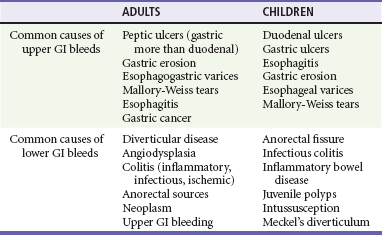
Chapter 30 Gastrointestinal bleeding (GIB) accounts for more than 1 million hospitalizations annually in the United States, with significant morbidity, mortality, and economic burden.1 GIB is traditionally classified by the bleeding source—upper GIB (UGIB) is proximal and lower GIB (LGIB) is distal to the ligament of Treitz in the terminal duodenum. UGIB accounts for more than 500,000 U.S. hospital admissions annually, with approximately 165 incidents per 100,000 patients.1 Mortality rates have remained consistent at 13 to 14% over the past two decades despite advances in medical therapy, intensive care unit (ICU) management, endoscopy, and surgery.2 An increasing proportion of elderly patients, who may die owing to comorbid conditions, and increases in the number of cirrhotic and variceal patients may contribute to the lack of change in mortality rates. In the United States, hospitalized patients with and without complications of nonvariceal UGIB had a mean length of stay of 4.4 and 2.7 days and hospitalization costs of $5632 and $3402 (2004 U.S. dollars), respectively.3 The characteristics of the bleed and the age of the patient can help determine the cause of the GIB. UGIB can routinely manifest as bloody or coffee-ground–like vomit known as hematemesis or as dark, tarry stools known as melena. In adults, peptic ulcer disease, erosive gastritis, and esophageal varices account for the majority of these cases4,5 (Table 30-1). In fact, peptic ulcers make up more than half of all acute cases of UGIB seen in the emergency department (ED). However, in inner city populations, varices and gastritis are more prevalent. In pediatric patients, gastric and duodenal ulcers, esophagitis, gastritis, esophageal varices, and Mallory-Weiss tears account for most cases of UGIB, in descending order of frequency. Contrary to this, LGIB usually produces bright red or maroon blood per rectum, known as hematochezia. Anorectal sources, such as hemorrhoids, are the most common causes of LGIB in all age groups.6 In adults, the most common sources of hematochezia are colonic diverticula and angiodysplasia.7 Other noteworthy causes include colitis caused by ischemia, infection, and inflammatory bowel disease. Major causes of LGIB in children include anorectal fissures and infectious colitis. Bleeding can also be caused by intussusception and Meckel’s diverticulum in infants and toddlers. Despite diagnostic advances for all ages, the source of GIB is not identified in 8 to 14% of patients.2 Death from exsanguination resulting from GIB is rare. However, there are two causes of GIB that may rapidly cause death if not recognized and mitigated: esophageal varices and aortoenteric fistula. The former is the single most common source of massive UGIB and has a mortality rate of 30%. The latter is caused when an abdominal aortic aneurysm or, more commonly, an aortic graft adheres to and erodes through a bowel wall. Aortoenteric fistula is a rare but rapidly fatal cause of LGIB.7 As is the case for any patient with acute massive hemorrhage, prompt consultation with a surgeon is warranted when aortoenteric fistula is a likely diagnosis. Finally, in the differential considerations, one must determine if in fact the patient is having actual GIB. Epistaxis, dental bleeding, or red food coloring can mimic the appearance of hematemesis. Bismuth-containing medications and iron supplements can create melanotic-appearing (but guaiac-negative) stools. Vaginal bleeding, gross hematuria, and partially digested red foods (such as beets) can all be mistaken for hematochezia.8 Unless an alternative diagnosis is clearly evident, the appropriate approach is to continue with the workup for GIB. 1. Context: The context of the bleeding can help explain its cause. For instance, if a patient complains of bright red blood per rectum after several days of constipation and straining, that presentation suggests an anorectal source for the bleeding. Alternatively, a patient with hematemesis after several earlier episodes of retching would lead one to suspect an esophageal tear. Finally, a patient with easy bruising and recurrent gingival bleeding might suggest a long-standing, underlying coagulopathy. 2. Quantity: Efforts should also be made to quantify the amount of blood lost during the bleeding event. Patients may describe the passage of large clots, blood changing the toilet bowl water red, or simply streaks of blood on the toilet paper. The patient’s recollection of the bleed and its amount is usually poorly quantified and inaccurate. Often, the degree of bleeding is better gauged by assessing symptoms associated with significant intravascular loss such as dyspnea, lightheadedness, or chest pain.9 These findings demonstrate signs of decreased oxygen-carrying capacity that often accompanies significant blood loss and should prompt a thorough and expeditious workup. 