If breathing is present then do the following.
Look for the Signs of Partial Upper Airway Obstruction
- Snoring: the familiar sound of obstruction caused by the soft tissues of the mouth and pharynx. Often it accompanies the reduced muscle tone of a lowered level of consciousness.
- Rattling or gurgling: the sound of fluids in the upper airway.
- Stridor: a harsh, ‘crowing’ noise, which is heard best in inspiration. It is thus different from wheezing, which is usually loudest in expiration. Stridor suggests obstruction at the level of the larynx and upper trachea. General illness and temperature usually indicate an infection causing swelling. Obstruction by a foreign body is the other main cause.
- Drooling: the inability to swallow saliva. It suggests blockage at the back of the throat.
- Hoarseness: gross voice change. This suggests obstruction at the level of the larynx.
Clearance and Maintenance of the Airway
A patent airway is a prerequisite for life; a blocked airway is a common harbinger of death in emergency situations. There are two main ways in which the airway becomes blocked.
This is overcome by:
- tightening these tissues (chin-lift manoeuvre)
- pushing the jaw and the hyoid bone and their attached soft tissues forward (jaw-thrust manoeuvre)
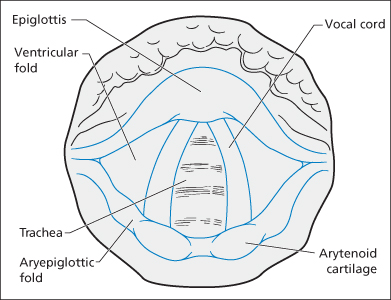
- putting an artificial airway down the anatomical airway (oro- or nasopharyngeal airways, endotracheal tubes, laryngeal masks, etc. → Figure 1.1).
This is overcome by:
- removing the cause of the obstruction (suction, manual removal or choking manoeuvres)
- passing an artificial airway (as detailed above) past the obstruction
- reducing the swelling with vasoconstrictor drugs (adrenaline)
- bypassing the obstruction with a surgical airway.
Protection of the Airway
The airway is normally kept clear of foreign matter by the gag, cough and laryngeal reflexes. These may be attenuated by specific palsies, the effects of drugs or a generalised depression of conscious level. They may also be impaired at the extremes of age and in states of general debilitation. Special vigilance is required in all such situations; the recovery position should be used whenever possible.
Paradoxically, these same reflexes may make advanced airway care extremely difficult in situations where they are not completely absent. At such times, the airway should be managed by a person skilled in both its assessment and the use of sedating and paralysing drugs.
Laryngospasm, bleeding, vomiting and consequent hypoxia can result from ill-judged attempts at intubation. It should be noted that the absence of the gag reflex is not a good predictor of the need for (or the ease of) endotracheal intubation.
On-going protection of the airway requires continual vigilance. The following are also essential:
- The recovery position uses gravity, both to drain fluid matter away from the airway and to allow the soft tissues to be positioned in such a way that they do not cause obstruction. Once the airway is clear, this position can be used to both maintain and protect the airway.
- A high-flow suction catheter must always be near the patient’s head.
- The patient’s trolley must be capable of tilting ‘head down’ so as to drain vomitus out of the airway.
- If endotracheal intubation is attempted, the airway must be protected by the manoeuvre known as cricoid pressure throughout the period of instrumentation. Pressure is applied to the front of the patient’s cricoid cartilage by an assistant using the thumb and two fingers. This compresses the oesophagus against the cervical spine and thus prevents the passive regurgitation of gastric contents. The airway is vulnerable from the start of induced paralysis until the cuff is inflated on a correctly positioned endotracheal tube.
Protection of the Cervical Spine
If the patient has an injury to the cervical spine, there is a risk of damage to the spinal cord during the procedures needed to maintain the airway. Because of the terrible outcome of such damage, it is mandatory to protect the neck immediately in patients who are:
Adequate protection of the potentially unstable cervical spine consists of a rigid collar and either a purpose-made cervical immobiliser or sandbags and tape.
B – Breathing
Breathing is the means by which oxygen is delivered to the alveoli and thus made available to the circulating red cells. At the same time carbon dioxide (CO2) is eliminated.
Look for
- Difficulty in talking
- Abnormal respiratory rate: usually fast, laboured breathing. Very slow respiratory rates may occur just before respiratory arrest or as a consequence of poisoning with narcotic drugs, e.g. methadone
- Nasal flaring and use of shoulder and neck muscles.
- Paradoxical respiration: a see-sawing movement of the chest and abdomen, which indicates obstruction of either the upper or lower airways or fatigue of the diaphragm.
- In children, recession of the chest wall: indrawing of the elastic tissues caused by increased respiratory effort.
All the above suggest that the patient is struggling to achieve normal respiration. Failure to oxygenate the blood adequately and hence the tissues is shown by:
- Tachycardia – the nervous system has detected hypoxia and is stimulating the heart
- Pallor and sweating – caused by sympathetic stimulation
- Cyanosis – a late sign
- Irritability, confusion or reduced responsiveness – the brain is short of oxygen. This is an extremely worrying sign
- A low SaO2 (<94%) – pulse oximetry should be established as soon as possible
- Unequal, diminished or abnormal breath sounds
- Hyperresonance or dullness to percussion
- Displacement of the trachea or apex beat
- A flail segment
Oxygen Therapy
The common denominator of all life-threatening illness, regardless of cause, is a failure to deliver adequate amounts of oxygen to the tissues. In normal circumstances, the oxygen content of atmospheric air (21%) is perfectly adequate but when the mechanisms for breathing are diseased or traumatised supplemental oxygen should be given. The physiological compensatory mechanisms for hypoxia and hypovolaemia all consume oxygen themselves; the immediate administration of supplemental oxygen may maintain these reflexes while more definitive measures are put in place. There are really only two main types of oxygen therapy:
The dangers of high-concentration therapy are known to every medical student. The patient with a chronically raised blood CO2 level may depend on a hypoxic drive to stimulate breathing – give him or her oxygen and the breathing slows, CO2 levels rise even higher and the patient becomes comatose with CO2 narcosis. In practice, these patients are a small group in whom the speed of onset of symptoms can be used to determine treatment (→ pp. 199 and 205).
 Box 1.1 Summary of the BTS Guideline for Emergency Oxygen Use in Adult Patients (British Thoracic Society Emergency Oxygen Guideline Group 2008)
Box 1.1 Summary of the BTS Guideline for Emergency Oxygen Use in Adult Patients (British Thoracic Society Emergency Oxygen Guideline Group 2008)Hypoxia is a swift killer and so patients in the resuscitation room invariably require a high concentration of oxygen. The use of a mask that has a reservoir bag improves the effectiveness of oxygen delivery (to perhaps 60–80%) and should be standard. (The reservoir bag is needed because a patient’s inspiratory flow is always greater than the 15 L/min maximum flow from the oxygen supply.) Blood gases must be obtained at an early stage to monitor the effect of supplemental oxygen. If improvement is not satisfactory, then ventilation may be needed. Continuous positive airway pressure (CPAP) is another method of increasing oxygenation.
Mechanical Ventilation
This should always be considered when:
- the patient cannot maintain a clear airway
- oxygen enrichment of the inspired gases fails to prevent the signs of cerebral hypoxia
- CO2 narcosis is present
- there has been a successful but prolonged resuscitation from cardiac arrest
- the patient is multiply injured
- the patient has a severe chest injury (particularly multiple rib fractures and/or flail segments)
- the patient is to be transferred and there is a risk of severe deterioration en route.
The emergency induction of anaesthesia for the purpose of intubation and ventilation in a hypoxic patient is a difficult and demanding task. It requires considerable anaesthetic skills.
C – Circulation
Check for a Central Pulse (over 5 Seconds)
The absence of a central pulse (or a rate of <60 beats/min in infants) indicates the need to follow procedures for cardiorespiratory arrest:
Arrest rhythms:
Look for
- Pallor and coolness of the skin – the body diverts blood away from the skin when there are circulatory problems and these signs are thus very useful indicators of shock.
- Pallor and sweating – signs of gross sympathetic disturbance.
- Active bleeding or melaena
- A fast or slow heart rate – fast heart rates usually mean that either there is a cardiac arrhythmia or more commonly the sympathetic nervous system has detected a problem with the body (such as hypoxia, hypoglycaemia, pain or fear) and is ‘instructing’ the heart to beat faster. A slow heart rate usually means that something is wrong with the heart itself. The worst cause of this is severe hypoxia (or hypovolaemia) and, in this case, it means that terminal bradycardia and asystole are only seconds away.
- Abnormal systolic blood pressure
- A raised capillary refill time – it should be less than 2 s if the circulation is satisfactory. However, peripheral shutdown in a cold, wet patient can easily produce a prolonged refill time.
- Absent or quiet heart sounds and raised jugular venous pulse (JVP) – suggestive of tamponade if accompanied by hypotension and tachycardia; JVP will not be raised if there is also hypovolaemia.
- A precordial wound
- An abnormal electrocardiogram (ECG) trace on the monitor
- Signs of left ventricular failure (dyspnoea, gallop rhythm and crepitations)
- Signs of abdominal, pelvic or occult bleeding (may need per rectum examination and a nasogastric tube or ultrasound scan)
- Signs of dehydration (especially in children)
- Purpura (meningococcal septicaemia)
Inadequate circulation will reduce tissue oxygenation and thus may also cause:
- a raised respiratory rate
- altered mental status.
Cardiac Function
The stroke volume is the amount of blood ejected from the heart with each beat. It is determined by the left ventricular filling pressure, myocardial contractility and systemic vascular resistance. The product of heart rate and stroke volume is the cardiac output – the most important parameter of cardiac function. (Cardiac index is cardiac output divided by body surface area.) An increase in heart rate will directly increase the cardiac output and is the earliest cardiac response to hypoxia. However, the faster the heart beats the less time there is for it to fill and, eventually, a rise in heart rate will no longer be matched by a rise in cardiac output.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree