6 Low Systemic Arterial Blood Pressure
 Initial Evaluation
Initial Evaluation
A clinician’s initial evaluation should be a global assessment (Figure 6-1). When walking into a patient’s room, you should think, “What do I see?” and quickly determine whether the patient is in distress or has problems related to the airway or breathing. Look for obvious signs of external hemorrhage, look for evidence of hypoperfusion, and assess the adequacy of intravenous (IV) access. Do not rely solely on blood pressure (BP) readings, as there is no “normal” BP for all patients, and a BP value in the “normal” range does not always equate with adequate tissue perfusion. A patient with a history of poorly controlled chronic hypertension may have signs of hypoperfusion even when the BP is within the normal range (for nonhypertensive patients). Conversely, a patient with cirrhosis may have adequate perfusion despite having a lower-than-normal BP. A quick bedside assessment of tissue perfusion should include evaluation of mental status, urine output, and skin findings (e.g., temperature, diaphoresis, mottling, and capillary refill). If any of these parameters are abnormal, a more urgent approach to treatment must be taken.
 What Is the Cause?
What Is the Cause?
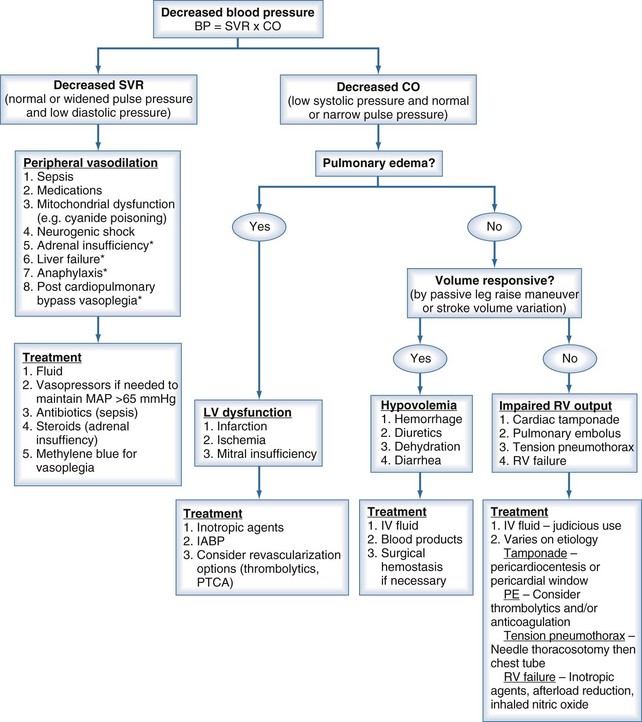
To help focus the differential diagnosis of a hypotensive patient, it is important to review basic cardiovascular physiology. The first concept to remember is that pressure = flow × resistance, where flow is cardiac output, and resistance is SVR. Because cardiac output is determined by stroke volume (SV) × heart rate, the presence of hypotension means that at least one of these parameters (e.g., SV, SVR, or heart rate) is abnormal.1 Disturbances in heart rate should be obvious by feeling the peripheral pulse, looking at the cardiac monitor, or evaluating a 12-lead electrocardiogram (ECG). The focus of this chapter is evaluating and treating conditions associated with decreased SV or SVR. By properly measuring pulse pressure and diastolic pressure, the clinician can determine whether the primary cause is a change in SVR or SV.
During systole, the SV is ejected into the proximal arterial conduits. Because more blood is being ejected than the peripheral circulation can accommodate in the arterioles, the arterial walls distend, increasing SBP in a way that is directly proportional to the SV and indirectly proportional to the capacitance (C) of the arterial wall. This relationship is represented by the formula1:
That is, for a fixed SV, if capacitance is higher, the SBP is lower.
During diastole, the portion of the SV that was “stored” by the distention of the arterial walls during systole fills the peripheral arterioles, leading to a progressive decrease in BP until the next systolic phase. This is the diastolic pressure, a parameter that is directly related to the SVR and capacitance (i.e., low diastolic pressure = low SVR and/or capacitance).1 When using these basic cardiovascular principles to understand the cause of hypotension, it is important to remember the following: (1) capacitance does not change from heartbeat to heartbeat, and (2) SV depends on preload, afterload, and contractility.
Low SVR is characteristic of a number of pathologic conditions, including sepsis, adrenal insufficiency, vasodilating medications, neurogenic shock, post–cardiopulmonary bypass (CPB) vasoplegia, and severe liver dysfunction. Decreased SVR should be suspected in the presence of a widened pulse pressure and low diastolic pressure.2,3
Reduced SV can be due to decreased preload, decreased contractility, or increased afterload. The most common cause of inadequate preload is hypovolemia. Other causes of inadequate preload include increased intrathoracic pressure due to dynamic hyperinflation in mechanically ventilated patients4,5 or tension pneumothorax, pulmonary embolism,6 mitral valve stenosis,7 cardiac tamponade,8 and right ventricular failure.9 Decreased contractility can be caused by myocardial ischemia or infarction, cardiomyopathy, myocarditis, negative inotropic drugs, myocardial stunning after CPB, and direct myocyte toxins, such as chemotherapeutic agents and inflammatory mediators (e.g., tumor necrosis factor [TNF] and interleukin 1-beta [IL-1β).10 A reduction in SV can be identified by decreased systolic BP and normal or narrow pulse pressure.