3. Appearance: Classifying the blood as hematemesis, melena, or hematochezia provides the initial clues to the source of bleeding. Vomiting of fresh blood or blood with the appearance of coffee grounds strongly suggests an upper GI (UGI) source. The passage of melena, dark digested stools, also suggests likely UGIB. In contrast, the presence of hematochezia, bright red or maroon stools, usually signifies LGIB. There are exceptions, however. In a hemodynamically unstable patient, bright red blood per rectum can represent brisk UGIB. Hematemesis rarely can arise from a source in the lower GI (LGI) tract that is proximal to an obstruction. Although the definitive cause and location of the bleed will usually be determined by the gastroenterologist, the emergency clinician uses the history to make a rough estimate of the source and help guide the initial workup.8 4. Relevant medical history: A review of the patient’s relevant medical history and risk factors for bleeding should note whether a patient has had similar bleeding before and the location of the causative lesion (Table 30-2). This is especially important with UGIB, as the majority of these presentations are caused by rebleeding of previously identified sources. Next, identification of relevant comorbid diseases helps to risk stratify these patients in the context of their bleed. Patients with GIB and a history of coronary artery disease, congestive heart failure, liver disease, or diabetes have a higher mortality and therefore may require earlier or more extensive intervention.8 A review of the patient’s medications should pay particular attention to gastrotoxic substances, anticoagulants, and antiplatelet drugs. Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, warfarin, clopidogrel, corticosteroids, and certain chemotherapeutic agents are known to increase the risk of GIB.5,8 In addition, reviewing the patient’s social history can identify activities that increase risk for GIB. Alcohol abuse is associated with gastritis and peptic ulcer disease. It can also result in cirrhosis, portal hypertension, and ultimately esophageal variceal bleeding. Smoking cigarettes results in slower healing and greater recurrence of ulcers. These two social habits are also closely associated with gastrointestinal malignancy—another, albeit rare, risk factor for GIB. Vital Signs.: Hypotension and tachycardia can suggest moderate hypovolemia and can be the early indicators of impending shock.5,8 Orthostatic vital signs, although frequently used, are of dubious value in determining volume status in the context of acute blood loss. General Examination.: Eye examination may show conjunctival pallor, suggesting blood loss anemia. In similar fashion, dermatologic changes can lend supporting evidence to the presence and cause of a GI bleed. Generalized pallor in a hemodynamically stable patient might indicate the anemia of a subacute or chronic GIB; in the unstable patient, pallor might reinforce the impression of massive blood loss. Cold, clammy skin on the extremities might signal significant volume loss consistent with hemorrhagic shock. Ecchymoses or petechiae suggest a coagulopathy. Finally, jaundice, palmar erythema, or spider angiomata suggests the possibility of UGIB from esophageal varices.5 The abdomen should be carefully examined for subtle findings that can help identify the source of bleeding. Hyperactive bowel sounds are a nonspecific finding, but might indicate UGIB, as intraluminal blood is a known cathartic that can stimulate peristalsis.5 Tenderness to palpation can be seen in many cases of peptic ulcer disease. Severe, diffuse tenderness on examination warrants the consideration of bowel ischemia, mechanical obstruction, ileus, or bowel perforation. Evidence of peritonitis merits a rapid surgical consultation for possible operative management. The abdominal examination may also show further signs of portal hypertension with the presence of hepatomegaly, ascites, or caput medusae.5 A rectal examination, with determination of the type of bleeding, should be performed in most patients with GIB. The examination should include evaluation of the external anus, a digital rectal examination, and anoscopy looking to identify possible bleeding sources such as hemorrhoids, polyps, or fissures.5,7,8
Gastrointestinal Bleeding
Perspective
Diagnostic Approach
Pivotal Findings
Medical History
Physical Examination
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Gastrointestinal Bleeding
Only gold members can continue reading. Log In or Register to continue