Chapter 24 Upper Airway Retraction
New and Old Laryngoscope Blades
II History
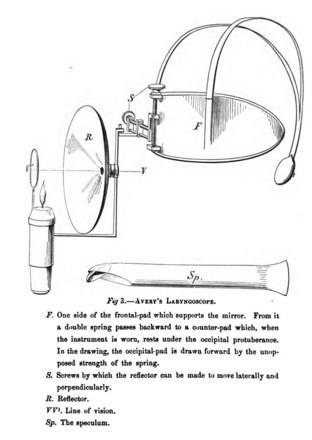
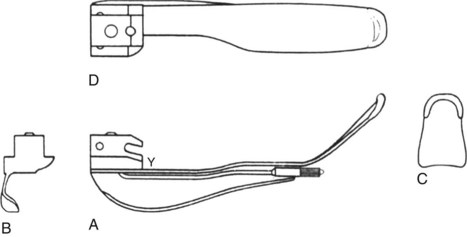
Benjamin Babington first described mirror-based indirect laryngoscopy in 1829,1 although it is often erroneously attributed to Manuel Garcia, a singer who described visualization of his own vocal cords in 1855.2–8 Babington also hinged a tongue depressor to his initial mirror design, but he subsequently abandoned the depressor and focused on the mirror alone (Fig. 24-1). In 1844, John Avery combined a reflective speculum with an external light source to view the larynx (Fig. 24-2).4 Mirror laryngoscopy for the investigation of laryngeal pathology was pioneered by Johann Czermak, who used instruments designed by Ludwig Turck in the late 1850s.5–8 Czermak subsequently applied an external light source and a head-mounted mirror to improve visualization.7

Figure 24-1 British physician Benjamin Babington combined a mirror and spatula.
(From Mackenzie M: Use of the laryngoscope in diseases of the throat, ed 2, Philadelphia, 1869, Lindsay & Blakiston.)
Horace Green, widely considered to be America’s first laryngologist, used tongue spatulas and probangs to examine and treat diseases of the larynx and trachea in the mid-1800s. In 1845, Green performed transoral removal of a laryngeal polyp in an 11-year-old girl using a bent tongue spatula to expose the larynx and polyp to direct vision (Fig. 24-3).7,9 Green’s technique9 is remarkably similar to the indirect elevation of the epiglottis described almost 90 years later by Macintosh:
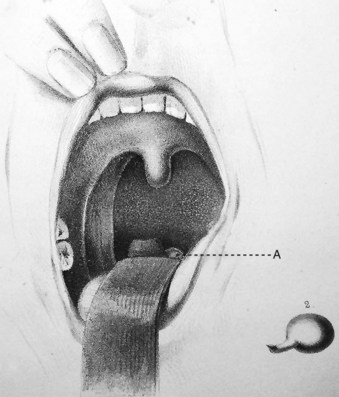
Green goes on to describe the use of a hook and knife passed “nearly an inch into the glottis” to extract the polyp. Despite Green’s accomplishments in direct laryngeal exposure, laryngeal surgery, and intubation, the first publication on direct laryngoscopy is credited to Alfred Kirstein in 1895, who called the new procedure autoscopy and devised techniques for use with the patient in sitting and supine positions.10,11 Kirtsein’s 1896 treatise on the procedure presages the development of laryngoscopy blades used in the modern era.11 He observes that the tongue must be drawn forward and downward (with the patient sitting in front of the operator): “To get this position of the tongue, a tongue depressor is necessary (i.e., spatula)—which, however, unlike the ordinary spatula, must not be placed in front of the circumvallate papillae but must be applied behind the same to the root of the tongue” (Fig. 24-4). The epiglottis can be elevated directly by an instrument that projects over the epiglottis (e.g., the tip of the spatula introduced behind the epiglottis) or indirectly by a method described by Reichert in 1879 and promulgated by Kirstein11:
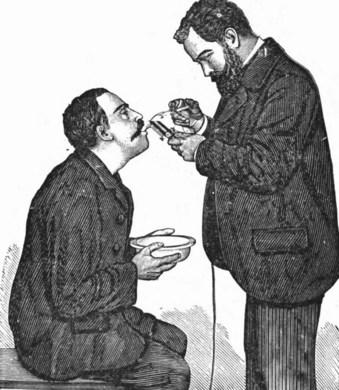
Figure 24-4 Alfred Kirstein performed autoscopy in the 1890s.
(From Kirstein A, Thorner M: Autoscopy of the larynx and the trachea (direct examination without mirror), Philadelphia, 1896, FA Davis.)
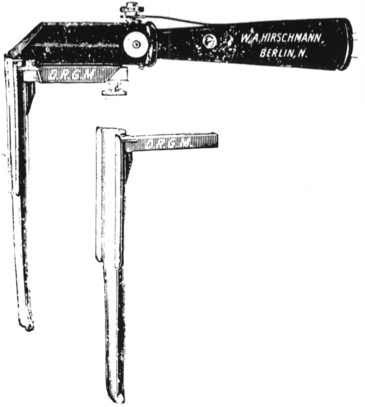
Kirstein developed two spatulas (Fig. 24-5). One had a distal, bent, bifid tip, which he called the standard spatula, that was designed for placement in the valleculae and pressed on the median glossoepiglottic ligament. Kirstein’s intralaryngeal, perfectly straight spatula was designed to be introduced behind the epiglottis and press it against the root of the tongue. His descriptions of these instruments and intended uses portray exactly the functioning of modern curved- and straight-blade laryngoscopes.11
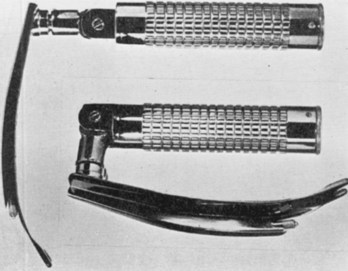
Chevalier Jackson, a professor of laryngology at Jefferson Medical College in Philadelphia (after Jacob de Silva Solis-Cohen, another Jefferson pioneer), refined laryngoscopy techniques in supine patients and established the principles of modern laryngoscopic exposure. Jackson created a tubed glottiscope in 1903 and was the first to apply enclosed distal lighting using a tungsten bulb that was connected to a large battery.5–912 Subsequent versions of Jackson’s tubular laryngoscope incorporated a removable, sliding floor that facilitated tube insertion, and he reported on the routine insertion of tracheal tubes using direct laryngoscopy in 1913 (Fig. 24-6).12,13 In the same year, Henry Janeway, an anesthesiologist at Bellevue Hospital in New York City, described a smaller and more portable laryngoscope powered by batteries located in the handle (Fig. 24-7).14 It featured a straight blade with a slight distal curve.14 Janeway’s blade did not achieve commercial success, but similar large, C-shaped, straight-blade designs created by Flagg, McGill, and Guedel became widely adopted.15,16
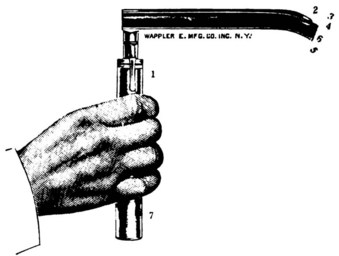
Figure 24-7 Henry Janeway produced a portable laryngoscope powered by batteries located in the handle.
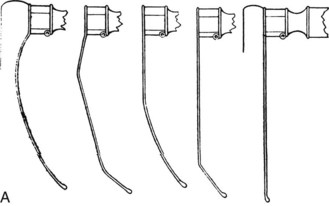
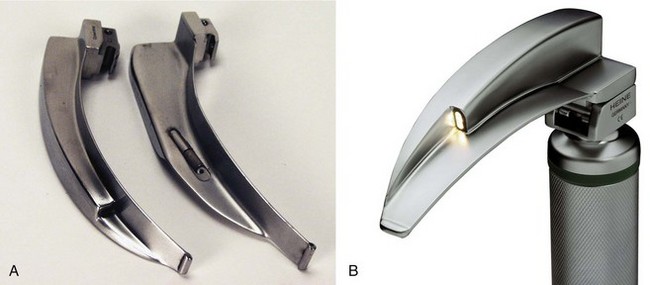
Laryngoscope blade design and laryngoscopy technique underwent little apparent evolution until Robert Miller’s 1941 narrow-lumen, D-shaped, straight-blade design and Robert Macintosh’s 1943 publication about a new curved-blade laryngoscope (Fig. 24-8, A).17,18 The Macintosh and Miller blades have become universally adopted and the benchmarks against which all direct laryngoscope blades are compared. Although innumerable modifications of these standard designs have been described in the past 70 years, only a few alternative designs have achieved widespread use. In the 1970s, the flexible fiberoptic bronchoscope offered another option for use in difficult situations, and rigid fiberoptic devices such as the Bullard laryngoscope were first introduced in the late 1980s. The 1990s saw the introduction of additional rigid fiberoptic laryngoscopes and commercially available fiberoptic stylets. In the 21st century, video-assisted devices have been added to clinical practice.
