34 Mesenteric Ischemia
• Severe abdominal pain out of proportion to the findings on physical examination should always raise suspicion for mesenteric ischemia, especially in elderly patients.
• The presence of hypotension, atrial fibrillation, severe cardiovascular disease, or recent myocardial infarction increases the likelihood of mesenteric ischemia.
• No serum marker is sensitive or specific enough to establish or exclude the diagnosis of bowel ischemia.
• Bloody diarrhea is a late finding that indicates mucosal sloughing—do not wait for the appearance of hematochezia or melena to make the diagnosis of mesenteric ischemia.
• Patient survival improves with early mesenteric angiography or surgical intervention (or both).
Epidemiology
Mesenteric ischemia accounts for 0.1% of all hospital admissions and 1% of emergency department (ED) visits for abdominal pain in geriatric patients. Cases of mesenteric vein thrombosis are more difficult to estimate accurately but have been reported at 2 per 100,000 admissions over a period of 20 years at one center.1–3
The overall mortality associated with mesenteric ischemia is between 60% and 93% but rises precipitously once bowel wall infarction has occurred. Mortality remains greatest for acute mesenteric ischemia resulting from obstruction or embolic phenomena. Patients with an early manifestation of NOMI have mortality rates of 50% to 55%, whereas patients with mesenteric vein thrombosis have a 15% mortality at 30 days.1–3 Those affected by chronic mesenteric ischemia have a more prolonged course, are relatively protected by dual blood supply, and present the physician with more numerous chances for intervention.
Pathophysiology
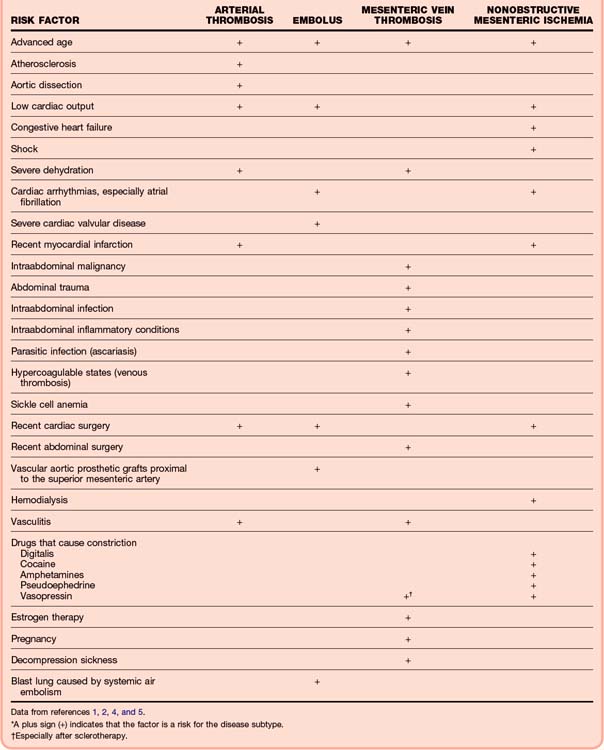
Any patient with advanced age, atherosclerosis, thromboembolic disease, atrial fibrillation, and processes leading to chronic low-flow states is at risk for the development of arterial mesenteric ischemia (Tables 34.1 and 34.2).1,2,4,5 Mesenteric venous obstruction carries its own separate risk factors, which are similar to those for venous thrombosis anywhere in the body.
Table 34.2 Incidence of Ischemic Bowel Diseases
| DISEASE | INCIDENCE (%)* |
|---|---|
| Superior mesenteric artery (SMA) embolism: | 50 |
| The SMA is susceptible to embolism because of large vessel caliber and a narrow angle of departure from the aorta. | |
| The proximal SMA is most commonly obstructed within 6-8 cm of the aorta. | |
| Nonocclusive ischemia | 25 |
| SMA thrombosis | 20 |
| Mesenteric venous thrombosis | 5 |
* Percentage of all cases of acute mesenteric ischemia.
Bowel perfusion is generally preserved during periods of hypotension; therefore, NOMI represents failure of the normal autoregulatory systems.2,6,7 Patients with chronic renal failure may have bowel ischemia after hemodialysis, probably from hypoperfusion, which promotes preferential shunting of blood from the splanchnic circulation to preserve flow to the cardiac and cerebrovascular systems.
Although acute mesenteric vein thrombosis accounts for a small proportion of cases of ischemic bowel disease (5% to 10%), the ease of diagnosis with computed tomography (CT) has allowed identification of a greater number of patients with venous thrombosis. Symptoms are even less specific than those of arterial obstruction and are manifested over a longer period before bowel infarction occurs. Thrombus secondary to hypercoagulable states develops first in the smaller vessels and later progresses into the larger veins; clots associated with cirrhosis, neoplasm, or local injury (operative, trauma) start at the site of obstruction and evolve distally.4
There is a significant array of collateral blood vessels and flow patterns. The small intestine is especially vulnerable to ischemia, however, because the terminal arterioles enter the intestinal wall without collateral pathways.4 Splanchnic blood flow requirements vary continuously but can account for up to 35% of cardiac output.
Presenting Signs and Symptoms
Classic Presentation
Clues to diagnosis of the various ischemic bowel diseases are as follows:
• Acute abdominal pain followed by rapid and forceful evacuation of the bowels (vomiting or diarrhea) strongly suggests an embolic phenomenon in the SMA.
• Long-standing abdominal pain (weeks to months), which is then followed by acute worsening, suggests intestinal angina and SMA thrombosis.
• Patients with risk factors for NOMI may have unexplained abdominal distention or gastrointestinal bleeding; pain is totally absent in up to 25% of these patients, and unexplained distention may herald infarction.
![]() Documentation
Documentation
Onset, severity, and duration of symptoms
Presence of melena or hematochezia
Presence or absence of risk factors
Vital signs: evidence of shock, sepsis
Findings of cardiac, full abdominal, genitourinary, and rectal examinations
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree