9 Acute Respiratory Failure
Acute respiratory failure is one of the leading causes of admission to an intensive care unit (ICU). Behrendt et al. reported that the incidence of acute respiratory failure requiring hospitalization was 137 per 100,000 population in the United States, and the median age of the patients was 69 years.1 More recently, Ray et al. reported that 29% of patients presenting to an emergency department (ED) with acute respiratory failure require admission to an ICU.2
 Causes of Hypoxic Respiratory Failure
Causes of Hypoxic Respiratory Failure
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
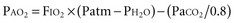
 ) mismatching. Hypoxia occurs as a result of
) mismatching. Hypoxia occurs as a result of  mismatching because of admixture of venous with arterial blood at the capillary level.
mismatching because of admixture of venous with arterial blood at the capillary level.  mismatching is the most common cause of hypoxia in hospitalized patients. In contrast to hypoxemia caused by an anatomic shunt, hypoxemia caused by
mismatching is the most common cause of hypoxia in hospitalized patients. In contrast to hypoxemia caused by an anatomic shunt, hypoxemia caused by  mismatching can be improved by administration of supplemental oxygen.
mismatching can be improved by administration of supplemental oxygen. mismatching is so severe that a portion of pulmonary arterial blood flows through lung regions with essentially no ventilation. Potential causes of this sort of physiologic shunting include pneumonia, lung contusion, or severe congestive heart failure. Oxygenation cannot be improved with supplemental oxygen in patients with a true right-to-left shunt, irrespective of whether the shunt is caused by an anatomic or a functional derangement.
mismatching is so severe that a portion of pulmonary arterial blood flows through lung regions with essentially no ventilation. Potential causes of this sort of physiologic shunting include pneumonia, lung contusion, or severe congestive heart failure. Oxygenation cannot be improved with supplemental oxygen in patients with a true right-to-left shunt, irrespective of whether the shunt is caused by an anatomic or a functional derangement.


