CHAPTER 67 UPPER EXTREMITY FRACTURES: ORTHOPEDIC MANAGEMENT
Fractures and dislocations of the upper extremity can vary from benign, requiring minimal intervention, to life and limb threatening. The treatment plan is based on the injury pattern including location, associated neurologic or vascular injury, status of the soft tissues, mechanism, and other associated injuries. In this chapter, several key issues in the decision-making process are discussed, followed by description and treatment of specific injuries.
OPEN FRACTURES
The associated soft tissue injuries add an element of urgency to the treatment of fractures. A fracture is classified as “open” if the fracture or fracture hematoma communicates with the air via a wound in the soft tissues. This can be caused from the bone protruding through the skin, “inside out,” or if there is a penetrating mechanism causing an injury from the “outside in.” Regardless, the implication is that environmental contamination can increase the incidence of infection and fracture healing complications. If there is a wound in the same limb segment as the fracture, it should be considered open until proven otherwise. A classification system for open fractures appears in Table 1. Infection rates are reported at 0%–2% for Type I, 2%–7% for Type II, and 10%–25% for Type III overall. Rates for type III are subclassified as follows: IIIA, 7%; IIIB, 10%–50%; and IIIC, 25%–50%.
Table 1 Classification of Open Fractures
DISLOCATIONS
Neurovascular compromise is the reason for emergent reduction of the joint. Sciatic nerve injury has been reported to occur in 8%–19% of hip dislocations. Osteonecrosis is a known complication of hip dislocations as well, occurring in up to 17% of these injuries. This is due to the interruption of capsular blood supply from the increased tension caused by the dislocation. Other associated neurologic injuries can be seen in Table 2.
Table 2 Neurologic Injuries Associated with Upper Extremity Fractures
| Joint | Common Neurologic Injury | Deficit |
|---|---|---|
| Shoulder | Axillary nerve | Sensory deficit in deltoid region, weakness of deltoid and teres minor |
| Elbow | Posterior interosseous nerve | Weakness of wrist dorsiflexion |
| Knee | Peroneal nerve | Weakness of ankle and great toe dorsiflexion |
| Hip | Sciatic nerve | More frequently common peroneal portion giving dorsiflexion weakness |
GUNSHOT WOUNDS
Special attention is deserved here due to the need to make an important distinction for the treatment of these injuries. It is important to determine if the wound was inflicted by a “low-” or “high-velocity” weapon. The exact distinction is somewhat cloudy, but according to the Wound Ballistics Manual of the Office of the Surgeon General, muzzle velocity greater than 2500 ft/sec constitutes “high velocity.” This is important because the kinetic energy of the bullet varies directly with the square of its velocity and only linearly with its mass.
IMAGING STUDIES
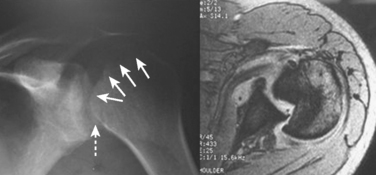
For fractures and dislocations, proper radiographic evaluation is essential before making any decisions regarding treatment of the injury. Ideally, two orthogonal views of the injured extremity should be obtained along with radiographs of the joints adjacent to the injured bone. Injuries to the shoulder girdle should have a minimum of three radiographic views in a standard trauma series, which includes anteroposterior (AP), scapular “Y,” and axillary views. Subtle injuries can be missed if adequate radiographs are not obtained. This is seen in Figure 1 of this missed posterior dislocation that was not properly diagnosed until a magnetic resonance image was obtained 6 months after the initial injury.
INJURIES TO SHOULDER GIRDLE AND HUMERUS
Scapula Fractures
A classification system was developed by Ada and Miller (Table 3), which divided fractures into those involving the acromion, spine and coracoid, type 1, glenoid neck, type 2, intra-articular glenoid fractures, type 3, and isolated scapular body fractures, type 4.
Table 3 Scapular Fracture Classification System
| Fracture Type | Anatomic Description/Location |
|---|---|
| 1A | Fracture through acromion |
| 1B | Fracture line through base of acromion or scapular spine |
| 1C | Fracture through coracoid process |
| 2A | Vertical glenoid neck fracture, lateral to base of acromion |
| 2B | Vertical glenoid neck fracture that extends up through scapular spine and supraspinatus fossa |
| 2C | Fracture line starts laterally at glenoid neck and propagates in transverse fashion through body exiting medially |
| 3 | Intra-articular glenoid fracture |
| 4 | Scapular body only |
Data from Ada JR, Miller ME: Scapular fractures: analysis of 113 cases. Clin Orthop 269:174–180, 1991.
Management of these fractures is often nonsurgical as poor healing is an infrequent complication due to the rich blood supply from the investing rotator cuff musculature. Nonoperative management consists of admission for a period of 24 hours to assess pulmonary and cardiac status. A brief period of sling immobilization is initiated for comfort, followed by passive range of motion. Most fractures are united by 6 weeks such that active mobilization and strengthening can ensue safely. Maximal functional recovery can take 6–12 months.
Proximal Humerus Fractures
Proximal humerus fractures are common injuries, especially with our aging population. The majority of these injuries are minimally displaced or nondisplaced and can be treated conservatively. Factors to take into consideration in the treatment plan are age of the patient, hand dominance, bone quality, fracture type, and fracture displacement. Associated injuries in the multitrauma patient are also important in the decision-making process.
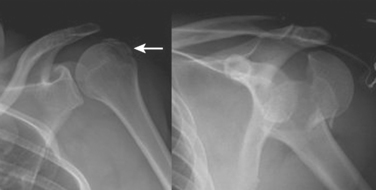
These fractures are classified according to the description by Neer. He described six variations of displaced proximal humerus fractures, and defined displacement as greater than 1 cm or 45 degrees of angulation. The anatomic “parts” consist of the anatomic neck, surgical neck, and greater and lesser tuberosities. Despite poor interobserver reliability, this is the most frequently used classification system. Figure 2 depicts various fracture patterns that are both considered “two-part fractures.” The portion of the humerus that is displaced has clinical relevance due to the varying blood supply of the proximal humerus. Displacement of the anatomic neck for example, has a high chance of disrupting the blood supply and adversely affecting outcome, regardless of the treatment chosen.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree