PEDIATRICS
Knowing a child’s age is important to determine normal vital signs, disease prevalence, and the appropriate medications. It is also an indicator of social milestones. The easiest way to determine a child’s age is to ask the parent or check available records. However, in cultures where birth records are unavailable, as well as during acute out-of-hospital or emergency department (ED) events, this information may not be easy to get.
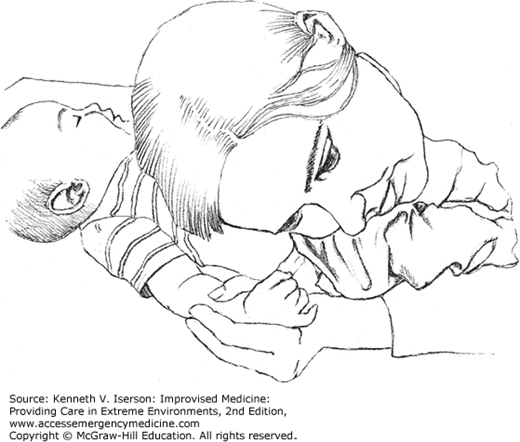
Without records, one way to estimate a child’s approximate age is to count the number of teeth present and then add six to derive the age in months.1 Another way is to have the child sit upright (with the head in a neutral position), then raise one arm over his head and try to touch the opposite ear (Fig. 7-1). This “overhead test” has a sensitivity of 90% and a specificity of 78% (positive predictive value 93%, negative predictive value 68%). If the child successfully performs this test, he is most likely ≥6 years old, which is the age to begin school and to receive other benefits in many cultures. If a child fails this test, there is a good chance that he is <6 years old, but it is less clear, because other factors, such as malnutrition, may influence the results. The test works because a 6-year-old child’s humerus is long enough to raise the elbow so that the forearm extends across the head and allows the fingers to reach the opposite ear.2
Any firm surface can be marked in 1-cm (or 0.5-inch) increments to measure a patient’s height. For ambulatory patients, use a vertical surface, such as a wall or the side of a doorway. For infants, children, and bedridden patients, mark the side rails of stretchers and beds with indelible ink. Once a child’s height is known, the weight can be estimated.
Correct weight estimates are crucial in determining pediatric medication and fluid doses. When asked, the parents of children aged from 1 to 11 years old can estimate their child’s weight within 10% of the measured weight only 78% of the time. All other forms of guessing a child’s weight, including the Argyll, the Advanced Pediatric Life Support (APLS), and the Best Guess methods, perform poorly.3 If the parents aren’t available, use the following formula for children 1 to 13 years old:
This formula underestimates weight by about 7%, as opposed to > 33% for the APLS formula.4
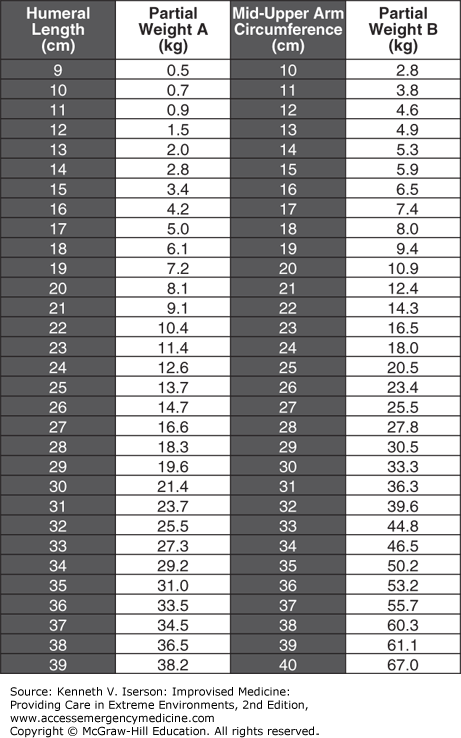
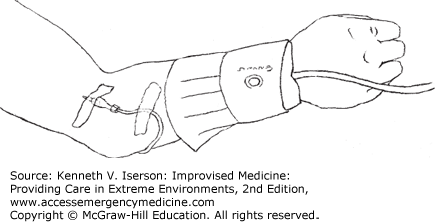
Although many clinicians still use the Broselow tape, it is inaccurate in most children >10 years old, falls within 10% of the measured weight only 61% of the time, and is less accurate with older children.5,6,7,8,9 A much better method is to use the Mercy TAPE (Fig. 7-2), which integrates mid-arm circumference (MAC) and humeral length (HL), a surrogate of height, to dramatically improve its predictive performance.10 The Mercy TAPE works well with children not only in developed countries, but also has been shown to be accurate in India and Mali.11
FIG. 7-2.
Mercy TAPE. Add “partial weight A” and “partial weight B” to get the child’s weight. (Reproduced with permission from Abdel-Rahman and Ridge.13)
In children, measure the MAC at the midpoint of the humerus with the arm hanging down at the child’s side. Measure the HL from the upper edge of the posterior border of the acromion process to the tip of the olecranon process. Record the measurements to the nearest millimeter.12
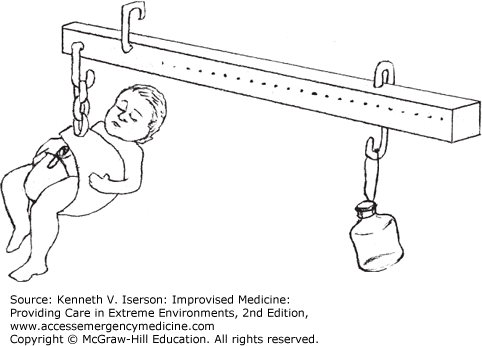
When standard scales to weigh infants are not available, make a beam scale (Fig. 7-3). If finely calibrated, the beam scale may also be used to weigh smaller items, such as medications.
To make a beam scale, use a straight, rigid pole of bamboo, metal, or dry wood, ~1 m long. Mount a hook close to one end from which the beam will be suspended. Put another hook about 5 cm away, between the first hook and the nearest end of the beam. This is where the infant or substance to be weighed is suspended. A fixed weight is also suspended from the beam, but on a moveable slide (e.g., metal wire). The weight can be a bag, bottle, or other container filled with sand. Mark gradations on the beam for each weight increment. Use standard weights to calibrate the scale initially, so the gradations are accurate. Hang the known weight at the end of the scale (i.e., where the infant would be) and mark the point on the beam where the sliding weight is when the scale balances evenly.14 Large increments (1 L of water weighs 2.2 kg, 0.5 L weighs 1.1 kg, etc.) and smaller increments (use the weight of a common coin and its multiples) can be easily determined. If a local merchant (jeweler, grain dealer, etc.) has standard weights, try to borrow them for more accurate calibration of the scale.
ADULTS
If an adult’s height can be measured only in a sitting position, such as with a wheelchair-dependent patient, measure each arm span in centimeters, from midsternum to the end of the extended middle finger (half-arm span). Use the longer of these measurements in the following formula: Height ≅ (0.73 × [2 × half-arm span]) + 43 cm.15 A simpler method is to double the longest measurement from midsternum to the tip of the patient’s long finger.16
Patient-reported height is the best bedside method to estimate true height and can be used to calculate ideal body weight (IBW). Physician and nurse estimates of true height are substantially less accurate, as is true height obtained from a regression formula that uses measured tibial length.17
A patient’s own weight estimate is the most accurate method to approximate true actual body weight. Clinicians’ bedside estimate of a patient’s weight is unacceptably low, and the conventional 70-kg/60-kg male/female IBW standard misclassifies most patients by 5 kg, and many by 10 kg. The following method is a good way to estimate adults’ actual body weights. These formulas can be preprogrammed in a computer for easier use.18
Knee height: The distance between the thigh prominence with the knee bent at 90 degrees proximally and the plantar aspect of the foot at the heel with the ankle bent at 90 degrees distally.
MAC: In adults, palpate the humeral head proximally and the lateral humeral condyle distally. Wrap a tape measure around the arm midway between these landmarks so that it contacts the skin at all points but does not compress the soft tissue.
Use the actual weight to determine the patient’s body mass index (BMI), which correlates with nutritional status. The formula to calculate BMI is body weight (kg) divided by [height (m) squared], or [kg ÷ m2].15 In adults, a BMI ≥18.5 is normal; BMI <16 is severe malnutrition.19
Knowledge of a patient’s ideal body weight (IBW) can be important for drug dosing and for calculating ventilator volume settings. It can be calculated from the patient’s height using the Devine formula, which is most applicable for people ≥60 inches (152 cm) tall17:
IBW for men (kg) = 50 + [2.3 × (height in inches – 60)]
IBW for women (kg) = 45.5 + [2.3 × (height in inches – 60)]
MEASURING TEMPERATURE WITHOUT A THERMOMETER
In austere circumstances, a thermometer normally is not available. Generally, caregivers notice a tactile fever in only about half of all children with a measurable fever. Elevated tactile temperatures, as measured at home by mothers touching their child’s forehead, have moderate (46%–73%) correlation with fevers recorded in the ED or hospital.20,21 However, for children >2 years old with a temperature ≥38.9°C (102°F), tactile assessment can determine that a child has a fever 98% of the time.20
If you do have a thermometer and you need to convert the numbers from Celsius (Centigrade; C) to Fahrenheit (F) or vice versa, use these formulas:
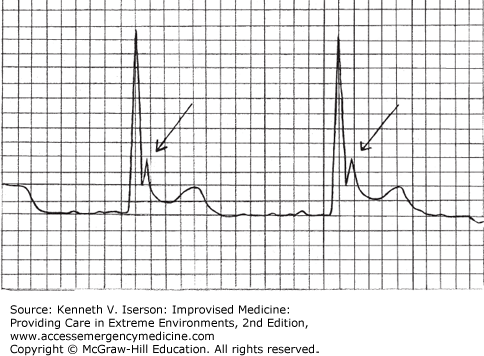
An Osborn or J wave on an electrocardiogram (ECG) can suggest hypothermia, especially in elderly patients in whom the diagnosis is not suspected. This elevation at the QRS-ST junction (Fig. 7-4) occurs in about 80% of hypothermic patients (a core body temperature ≤95°F [35°C]) and in nearly all patients whose temperature is <90°F (32.2°C). The waves’ sizes appear to be inversely related to temperature, but otherwise they do not appear to have any prognostic value.22
PULSE AND RESPIRATIONS
To time pulse or respiration measurements without a watch, clock, or other timepiece, you must either count the pulse beats or respirations yourself or make a timer.
Counting is not as accurate as using a watch, but time may be measured by counting in any situation: Simply count “one-thousand-one, one-thousand-two,” and so on, while someone else counts the pulse. To calculate pulse rate per minute, count to “one-thousand-six” (about 6 seconds), then multiply the counted pulsations by 10. Simply estimating time without counting always results in underestimation.
To make a simple, portable sand timer, use a blood collection tube or other piece of glass that can be molded when heated. Heat the middle of the tube and stretch to narrow the diameter. Then, if both ends of the tube are open, seal one end by heating it over a flame. Next, sift some sand through a fine strainer. Dry the sifted sand completely by using sunlight or an oven. Stand the tube upright and put enough sand in the top part so that the sand takes 1 minute to run from the top, through the narrow middle, to the bottom section (Fig. 7-5). During construction, you will need a watch, a clock, or a previously calibrated timer to check the initial timing. After the correct amount of sand is in the tube, seal the open end either by heating or with a stopper. Because these tubes break easily, store the timer in a padded box.
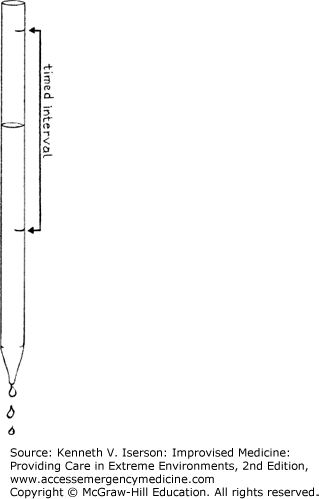
Water timers also work well. Heat the end of a long, narrow glass tube. Stretch that end and break it, leaving a very tiny opening. A micropipette with a very tiny opening may also suffice without the need to work with heated glass. In either case, make a narrow mark near the top (near the wide opening) of the tube with nail polish, tape, or another marker, or by etching the glass. Cover the narrow end of the tube and fill the tube with water exactly to the level of the mark. Let the water drip out of the tube for 1 minute. Mark the tube again at the exact water level after 1 minute (Fig. 7-6). Voilà, you have a timer!
Finally, if you have no clock or wristwatch for measuring pulse and respirations, use the clock or timer function on the now ubiquitous (even in the least-developed regions of the world) cell phones—if it has a second hand—or download a free stopwatch app.
When you cannot palpate a pulse at the typical wrist or femoral areas, try one of these sites:
Carotid artery: Slide your fingers from the midline to the opposite side of the neck from where you are standing and stop at the anterior border of the sternocleidomastoid muscle. The carotid should be palpable. Do not press too hard and cause a vagal response.
Superficial temporal artery: This is accessible in nearly all patients. Put two fingers just anterior to the ear at the superior part of the tragus. The finger most proximal to the ear will normally feel the pulsation without difficulty.
Dorsalis pedis and posterior tibial (foot/ankle) arteries: These are often used to check for peripheral vascular integrity, and also to monitor the pulse, especially when the other sites are inaccessible. These arteries can also be used when drawing arterial blood gasses; it is much easier and safer to draw from these arteries than, for example, from the femoral arteries.
Palpating an infant’s pulse, especially when they are critically ill and a decision must be made immediately about whether to begin resuscitation, can be very difficult. The easiest, fastest, and most successful method of determining infant cardiac activity can be applied in any situation, because it requires no equipment. It does not even require finding and palpating a pulse: Simply place your ear against the infant’s chest wall and listen for heart sounds—direct auscultation (Fig. 7-7).
A study with experienced pediatric nurses trying to find a pulse in infants showed that the mean time to correctly identify the pulse rate using direct auscultation was 2.4 ± 1.2 seconds, with a 100% success rate. Palpation methods took longer and were less successful. The frequently used femoral pulse rate took 9.1 ± 5.9 seconds to find, with only a 43% success rate.23
A weak radial pulse in most trauma patients (at least those 18-50 years old without a head injury) indicates a markedly increased mortality (29%) compared to only 3% of those with a normal pulse (odds ratio: 15.2). There is also a strong likelihood that these patients will require intubation (odds ratio: 7.5) and admission to the intensive care unit (ICU) (odds ratio: 5.3). Patients with an absent radial pulse are usually dead or soon will be dead.24 In addition, tachycardia is a much more reliable sign of hypovolemia than is blood pressure (BP).
BLOOD PRESSURE
“The ability to obtain a blood pressure measurement in an austere environment is often limited by time constraints, equipment availability, and noisy conditions.”24
Estimating BP from a palpable pulse, for example, radial (>80 mm Hg), femoral (70-80 mm Hg), or carotid (60-70 mm Hg), overestimates the patient’s actual BP.25
A useful finding is that patients with palpably cool extremities as compared with those of other patients have hypoperfusion. Especially when found in an arm and a leg, such patients have low cardiac indices, low pH, low bicarbonate levels, low mixed venous oxygen saturation (SvO2), and elevated lactate levels.26
When transporting patients by air or in a noisy ambulance, Korotkoff sounds (BP) may not be audible through a stethoscope. When a stethoscope is not readily available or cannot be used, palpate the systolic pressure. If done carefully, this method is as accurate as using a stethoscope.
If a pulse oximeter is available, it also can be used to measure the systolic BP when there is too much noise or vibration either to use a stethoscope or to palpate a pulse. Place the sensor on a finger, get a good waveform, inflate the sphygmomanometer until the waveform disappears, and then slowly deflate the cuff until the waveform reappears. This measurement is an accurate measure of the systolic pressure.27
Neonatal arm BP cuffs can be used successfully on adult forefingers, producing a “finger cuff.” Only the mean BP equates to that taken on the arm.28 If a manometer is available, some disposable (or non-disposable) pressure pumps for intravenous (IV) fluids and blood can be used as (a) a BP cuff if attached to a manometer or (b) an extremity tourniquet (clamp the tube when inflated). In large adults, these devices may only fit on their calf or forearm.
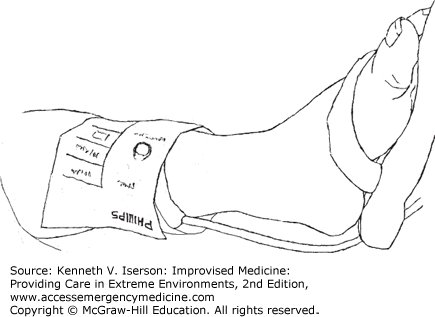
Blood pressure cuffs placed on the forearm (Fig. 7-8) and above the ankle (Fig. 7-9) deliver the same or nearly the same BP as when placed at the brachial artery (arm). Forearm or ankle measurement comes in handy with obese patients on whom the standard adult cuff is too small, for adults when only a child-sized cuff is available, or to avoid compressing an area with trauma. In addition, use a forearm or ankle BP to avoid periodically occluding an arteriovenous fistula (in dialysis patients) or an IV line. The mean and diastolic pressure readings are essentially equal in the arm and the ankle, but the systolic pressures are not. So, use the mean BP with a calf BP cuff. (Calculate this by multiplying the diastolic pressure by two and adding the systolic pressure. Then divide the result by three. Alternatively, take one-third of the difference between the systolic and diastolic pressures and add it to the diastolic pressure.)
This difference between the calf and the arm BP readings is reflected in the normal ankle–brachial index (ABI), used to test for vascular compromise in the leg. The calf’s systolic pressure is normally higher than that in the arm. To calculate ABI, divide the systolic pressure in the leg by that in the arm. Use a Doppler for accuracy. In the supine patient, the normal result is generally 0.9 to 1.2.
To prevent an IV from backing up and possibly contaminating the IV solution when the BP cuff inflates on the same extremity, run the IV tubing under the cuff, so that when it inflates, the IV stops. When the cuff deflates, the IV starts flowing again.29
Falsely high BP measurements result in patients taking unnecessary and potentially harmful medication. The following factors can result in inaccurate BP readings30:
| If the: | BP can be falsely elevated by: |
|---|---|
| 1. Patient has a full bladder. | 10-15 mm Hg |
| 2. Patient’s back is unsupported. | 5-10 mm Hg |
| 3. Patient’s feet are unsupported. | 5-10 mm Hg |
| 4. Patient’s legs are crossed. | 3-8 mm Hg |
| 5. Sphygmomanometer cuff is over clothing. | 10-40 mm Hg |
| 6. Patient’s arm is unsupported. | 10 mm Hg |
| 7. Patient is talking or has not had at least 3 minutes of quiet time prior to the measurement. | 10-15 mm Hg |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree