186 Wound Repair
• Thoughtful consideration of the patient, characteristics of the wound, and selection of an appropriate technique for closure is the most important aspect of wound care.
• Antibiotics are not a substitute for adequate wound preparation, irrigation, and exploration.
• Following gross decontamination, the pressure of an irrigating stream must be sufficient to overcome the adhesive force of bacteria (5 to 12 psi).
• Proper skin eversion and suture placement make a difference and take no significantly greater amount of time than does hastily managing a wound.
• Address tetanus status and allergies in all patients.
• Immobilization, a clean moist environment, elevation, and avoidance of sun are the key elements of aftercare.
• Diligent documentation needs to include information regarding the patient’s characteristics, the wound’s appearance, previous care, assessment of the functionality of surrounding structures before and after intervention, and steps taken to reduce infection, as well as the actual closure technique.
Acknowledgment and thanks to Dr. E. Parker Hays, Jr., for his work on the first edition.
Epidemiology
Approximately 12 million wounds are treated in EDs in the United States each year.1 Data on the true incidence of wounds are limited because many are thought to be treated away from the ED or urgent care setting. Of individuals with wounds seen in the ED, the majority are men.2 Wounds can clearly occur anywhere on the body, but lacerations on the upper extremities, head, and neck constitute the majority of cases encountered in EDs.
Pathophysiology
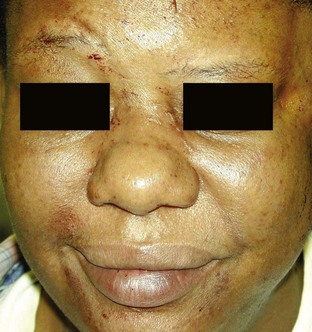
Skin, the largest organ in the body, has numerous functions, most prominently heat exchange, prevention of infection, and provision of a tactile interface with the environment. The layers of skin—epidermis, dermis, and connective tissue—all play different roles in wounds and healing. The thickest and most important layer, the dermis, serves as structural integument, supports conveyance of nutritional and waste products, and contains cutaneous nerves (Fig. 186.1).
Presenting Signs and Symptoms
Wound repair may be sought intentionally or be required following evaluation of other complaints, such as a syncopal event. It is not uncommon for patients to be entirely unaware of their wounds (as in trauma) or to be unimpressed with the severity of their lesion because of more painful conditions, such as a fracture. For all these reasons, a thorough physical examination plus evaluation of all wounds is required. Through this evaluation and assessment of the patient’s unique situation, an appropriate approach may be undertaken to address a wound. The overall risk for infection and the likelihood of complications can be predicted by considering wound and host factors. A major pitfall of wound management is fixation on the wound without sufficient attention to the host. For example, a 4-cm linear laceration on the arm of a healthy 18-year-old patient has a different prognosis than the same wound on the shin of a 73-year-old diabetic patient with peripheral vascular disease (Box 186.1).
Differential Diagnosis and Medical Decision Making
Patient Evaluation
A wound is the physical manifestation of an injurious force exerted on the body. Accordingly, careful evaluation of the patient as a whole is critical. A common pitfall is focusing on the most visible injury and not recognizing other lesions that were caused by one event, such as trauma. Understanding the injurious mechanism also enables better prediction of the wound’s severity. As an example, blunt force injuries have significantly greater potential for diffuse tissue nonviability and are consequently more prone to infection.3 Once all injuries have been catalogued, each may be addressed. Important considerations include knowing how the patient was injured (shear, abrasion, compression), whether the location of the wound is in a cosmetically or functionally vital area, and whether potentially confounding influences on the potential for healing are present.
Injury to Underlying Structures
When sufficiently breached, skin fails in its protective role and may allow underlying structures to be injured (Fig. 186.2). Diligent assessment of the functionality of surrounding anatomic structures is of utmost importance.
Foreign Bodies
Foreign bodies can be driven into wounds through innumerable routes of entry. Common situations include shattered glass in motor vehicle accidents, vegetative material in wounds during outdoor pursuits, and puncture wounds through footwear. Foreign bodies increase the risk for infection and may prevent healing. The following section on puncture wounds specifically addresses foreign bodies in these situations. For additional discussion of foreign body evaluation and management, see Chapter 187.
Treatment
The emergency physician (EP) can close most wounds; some situations requiring specialist consultation are listed in Box 186.2.
Box 186.2 Wounds Requiring Specialty Consultation
Wound Preparation
Tips and Tricks
Wound Preparation
Sterile Technique
Use of sterile fields, gloves, caps, masks, and gowns is de rigueur in operating room surgery but not as well established in routine wound closure. Studies have shown that the use of sterile versus nonsterile boxed gloves in routine wound management may not have a significant effect on the rate of infection.4 Powdered gloves should be avoided because of their association with granuloma formation, and EPs must be aware of possible latex allergy.
Anesthesia
In general, anesthesia should precede significant efforts at cleansing, irrigation, exploration, and closure. Despite long-held dogma, lidocaine with epinephrine can be used in most areas of the body, including the majority of hand wounds and digital blocks.5 For a complete discussion of local and regional anesthesia, please see Chapter 188.