- Give high-concentration oxygen
- Give nebulised salbutamol for wheezing
- Estimate arterial blood gases and carboxyhaemoglobin
- Save blood for forensic tests
- Request a chest radiograph
- Admit for 24 h observation even if burns appear minimal.
Assessment of a Burn
Extent
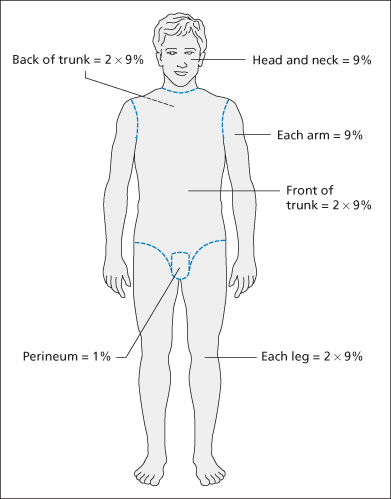
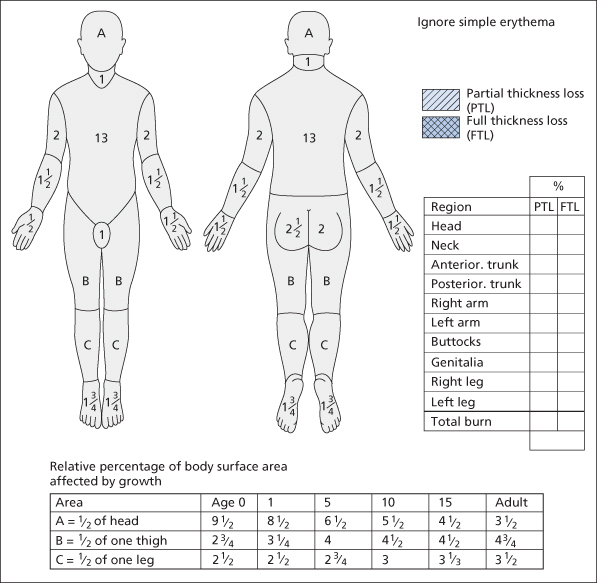
The extent of a burn is estimated by using the rule of nines in adults (→ Figure 10.1). In children, the Lund–Browder chart is used to take account of the relatively larger head and smaller legs (→ Figure 10.2). As a useful guide, the surface area of the patient’s own outstretched hand is around 1% (or more exactly 0.8%) of the total body surface area.
There is only a slight difference between the volume of fluid lost through partial-thickness and that lost through full-thickness burns, although the extent of erythrocyte destruction is greater in the latter.
Depth
The depth of a burn is a function of:
The circumstances leading to the cause of the burn may help. A motorbike exhaust pipe burning through a leather boot may only inflict a superficial burn. Someone with epilepsy or alcohol problems who falls into a fire will sustain deep burns. Elderly patients and those with peripheral neuropathy (e.g. people with diabetes) are at especial risk. Electrical burns are usually very deep.
Clothes closely applied to the skin, such as underwear, socks, belts and collars, tend to trap fluids and potentiate the severity of the burn locally.
Superficial burns expose intact nerve endings and are painful. Deep burns destroy nerve endings and are painless – testing the response to a pinprick may be helpful but is not always reliable. The skin often resembles thick, dry, cream-coloured parchment, unlike the red, angry skin of a superficial burn.
Treatment of Burns
Flooding with Cold Water
The damage inflicted by hot fluids may be diminished by flooding the affected part with cold water. Pain is simultaneously reduced. Immediate irrigation for up to 5 min may limit the extent of the burn, but beware of hypothermia, especially in small children.
Analgesia
Analgesia should be given early and always before transfer to another unit. It is usually under-prescribed. The beneficial effects of morphine in small children greatly outweigh any haemodynamic side effects, but it is essential to calculate the initial dose using the patient’s weight. Do not be afraid to give further doses as dictated by the state of the patient (→ p. 13).
Intravenous Fluids
If the burn involves more than 15% of the skin (10% in children and elderly people) or involves the face (making oral feeding difficult), an IV line must be set up. It will be required for a few days and must be reliable and easy to maintain. Reduced immunological competence increases the risk of infection after burns. An aseptic technique must be used.
The initial fluid should be Hartmann’s solution; later on, a colloid may be used. The choice includes synthetic sugars, gelatin and starch, albumin, plasma protein fraction and reconstituted plasma. Most departments use a gelatin solution initially but check the local burns unit’s preference. Whole blood will be required if there is a significant element of full-thickness skin loss.
 Box 10.1 Fluid Replacement for Burns
Box 10.1 Fluid Replacement for Burns- Intravenous fluids are required if more than a 15% surface burn (10% in those <10 or >70 years). Hartmann’s solution should be used. An initial 10–20 mL/kg can be given whilst awaiting formal calculations
- Isolated areas of erythema are not included in the calculation but cannot be ignored
- No distinction is made between areas of full- and partial-thickness loss at this stage
- Patients who have inhalational injuries in addition to skin burns initially require up to 40% more fluid
- Fluid to be given must be calculated from the time of the burn rather than the time of arrival at hospital
- The Parkland formula is used to calculate the amount of Hartmann’s solution required in the first 24 hours following the burn:
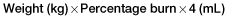
Half of this volume should be given during the first 8 hours and the remainder over the following 16 hours.
- An additional amount will be required to satisfy the patient’s normal fluid requirements (about 1500 mL/day for a 70-kg man). This will be raised if there is pyrexia
- Urinary output is the best way of monitoring fluid replacement. Plasma substitutes and blood will be required later on if there is a significant element of full-thickness burning
Definitive Care of Large Burns
Patients with large burns must not be kept in the ED for longer than it takes to:
- initiate resuscitation
- exclude, or treat, other major injuries
- establish monitoring and investigations
- agree a treatment plan with the local burns unit
- prepare for controlled transfer to the appropriate area.
The indications for admission are based on the extent and site of the burns:
- Burns >15% (>10% in children and elderly people) produce haemodynamic changes, which demand inpatient treatment.
- Burns to the perineum, around the mouth and to the airway will require specialised nursing care.
- Some small burns can be managed safely and effectively only if the patient is in hospital. These include circumferential limb burns and full-thickness loss around the eyes, nose and ears (these are discussed in the next section).
Local arrangements will influence whether admission is to a general surgical ward, an intensive care unit or a specialised burns unit. The last is often some distance from the ED and usually has a limited number of beds. It is inappropriate to refer very severely burned elderly patients to specialised (and often distant) burns units when it is clear that they will die.
Before transfer check the following:
- The airway control is immaculate, and unlikely to deteriorate.
- IV access is adequate and cannula fixed well in place.
- Fluid regimen is agreed and running.
- Monitoring equipment is suitable.
- Charts, notes and laboratory results are with the patient.
- Analgesia is satisfactory and can be topped up.
- Level of nursing/medical care required en route has been considered.
SMALL BURNS
Most burns under 10% of the body surface area can be managed on an outpatient basis. Exceptions are discussed under Special burns → p. 142.
Initial Assessment and Management
Initial action includes:
- the removal of the source of the burn
- flooding with cold water
- analgesia
- assessment of size, site and depth (a drawing is useful) → p. 137.
A temporary dressing, without medication, is applied once the burn area has been exposed and the patient is waiting for definitive care. Analgesia must be given as soon as possible, especially to children.
The pattern of burning should be considered in the light of the history available. A scald from spilt water will produce a cascade effect, with streaks of burnt skin following the path of the falling fluid, possibly with increasing depth of injury where its flow has been held up by constricting clothes such as waistbands or socks. A scald with a glove or stocking distribution is unusual; either the patient has impaired peripheral or central pain perception or the limb was held under water. In children, this type of appearance suggests abuse (→ Box 10.2 and p. 353).
 Box 10.2 Features of a Burn That Suggest Non-Accidental Injury
Box 10.2 Features of a Burn That Suggest Non-Accidental Injury- Glove or stocking distribution, especially if bilateral
- Involvement of buttocks or perineum
- Scalds with a clearly demarcated edge with no peripheral splash marks
- Small, even, rounded (cigarette tip) burns
- General features of history and presentation suspicious of abuse
The depth of the burn influences long-term treatment and should be determined as soon as possible. Superficial erythema is initially painful whereas full-thickness burns will be insensitive because the nerve endings have been destroyed. Most areas of most burns fall between these extremes and are termed partial-thickness burns.
If most of the dermal papillae and all of the skin appendages (hair follicles and sweat glands) are intact, there is a very good potential for spontaneous regeneration. The term ‘deep dermal’ is used to describe partial-thickness burns with only a few epidermal remnants remaining – usually around the necks of sweat glands and hair follicles. If the wound becomes infected, these cells may die, resulting in full-thickness skin loss. Prevention of infection is thus of paramount importance in deep dermal burns.
There is frequently a combination of partial- and full-thickness burning. The patient may consider the whole area sensitive and it is often difficult to determine depth at the first examination. However, the distinction is usually unimportant in the very early stages of treatment. Most areas of full-thickness loss that require grafts are evident by 5–10 days. Electrical burns may be suitable for the specialised technique of immediate excision and grafting.
Dressing and Follow-Up of Simple Superficial Burns
Skin debris and foreign material are removed with dilute antiseptic and cotton-wool balls.
A sterile, non-adherent dressing is then applied. Antiseptic substances are not needed for most burns but are often used (e.g. silver sulfadiazine or mupirocin cream). Healing will occur more rapidly in a moist environment, but excess exudate should be kept away from the wound surface. A moist wound surface reduces damage to the new epithelium when the dressing is changed and is less painful. Specialised dressings are available that retain excess exudate and allow gas exchange but they are expensive. Technique and experience are as important as dressing material.
The wound dressing is covered with a more robust gauze for added protection. Limb burns should be elevated, but the patient encouraged to move the burned part as much as possible. Stiffness will develop quickly and is slow to resolve once established. Routine prophylaxis with antibiotics is not indicated.
The burn should be reassessed within 36–48 h. Dressings should be changed no more than three times in the first week and less frequently thereafter. Most patients can be taught to dress small burns at home. Elderly patients can be treated at home by the district nurse or at the local health centre. All burns to special areas and full-thickness burns should be reviewed in the ED.
Once the wound has fully epithelialised, and has thus become dry, it should be exposed to a clean environment but protected from dirt and friction by temporary dry dressings. A moisturising cream can be applied to replace the sweat gland secretions, which are often deficient for some months after burning. The patient should be warned that the skin will be especially sensitive to ultraviolet light throughout the following summer.
Skin Grafting of Burns
Some electrical burns are most effectively treated by initial excision and early grafting and are best referred immediately to a burns unit. However, most small, simple burns treated on an outpatient basis in an ED should be managed conservatively for at least the first 5 days.
Wounds under 2 cm in diameter usually contract and close spontaneously, even if there is full-thickness skin loss. Larger wounds will show evidence of marginal and focal epithelialisation. It should be possible to distinguish deep-dermal from full-thickness burns within 10 days of the injury. If the former remain sterile, thereby avoiding destruction of the epithelial remnants, they will heal spontaneously. The latter will require split-skin grafts. The technique is described on p. 395.
SPECIAL BURNS
Burns to the Face
Inhalation burns must be excluded (→ p. 136). The patient may have deceptively good function when first assessed but can deteriorate over 24 h. Swelling is a major problem:
- Patients with burns to the eyelids and cornea must be admitted to a specialised eye unit. Lid retraction may cause major problems. Apply an antibiotic (e.g. chloramphenicol) eye ointment before transfer.
- Burns around the mouth cause feeding problems. Inpatient care is usually required. The burns unit should be contacted for advice.
- Deep burns involving the nose and ear may destroy underlying cartilage and should always be referred for specialised care.
- Partial-thickness burns of other areas of the face can be adequately treated on an outpatient basis. Silver sulfadiazine cream is applied very sparingly and repeated by the patient at home, once or twice per day. The area may blacken and be unsightly, but this is not harmful. No other dressing is required. Chloramphenicol ointment should be prescribed if the burns have encroached on the periorbital area.
Burns to the Hands
The fingers quickly stiffen up and conventional bandages become very dirty, with an increased risk of infection. These complications are avoided if plastic gloves are used initially instead of standard dressings. Silver sulfadiazine cream is applied and a loosely fitting examination glove is fitted in place with tape around the wrist. The gloves tend to burst, so patients must be given a supply to apply by themselves.
Patients are encouraged to move the hand as much as possible. The skin becomes macerated and the exudate and silver sulfadiazine produce an aesthetically unpleasant sight. Coloured gloves overcome some of the patient’s understandable anxieties but reassurance should be given that the maceration will resolve rapidly once the glove is removed.
Burns to the Perineum
The perineum must be examined carefully. It is a common site for non-accidental burns. Any burns to the top of the thighs or on the buttocks, which cannot be adequately dressed, and all those nearer the perineum, which cannot easily be kept clean, must be managed in hospital. A short-stay ward may be appropriate, but extensive or full-thickness burns should be referred to the burns unit.
Circumferential Burns
If a partial- or full-thickness burn extends completely around a limb the distal circulation may become impaired. Minor degrees of venous obstruction can be treated by admission and elevation. Deep burns, which will quickly contract, may cause more serious obstruction. Similar complications may occur on the trunk causing respiratory distress. Escharotomy may be required. This is associated with significant fluid loss and must not be undertaken without expert advice.
Chemical Burns
Acidic solutions produce painful coagulation burns, which are often self-limiting and superficial with destruction of the surface epithelium and submucosa only. Concentrated and corrosive acids such as phenol and hydrofluoric acid (→ p. 143) may cause deep burns with systemic absorption. Alkaline solutions produce deep, full-thickness liquefaction burns that can be surprisingly pain free at first. However, there is extensive damage that is due to solubilisation of proteins such as collagen, saponification of lipids and dehydration of tissue cells.
TX
No attempt should be made to neutralise chemicals on the skin (except hydrofluoric acid → p. 143). Most neutralising reactions are exothermic and would cause an additional thermal injury. Dilution by continuous irrigation with water for at least 10–15 min (or until the pH of the burned area is normal) is the mainstay of treatment. Prolonged irrigation with cold water also reduces pain significantly. Caution must be exercised with young children who quickly become hypothermic. Systemic absorption of some chemicals (e.g. phenol) may be significant. Toxicological advice should be sought.
Hydrofluoric acid Burns
Hydrofluoric acid (hydrogen fluoride) is used extensively in industry and horticulture. Skin contact causes severe local tissue damage with a great deal of pain. The burn is deep and slow to heal. With solutions containing less than 50% hydrofluoric acid there may be a delay until the burn develops as follows:
- Anhydrous or >50% concentrations – immediate damage
- 20–50% concentrations – up to 8 h delay
- <20% concentrations – up to 24 h delay.
Even concentrations of acid as low as 2% may cause burns after prolonged skin contact.
Investigations:
Significant absorption of fluoride ion through the skin may cause hypocalcaemia. Cardiac arrest may occur in the extensively burned patient. The serum calcium should be checked in all patients with larger burns resulting from contact with hydrogen fluoride.
TX
Immediate irrigation of the contaminated area is essential and may be very effective. Pain, tissue destruction and hypocalcaemia can be reduced by converting the acid to its calcium salt. This is achieved by repeated application of calcium gluconate gel (marketed as hydrofluoric acid burn jelly). There is no exothermic reaction. The injection of 10% calcium gluconate around and under the burn is sometimes advocated for persistent pain in well-localised lesions.
White Phosphorus Burns
White (or yellow) phosphorus is commonly used in incendiary devices and so may cause severe burns. Exposure to phosphorus can lead to hypokalaemia, hypocalcaemia and hypophosphataemia. In addition, toxic phosphorus pentoxide gas can be released, which is irritant to the lungs.
TX
Injuries and burns that are contaminated with white phosphorus require special and unique management:
- The burned area should be lavaged copiously to remove identifiable particles (which should be placed in water to prevent spontaneous combustion). A Woods lamp (in a darkened room) may help to identify phosphorus particles. The burned area must be kept covered with saline-soaked gauze to prevent further combustion.
- Definitive treatment consists of a rinse using 1% copper sulphate (CuSO4) solution to aid removal of the particles of phosphorus. Copper sulphate combines with phosphorous to create a blue–black cupric phosphide coating. This impedes further combustion and makes phosphorus particles easier to find. The burn is irrigated with copper sulphate solution, particles are removed and then the copper sulphate is lavaged away with saline. Excess copper sulphate absorption can cause intravascular haemolysis and renal failure.
Chemical Burns from Giant Hogweed
The plant Heracleum mantegazzianum – better known as giant hogweed – is a public health hazard and an environmental nuisance. In addition to its toxicity, this aggressive foreign invader prevents native plant species from growing and increases soil erosion. Under the Wildlife and Countryside Act 1981 and the Wildlife (Northern Ireland) Order 1985, it is an offence to ‘plant or otherwise cause giant hogweed to grow’. Despite this, the species is common in the British Isles and is found alongside roads, railway lines, rivers and footpaths, often in areas of wasteland. The plant is characterised by its size. Over a period of 4 years, it may grow up to 5 m in height and looks rather like an overgrown cow parsley. It has a reddish-purple stem and spotted leaf stalks with fine spines that make it appear furry. The leaves may be up to 1.5 m in width with large flowering heads. These characteristics make the giant hogweed plant irresistible to children who make swords and umbrellas from it.
Unfortunately, giant hogweed exudes a clear watery sap from its leaves and also from the stem in even greater quantities. This sap contains a glucoside called furanocoumarin, which renders the skin photosensitive to ultraviolet (UV) light. Exposure to sunlight after contact with the sap results in large painful blisters, burns and linear inflammation. This reaction usually appears within 15–20 h of contact although it can occur up to 48 h later. Damaged skin heals very slowly over at least 2 weeks, leaving residual pigmentation that can develop into chronic phytophotodermatitis. Inflammation may recur in sunlight for many months.
TX
In the event of contact with giant hogweed sap, the skin should be washed immediately with soap and water and then covered to reduce the exposure to sunlight. Application of topical steroids, if started early in the inflammatory process, can reduce the severity of the developing burns. Otherwise, partial-thickness lesions are treated with dressings and analgesia until healing occurs. Advice about subsequent UV light exposure should be given to all patients.
Burns from Hot Tar
Hot bitumen solidifies on contact with the skin. Water should be applied at the site to hasten hardening and limit heat transfer. Bitumen on blistering skin should be removed with the blister. Adherent bitumen should be left in place and covered with paraffin gauze. This will help to dissolve and separate it. Earlier excision would inflict more damage.
Sunburn
Unprotected exposure to UV radiation can cause extremely painful, blistering, oedematous skin. In general, the treatment is as for any other burn. However, the pain of the intense erythema that so often results can be greatly alleviated by the regular application of 1% hydrocortisone cream.
ELECTROCUTION
High-Voltage Injury (Including Lightning)
Injuries following a high-voltage electric shock may result from the following:
- Falling or being thrown to the ground, causing secondary injuries
- Tetanic muscle contraction, causing fractures of long bones, crushed vertebrae, torn muscles
- Spontaneous ignition of clothing, causing burns
- Conduction of electricity through the body, causing entry and exit wounds and internal injuries
- Current passing along the surface of the body to earth, causing very deep burns over a large area of skin
- Current jumping from one part of the body to another, causing secondary exit and entry wounds.
The patient may have a respiratory or cardiac arrest. If this is successfully reversed or if the patient presents without having had a life-threatening cardiac dysrhythmia, it is unlikely that one will develop subsequently. Supraventricular tachycardia has been reported, but more commonly the ECG shows right bundle-branch block and/or ST changes. These may last many weeks. Treatment is based on symptoms and clinical signs in the normal way. Cardiac markers will be raised irrespective of cardiac damage and so their measurement is not helpful.
If the current travels through the body, it naturally follows the path of least resistance. Nerves and blood vessels are good conductors. Increasing resistance is offered by muscle, skin, tendon, fat and bone in that order. Structures with high resistance will generate the greatest heat but, clearly, some tissues are more readily damaged by heat than others. Nerves, blood vessels, muscles and skin sustain most of the injury.
The entry point is typically charred and depressed. It becomes swollen very quickly, with the accumulation of extracellular fluid. The exit point has an explosive appearance – round or oval grey craters with no inflammatory changes. These increase in size over the first few days.
In the peripheral nerves, axons are distorted and Schwann cells break down and coalesce. Spinal cord lesions are surprisingly common, often producing partial transections. Brain damage is unusual unless the head has been directly involved.
Blood vessels sustain endothelial damage and media degeneration. Thrombosis and late rupture can occur at sites distant from the entry point. Visceral lesions, which are often unrecognised, probably have a vascular aetiology.
Muscle involvement is typically patchy, with swelling, necrosis and the later development of deep sepsis.
Acute tubular necrosis is common. Inadequate volume replacement, myoglobinuria and direct damage to renal vessels probably all contribute to its development.
Cataracts are a well-recognised, late complication.
Late death is commonly caused by overwhelming sepsis. However, there is only a one in several million chance of being killed by lightning in the UK!
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree