116 Urinary Tract Obstruction
Several definitions may be encountered when considering urinary tract obstruction:
 Epidemiology
Epidemiology
Urinary tract obstruction is a common disorder. On autopsy, 3.1% of adults have hydronephrosis.1 Data from the Healthcare Cost and Utilization Project’s National Inpatient Sample (based on ICD-9 codes) indicate that 1.75% of all hospital discharges are complicated by either hydronephrosis or obstruction.2 When hydronephrosis is excluded, urinary tract obstruction occurs in approximately 1% of hospital discharges.2 Urinary tract obstruction accounts for approximately 10% of community-acquired acute kidney failure3–5 and is a factor in 2.6% of acute kidney failure cases in the intensive care setting.6
 Etiology
Etiology
Congential Causes
Congenital UPJO is usually due to disease intrinsic to the urinary tract. Often an adynamic segment of ureter results in failure of peristalsis at the ureteropelvic junction (UPJ).7 Ureteral kinks or valves are another intrinsic cause of UPJO. Potential extrinsic causes of UPJO include abnormal rotation of the kidney during development, leading to ureteral compression and entrapment of the ureter by blood vessels, although significant controversy exists regarding the latter.7,8
Upper Urinary Tract Obstruction
Intrinsic Causes
Intraluminal Causes
Obstruction at the level of the renal tubules may be due to crystal-induced disease, uric acid nephropathy (as in the tumor lysis syndrome), or cast nephropathy due to multiple myeloma. Crystal-induced nephropathy has been classically described with sulfadiazine, acyclovir, indinavir, triamterene, and methotrexate.9 Newer literature also implicates orlistat10 and ciprofloxacin.11
Nephrolithiasis is a common cause of upper urinary tract obstruction at the level of the ureter, with the size of the stone determining the likelihood of obstruction. Stones ≤2 mm, 3 mm, 4 to 6 mm and larger than 6 mm will pass spontaneously 97%, 86%, 50%, and 1% of the time, respectively.12 Typically the obstruction occurs at one of the three narrowest portions of the ureter: the UPJ, the ureterovesicular junction (UVJ), or at the point where the ureter crosses over the pelvic brim. The obstruction is usually, but not always, acute and symptomatic. Neoplasms, blood clots, and sloughed renal papillae are rarer causes of intrinsic obstruction at the level of the ureter.
The causes of intraluminal obstruction at the level of the bladder are similar to those affecting the ureter, with urolithiasis, blood clots, and neoplasms being most common. Worldwide, infection with Schistosoma hematobium with resulting fibrosis is a common cause of bladder obstruction.13 Although rare in industrialized nations, it should be suspected in patients from endemic areas such as Africa and the Middle East.
Intramural Causes
Obstruction due to intramural causes is most often seen in the lower urinary tract. Disorders affecting the neuromuscular control of bladder emptying, such as cerebrovascular accidents,14 spinal cord injury,15 multiple sclerosis,16 and diabetic neuropathy17 may lead to bladder outlet obstruction. Multiple medications, including anticholinergics, opioid analgesics, nonsteroidal antiinflammatory agents, α-adrenoreceptor antagonists, benzodiazepines, and calcium channel blockers have also been associated with urinary retention.18 Stricture of the urethra may also lead to obstruction.
Extrinsic Compression
Pregnancy is typically associated with right-sided dilation of the renal pelvis, calyx, and ureter. Hormonal mechanisms and mechanical compression from an enlarging uterus and an enlarging ovarian vein plexus have been implicated in these changes.19 Clinically meaningful obstruction from the gravid uterus is extremely rare.
Malignancies may cause obstruction by several different mechanisms. Local ureteric compression may be seen in metastatic cancers of the cervix, bladder and prostate, as well as with expanding retroperitoneal soft-tissue masses. Alternatively, the ureters may be compressed or encased by metastatic retroperitoneal lymphadenopathy from a distant primary.20
Retroperitoneal fibrosis may lead to obstruction of one or both ureters via inflammation. It is an uncommon disorder, with a reported incidence rate of 1.3 case per million population and a male/female ratio of 3.3 : 1.21 Although the majority of these cases are idiopathic (>75%),22 numerous conditions are suspected to cause retroperitoneal fibrosis, including malignancies, medications, infection, trauma, or radiation.23 Treatment of idiopathic retroperitoneal fibrosis is initially with steroids, but recurrences are common. Case reports describe the use of cyclophosphamide, azathioprine, colchicine, mycophenolate, or tamoxifen for treatment relapses or steroid-resistant disease, although conclusive data are absent.22 Abdominal aortic aneurysms (AAA) may also cause obstruction due to compression of the ureter or via inflammation. A recent series evaluated 999 cases of inflammatory AAA and found preoperative hydronephrosis in 7.4%.24
The etiology of urinary tract obstruction is summarized in Box 116-1.
 Clinical Presentation
Clinical Presentation
Pain
Acute ureteral obstruction often presents with severe flank pain, otherwise known as renal colic. This is usually due to urolithiasis but may be due to other causes of ureteral obstruction (see earlier). Obstruction causes increased intraluminal pressure and spasm of the ureteral muscles, which are responsible for the colicky pain.25 Partial ureteral obstruction may present with a chronic dull pain. Bladder outlet obstruction may lead to distention and subsequent abdominal discomfort.
Lower Urinary Tract Symptoms
Obstruction of the lower urinary tract often presents with some or all of a predictable constellation of symptoms known collectively as lower urinary tract symptoms, or LUTS. LUTS include voiding symptoms (difficulty urinating, incomplete emptying), postmicturition symptoms (post-void dribbling), and storage symptoms (urgency, frequency, hesitancy, incontinence).26 Alternatively, patients with lower urinary tract obstruction may be asymptomatic.
Infection
The urinary retention associated with lower urinary tract obstruction provides an excellent culture medium for bacteria. Patients may present with cystitis, pyelonephritis, or sepsis. An obstructing renal stone may also be a nidus for infection. Recurrent infection should raise suspicion for possible anatomic abnormalities, especially in men. In one study, 25 out of 83 men (30%) with a febrile urinary tract infection (UTI) had anatomic lesions in the lower urinary tract, supporting imaging of the lower tract in men with this presentation.27 More recent data refute this finding in men younger than 45 years old.28
 Imaging in Urinary Tract Obstruction
Imaging in Urinary Tract Obstruction
Plain Abdominal Radiography
Abdominal radiography (kidney, ureter, and bladder [KUB]) is often the first imaging modality preformed in patients with acute flank pain. Although most stones are composed of calcium and should in theory be visible, only 59% of stones are detected on plain film.29 Compared to CT scanning, the sensitivity and specificity of abdominal films were 45% to 59% and 77%, respectively.29 Further, plain films may not always be able to differentiate phleboliths from calculi. This limits the utility of plain abdominal films to the diagnosis of recurrent disease in those with known radioopaque stones.
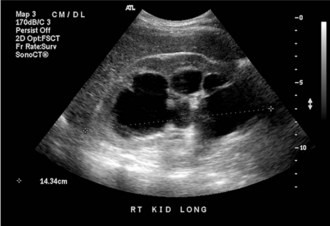
Ultrasound
Ultrasound (US) is inexpensive, does not expose the patient to radiation, and is typically readily available. Its accuracy in detecting hydronephrosis makes US a good screening tool for obstruction in the patient with unexplained kidney failure, or the patient with suspected lower urinary tract obstruction (Figure 116-1). US has been largely superseded by noncontrast CT in the detection of nephrolithiasis and stone-related obstruction. When CT is used as a reference, US has a sensitivity of 24% and a specificity of 90% for the detection of kidney stones and is likely to miss those less than 3 mm.30 Another disadvantage of US compared to CT is that bowel gas may obscure visualization of the ureters.31 Thus despite its ability to detect hydronephrosis, US may be limited in its ability to demonstrate the cause or site of an obstruction. Other conditions such as peripelvic cysts and renal artery aneurysms may mimic hydronephrosis on US.31 These conditions are easily distinguished via CT scanning.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree