extrinsic ligaments and are the most important in providing stability to the wrist. Between these volar arcades is an area relatively devoid of ligamentous support called the space of Poirier. This space enlarges when the wrist is dorsiflexed, and an injury to the joint capsule in this region can result in significant carpal instability (Fig. 51-2). The vascular supply to the wrist is provided by the radial and ulnar arteries, which join in a series of dorsal and palmar arches to supply the bones of the carpus. The intrinsic blood supply to most carpal bones enters the distal portion of the bone, leaving the proximal portion at risk for devascularization and avascular necrosis (AVN) when fractured. This is particularly true for the scaphoid, capitate, and lunate, because they each receive their blood supply from a single distal vessel (Fig. 51-3). The innervation of the wrist and hand is by the radial, median, and ulnar nerves. The radial nerve and the dorsal sensory branch of the ulnar nerve cross the dorsum of the wrist near the radial and ulnar styloids, respectively. The median nerve crosses within the carpal tunnel on the volar aspect of the wrist just radial and deep to the palmaris longus tendon. The ulnar nerve is within Guyon’s canal between the pisiform and the hook of the hamate (see Fig. 51-3). In the setting of trauma, motor and sensory function of the radial, median, and ulnar nerves may be assessed at the wrist and distally based on common clinical examinations (Table 51-1). On palpation, several bony prominences serve as useful landmarks, and the locations of these are best described in relation to the two major lateral and medial reference points in the wrist, the radial and ulnar styloids, respectively. Just distal to the radial styloid is the anatomic snuffbox, bordered radially by the abductor pollicis longus (APL) and extensor pollicis brevis (EPB) tendons and ulnarly by the extensor pollicis longus tendon. The body of the scaphoid is palpable within the snuffbox and is more prominent with the wrist in ulnar deviation.1 Lister’s tubercle can be palpated on the dorsum of the wrist just ulnar to the radial styloid. This is an important landmark because, notably, just distal to the tubercle lies the scapholunate joint, a common site of ligamentous injury in the wrist. With the wrist in neutral position, the capitate is palpable in a small depression found midway between the base of the middle metacarpal and Lister’s tubercle. Bringing the wrist into flexion can bring the lunate forward into a palpable position at this same site. Lister’s tubercle divides the second and third dorsal extensor compartments of the wrist and is also used as a primary landmark for radiocarpal arthrocentesis. Further ulnar on the dorsal side of the wrist from Lister’s tubercle is the DRUJ. The triquetrum is palpable just distal to the ulnar styloid in the proximal carpal row and can be made more prominent with radial deviation of the wrist. On a correctly positioned PA view of the wrist, the ulnar styloid arises from the lateral aspect of the distal ulna, and the extensor carpi ulnaris (ECU) tendon groove should be visualized at, or radial to, its base. The radial styloid process extends beyond the end of the articular surface of the ulna by a normal distance of 9 to 12 mm. This normal difference in length is called the radial length measurement (Fig. 51-4). There may be some degree of ulnar variance that affects the radial length measurement on a PA radiograph. The distal articular surface of the ulna may terminate before, at, or distal to the radiolunate articulation as a result of wrist rotation, flexion, extension, anatomic variation, or injury. Neutral ulnar variance (as seen in Fig. 51-4) is described when both the distal ulnar and radiolunate articular surfaces terminate at the same point distally. A positive ulnar variance (ulnar articulation is more distal) or negative ulnar variance (ulnar articulation is more distal) or negative ulnar variance (ulnar articulation is more proximal) is independent of styloid size and may be associated with wrist pathology (e.g., ulnar impaction syndrome and Kienbock’s disease, respectively). The ulnar slant of the articular surface of the radius, referred to as radial inclination, is visible on the PA view and normally measures 15 to 25 degrees (see Fig. 51-4). Both of these measurements are important in assessing the degree of radial shortening seen in association with some fractures of the distal radius.2 The normal appearance of the carpus on the PA view shows an approximately equal distance (usually 1 to 2 mm) between each of the carpal bones, and opposing articular surfaces are parallel to one another (an arrangement known as parallelism). On radiographs, three smooth curves normally can be drawn along the carpal articular surfaces, known as carpal or Gilula’s arcs (Fig. 51-5). Disruption of these curves or widening of the carpal spaces is an indication of carpal ligament disruption, instability, or fracture.3 The normal volar tilt of the distal radial articular surface is visible on the lateral view of the wrist and normally measures 10 to 25 degrees (Fig. 51-6). Adequacy of a lateral view of the wrist is assessed based on the relationship among the scaphoid, pisiform, and capitate projections. The palmar cortex of the pisiform should project midway between the palmar margins of the distal pole of the scaphoid and the capitate head, forming the S-P-C lateral (Fig. 51-7). The normal alignment of the distal radius with the lunate and capitate also is seen on the lateral view, which will show two concentric cups, the cup of the distal radius containing the lunate and the cup of the distal lunate containing the capitate. Ideally, the long axis of the radius, lunate, capitate, and third metacarpal should appear as a straight line on the lateral view, although the “normal” alignment usually is within 10 degrees of this line (Fig. 51-8). The carpal alignment on the lateral view is defined further by the scapholunate angle, which normally measures 30 to 60 degrees, and the capitolunate angle, which normally is 0 to 30 degrees (Fig. 51-9). Abnormalities in these angles are seen in patients with carpal ligament injuries and carpal instability. The soft tissues of the wrist also offer valuable clues to the presence of underlying bony injuries. It is estimated that on 90% of normal lateral radiographs of the wrist, the pronator quadratus line is visible as a linear, lucent, fat collection in the volar soft tissues just anterior to the distal radius and ulna (Fig. 51-10). Fractures of the distal radius or the ulna result in volar displacement, anterior bowing, or complete obliteration of this line. Although this pronator quadratus sign may suggest fracture, a wide range of sensitivities has been quoted—26 to 98%—so its absence does not exclude a fracture. A positive pronator quadratus sign has also been observed in soft tissue injuries and infectious and inflammatory medical conditions.4 Additional radiographic imaging of the wrist may be indicated based on chief complaint, mechanism of injury, or physical examination findings, including specific areas of tenderness. In addition to the standard PA, lateral and oblique wrist radiographs, adjunct imaging may include views with ulnar and radial deviation, maximal flexion, extension, a carpal tunnel view, reverse (supinated) oblique, clenched fist PA, or anteroposterior (AP) views. Patient-specific imaging helps to further delineate otherwise occult fracture or abnormal motion of the carpus resulting from ligamentous injuries. Specific scaphoid views, obtained with the wrist pronated and in ulnar deviation, allow for better visualization of the scaphoid along its long axis. The carpal tunnel view is performed with the wrist hyperextended and provides an axial image of the bony margins of the carpal tunnel. This view and the reverse (supinated) oblique view help identify fractures, especially involving the hook of the hamate and the pisiform.5 The clenched fist, both PA and AP views, drive the capitate proximally as a wedge causing diastasis within the scapholunate joint, highlighting ligamentous instability (Table 51-2). Although scapholunate width may be exaggerated on the AP view, instability is suspected when either view shows a distance of 3 mm or greater. The scaphoid is the most commonly fractured bone of the carpus.6 It accounts for approximately 70% of all carpal fractures. Typically seen in individuals 15 to 40 years of age, scaphoid fractures most commonly occur after a fall on the outstretched hand or as a sports-related injury.7,8 Scaphoid fractures are rare in skeletally immature patients because the carpus is composed entirely of cartilage at birth and remains predominantly cartilaginous until late childhood and the adolescent years.9 In pediatric patients, although the physis of the radius is likely to fail first, scaphoid fractures with and without this injury pattern have been observed.9 In the elderly, a distal radius metaphysis fracture is more likely to occur than a scaphoid fracture.8 Scaphoid fractures are classified by their anatomic location and may be divided into three groups: fractures of the tuberosity and distal pole, the waist, and the proximal pole. Of these three patterns, fractures through the waist of the scaphoid are the most common, accounting for approximately 70 to 80% (Fig. 51-11).8 Patients typically report dorsal radial wrist pain, distal to the radial styloid, with limited range of motion of the wrist and thumb. Classically, physical examination reveals tenderness on palpation of the scaphoid and swelling within the anatomic snuffbox. Increased sensitivities have been suggested for snuffbox tenderness with ulnar or radial deviation of the wrist with pronation. Pain also may be elicited with palpation of the scaphoid tubercle volarly, Watson’s scaphoid shift test, axial compression of the first metacarpal, and pain on thumb–index finger pinch.10 In an effort to not miss occult scaphoid fractures, the combination of clinical examination methods of tenderness in the anatomic snuffbox, on the scaphoid tubercle, and with first metacarpal compression has been suggested and may approach 100% sensitivity for disease.10 When routine radiography is negative, a combination of these clinical examinations is used for maintaining a high sensitivity for identification of occult fracture, despite a low specificity (40-80%).10–12 Radiographic diagnosis of scaphoid fractures often is difficult, and special scaphoid views should be requested when a fracture is suspected based on clinical findings. A visible fracture lucency may be absent, and a more subtle change, such as obliteration or displacement of the scaphoid fat pad, may be the only clue to the presence of a fracture, although these signs are not reliably present.13 Plain radiographs taken soon after injury fail to detect approximately 15% of scaphoid fractures.14,15 In addition, because of the associated risk of nonunion, when diagnosis and immobilization are delayed, patients clinically suspected of having a scaphoid fracture are often treated with splint immobilization and repeat clinical evaluation, and radiographic imaging after 7 to 10 days.16 Recent evidence has called into question the practice of immobilizing the wrist in all patients with suspected scaphoid injuries and has suggested that the use of more advanced imaging modalities is both accurate and cost-effective and should be performed earlier rather than later. The cost of time off from work, serial casting, repeat physician evaluation, and office visits easily exceed that of MRI, bone or CT scans for definitive diagnosis where these imaging modalities are readily available.17,18 In addition to advanced imaging, clinical risk assessments and decision rules are being developed to help further risk stratify patients.10 MRI and CT imaging allows clinicians to diagnose the majority of radiographically occult scaphoid fractures and offer alternative diagnoses for wrist pain.10,15 Macroradiography and ultrasound, including high-resolution sonography, have not approached the sensitivities and specificities observed with bone scintigraphy, MRI, and CT imaging. Despite extensive study, the optimal imaging modality and the sensitivity and timing of these studies in diagnosis of occult scaphoid fracture remain controversial.10,19 As a result, these imaging modalities are not emergently performed on a routine basis. Historically, bone scans were used 72 to 96 hours after injury to detect scaphoid fractures. Although high sensitivities are quoted (97%), lower specificities, many false positives, decreased effectiveness in the elderly, and limited availability have tempered their use.10,20,21 CT is excellent for detailed bone imaging, and it reveals the complications of fracture fragment displacement, malunion, and nonunion.22 However, CT has not had the sensitivity required (93%) for diagnosing occult fractures in the emergent setting. Despite increased costs and more limited availability, MRI protocols have the advantage of allowing diagnosis of alternative soft tissue injuries and are being used to detect these radiographically occult fractures with sensitivity rates approaching 100%.10,21,23–26 More prospective data on the optimal emergent and urgent diagnostic imaging modalities for occult scaphoid fractures are needed. The definitive treatment for uncomplicated, nondisplaced scaphoid fractures is debated among orthopedic specialists, although trends toward screw fixation over cast immobilization are evident.10 Emergency management typically involves immobilization in a thumb spica splint (Fig. 51-12). Immobilization with the wrist in 10 degrees of flexion with radial deviation is used to immobilize the fracture fragments of the scaphoid, and the majority of surgeons terminate the thumb spica at the interphalangeal joint line. Some specialists prefer a long arm (above the elbow) cast or splint, which prevents pronation and supination for the first few weeks. In addition to flexion and extension, pronation and supination have been suggested to produce fracture displacement in the proximal carpal row. Eventual replacement with a short arm cast for the remainder of the immobilization period may be acceptable. The duration of immobilization varies relative to the location of the fracture, but 6 to 12 weeks is common. More proximal fractures commonly require longer durations to ensure adequate healing. Variability in healing time is related directly to the pattern of blood supply to the scaphoid, which flows from the distal to the proximal portion of the bone through the scaphoid tuberosity. This pattern of blood flow also accounts for the higher incidence of AVN and nonunion in the more proximal fractures (Fig. 51-13). AVN is seen in approximately 13 to 40% and nonunion in 5 to 12% of scaphoid fractures, with the risk of complications being greatest in fractures of the proximal pole.27–29 Because of the increased risk of AVN or nonunion, scaphoid fractures, especially those that are unstable, are displaced more than 1 mm, are associated with other fractures, or have an increased scapholunate or capitolunate angle, require urgent orthopedic referral for consideration of operative treatment. Fractures of the lunate are relatively uncommon and represent approximately 1 to 4% of all carpal fractures.6,8,30,31 This injury occurs more commonly in persons with a congenitally short ulna, perhaps as a result of a compromised support for the TFCC. The usual mechanism of injury involves a fall on the outstretched hand, causing extreme dorsiflexion, with transmittal of the resultant force from the capitate to the lunate. Patients have pain over the dorsum of the wrist, which is exacerbated by axial loading of the long finger metacarpal. On physical examination, tenderness may be elicited by palpation over the dorsum of the wrist in the depression felt just distal to Lister’s tubercle. Fractures of the lunate may be difficult to see on plain radiographs because of overlap of the distal radius, ulna, and other carpal bones. For this reason, and because of the risk of AVN in missed injuries, clinically suspected lunate fractures should be immobilized. Nondisplaced lunate fractures are treated with immobilization in a short arm splint with a thumb spica, and patients are given orthopedic referral in 7 to 10 days. Displaced fractures should be reduced, and urgent orthopedic referral is warranted. Complications include progression to carpal instability, nonunion, and AVN. Lunate and perilunate dislocations are discussed later in the section on carpal instability. Post-traumatic AVN is a sequela in 20% of fractures and is presumed to be the cause of Kienbock’s disease. In well-established cases of Kienbock’s disease, the lunate appears sclerotic and fragmented on radiographic examination, and ultimately the bone collapses with resultant proximal migration of the capitate (Fig. 51-14). These changes cause secondary osteoarthritis of the radiocarpal joint and chronic wrist pain. Treatment involves operative intervention, with correction of the articular abnormalities either by lengthening the ulna or by shortening the radius. In more advanced cases, excision and prosthetic replacement of the lunate or arthrodesis may be necessary.32 Triquetrum injuries, second only to the scaphoid in incidence, account for approximately 15% of carpal fractures.8 They usually result either from a direct blow to the bone, causing a fracture of the body, or much more commonly from a fall on the outstretched hand. In the former scenario, triquetrum body fractures are commonly associated with perilunate and lunate dislocations, and therefore ligamentous injury should be considered. A fracture to the triquetral body is best seen on the AP radiograph, and urgent orthopedic referral is suggested. In the latter scenario, the mechanism of fracture is believed to be impact of the ulnar styloid or proximal hamate against the triquetrum, which results in a dorsal avulsion fracture.31,33 Patients have localized tenderness over the dorsum of the wrist just distal to the ulnar styloid. On physical examination, swelling may be noted in this same area, and wrist motion is limited secondary to pain. The fracture is best seen on the standard lateral view of the wrist as a small dorsal avulsion fragment, although, a more oblique pronated view may be necessary for visualization (Fig. 51-15). Treatment is with immobilization in a short arm splint or ulnar gutter with more routine orthopedic referral (1-2 weeks). Definitive treatment in a short arm cast usually results in an uncomplicated course, with prompt fracture healing over 4 to 6 weeks. The pisiform is unique in the carpus because it is the only sesamoid bone and lies within the FCU tendon, articulating on its dorsal surface with the triquetrum. Although pisiform fractures are extremely rare, occurring in less than 1% of all carpal fractures, given the important role of the pisiform in forming the lateral wall of Guyon’s canal, ulnar arterial damage and neurapraxias may be associated. Fractures of the pisiform usually occur from a fall on the outstretched hand but also may be seen after direct blows to the hypothenar eminence. Commonly this occurs from repetitive trauma when the palm of the hand is used in a hammer-like manner. On clinical examination, there is tenderness over the ulnar aspect of the wrist just distal to the volar crease. Pain may be exacerbated with wrist flexion and ulnar deviation. Paresthesias in the distribution of the ulnar nerve and hand clumsiness from intrinsic muscle dysfunction can occur. Pisiform fractures are poorly seen on routine wrist radiographs and are therefore likely under-reported, so special views should be requested. A reverse (supinated) oblique and the carpal tunnel view allow for better visualization of these fractures (Fig. 51-16).4 Hamate fractures are rare and account for approximately 2 to 6% of all carpal bone fractures.8 The hook or hamulus is the most common site of fracture, although articular surfaces and body fractures are also seen. Fracture of the hook usually occurs from a fall on the outstretched hand or from a direct blow to the palm. Classically, hook of the hamate fractures occur from those participating in racquet or club sports (e.g., tennis, golf, baseball). The use of hammers and vibration equipment (e.g., jack hammers) is also a common mechanism, which can predispose workers to hamate fractures, ulnar canal and hypothenar hammer syndrome.34 Patients may have isolated pain over the hypothenar eminence, associated decreased grip strength, or compromised distal perfusion. Pain may be localized directly on palpation of the hamate, 1 cm distal and radial to the pisiform. Hamate body and articular surface fractures are usually caused by increased load to the ring and little finger metacarpals. These fracture patterns are best seen on PA views of the wrist (Fig. 51-17). Fractures of the hook are more easily seen on the reverse supinated oblique and carpal tunnel views (Fig. 51-18).4 Because low sensitivities have been quoted for hook of the hamate fractures (40-70%), when radiographs are inconclusive and pathology is still suspected, CT scanning may be considered given its increased sensitivity, the complications of missed fracture, and changes in clinical management. The timing of CT scanning is debatable, and empirical treatment may be warranted. However, confirmed hook of hamate fractures should be splint immobilized with ulnar outrigger and thumb spica to limit traction from the transverse carpal ligament. Missed injury may result in complications, including delayed flexor tendon rupture affecting the little finger.5,35 Fractures of the hook of the hamate may also be complicated by associated ulnar neurapraxia, which would warrant urgent orthopedic referral and is an indication for operative intervention with excision of the hook at the fracture site to restore function.5 Vascular compromise or distal ischemia would warrant emergent orthopedic consultation.36 Hamate body and articular fractures typically require closed or open reduction and internal fixation. Fractures of the trapezium are also uncommon and represent approximately 3% of all carpal fractures.8 There are two main types of fractures, those involving the body and the trapezial ridge. A direct blow to the adducted thumb causes fracture through the body of the trapezium, with transmittal of the force by the base of the thumb metacarpal. Avulsion fractures of the trapezial ridge occur with forceful radial deviation or rotation of the wrist. On examination, patients report pain with movement of the thumb and on direct palpation of the trapezium just distal to the scaphoid in the anatomic snuffbox. Although trapezium fractures may be seen on the AP view of the wrist, they are typically better visualized on oblique views (Fig. 51-19) and unfortunately are also commonly occult.35 These injuries are treated with immobilization in a thumb spica splint, and patients are given orthopedic referral. Nondisplaced fractures are held in a cast for 6 weeks, whereas displacement or involvement of the carpometacarpal joint warrants urgent orthopedic referral for ORIF. Trapezoid fractures are rare, most commonly seen in association with other carpal injuries, and account for only approximately 1% of all carpal fractures.5 The typical mechanism of injury is a direct blow down the long axis of the index metacarpal, which may result in isolated fracture to the trapezoid or cause a dorsal fracture-dislocation. On clinical examination, pain and tenderness are localized over the dorsum of the wrist at the base of the second metacarpal. The fracture may be visible on routine PA views of the wrist; however, oblique views may be superior for visualization of the injury. Nondisplaced trapezoid fractures should be immobilized with a short arm splint and thumb spica, and patients are given an orthopedic referral in 1 to 2 weeks. However, displaced fractures warrant urgent orthopedic referral for reduction and fixation. Mayfield and associates described a progressive pattern of carpal ligamentous injury caused by wrist hyperextension, ulnar deviation, and intercarpal supination.37 Their studies of the pathomechanics of these injuries led to the classification of carpal instability into four distinct stages. Each stage represents a sequential intercarpal injury beginning with scapholunate joint disruption and proceeding around the lunate, creating progressive carpal instability (Fig. 51-20). Each stage also may be associated with specific bony fractures, which, if present, should alert the physician to the possibility of an occult perilunate ligamentous injury. These associated injury patterns include fractures of the radial styloid, scaphoid, capitate, and triquetrum.
Wrist and Forearm
Wrist
Anatomy
Clinical Features
Diagnostic Strategies: Radiology
Carpal Injuries
Lunate Fractures
Triquetral Fractures
Pisiform Fractures
Hamate Fractures
Trapezium Fractures
Trapezoid Fractures
Carpal Instability
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Wrist and Forearm
Only gold members can continue reading. Log In or Register to continue