III Direct Laryngoscope Design
A Components of a Direct Laryngoscope
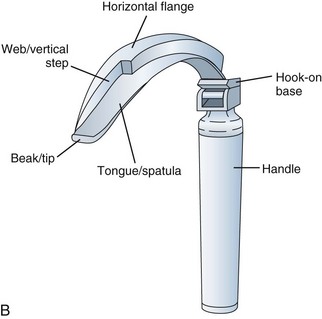
A laryngoscope consists of a handle, a blade, and a light source. There are marked variations in blade shape, tip design, and the mechanism and location of illumination systems (i.e., bulbs, or light-conducting fibers). The section of the blade that contacts the tongue is the spatula, and the left edge of the blade (from the operator’s perspective) is the flange. (see Fig. 24-8, B). The proximal vertical flange is sometimes called the vertical step. At the base (or heel) of the blade is the block, which interacts with the top of the handle. The connection between the blade and handle causes the light to come on when the blade is opened. Blades are designed to attach and detach from the handle with a standardized fitting (engaged at 45 degrees) that connects a hook on the blade to a small rod at the top of the handle.
B Direct Laryngoscope Lighting
Visualization of the laryngeal inlet during direct laryngoscopy depends on adequate illumination of airway structures by the laryngoscope. Illumination is a function of the intensity and color of the supplied light and the area over which it falls. These factors depend on the nature of the laryngoscope blade’s light source and the potential of the power source applied to it. Light can be measured in several ways: at its source (i.e., luminous flux, measured in lumens), at its receiving surface (i.e., illuminance, measured in lux), or by the amount of light re-emitted from a surface in a given direction (i.e., luminance, measured in candela per square meter [cd/m2]).19,20 During direct laryngoscopy, perception of the surface brightness of the larynx depends on light transmitted back to the laryngoscopist’s eyes from the surface of the larynx; this is luminance.
A significant variable in the perception of adequate lighting during laryngoscopy is the operator. As clinicians age, they develop presbyopia (beginning in the fourth decade, regardless of visual acuity), and the amount of light needed for a given visual task increases. This is especially significant in performing direct laryngoscopy because the larynx is sighted with only one eye due to the severe visual restrictions of the procedure.21 The procedure is visually analogous to looking down a 1-inch pipe at a target 12 to 18 inches away; visual restrictions include the mouth, teeth, tongue, blade, and epiglottis. Because the right and left eye are separated in the skull by 4 to 5 inches, the two views are disparate and cannot be merged into a stereoscopic view of the larynx. Subconsciously, we suppress the nondominant image through a phenomenon known as binocular suppression. It is not known what component of difficult laryngoscopy is related to inadequate lighting, but adequate illuminance is especially important when landmarks are obscured by secretions, blood, and vomitus and when the epiglottis causes shadowing of the larynx.
Historically, there was no standard for laryngoscope light, but the International Organization for Standardization recently agreed on a standard of 500 lux after 10 minutes of operation.22 The illuminance of a laryngoscope light at the distal tip of the blade is a function of the distance from the light source to the tip of the blade, the type of bulb or fiberoptic-conducting system, and the battery type and charge status.23 The light-to-tip distance is important because the amount of illuminance at a target is governed by the inverse square law (i.e., if the distance from the light source is doubled, one fourth of the amount of light lands on the target). Across different clinical settings, there may be dramatic differences in the illuminance of blade and handle pairs. Marked variation and poor light performance of laryngoscopes is widespread in anesthesia and emergency departments.23,24 In a study of many emergency departments in Philadelphia, there was a 500-fold difference in the illuminance produced by different blade and handle pairs, ranging from 11 to more than 6000 lux.24
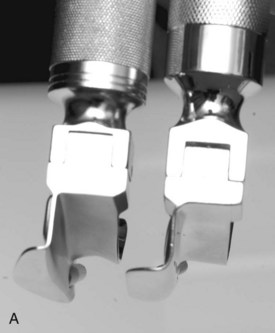
Bulb-on-blade laryngoscopes (called conventional blades) and fiber-lit laryngoscopes (in the United States, called green-line scopes) use different, non-interchangeable fittings (Fig. 24-9). Bulb-on-blade laryngoscopes have a simple electrical connection between the handle and blade. The electrical circuit is completed by opening the blade, providing power to the bulb, which is mounted on the distal aspect of the blade. Halogen and xenon bulbs are used by many manufacturers, but within the past 5 years, super-bright LED bulbs have become available. LED bulbs have tremendous advantages compared with other bulbs. They use a fraction of the energy of xenon or halogen bulbs, and they operate at much lower temperatures. The light they produce is much whiter, which may improve the discrimination of landmarks. The more yellow color of standard bulbs can be especially poor for distinguishing reddish yellow mucosal structures (e.g., epiglottis from the posterior pharyngeal wall). The primary reason LED lights will become standard on all instruments in the future is cost; as LEDs become much more commonly used on laryngoscopes and other portable medical instruments, the cost of the bulbs will continue to decrease. Some manufacturers already offer inexpensive, single-use, all-steel, LED-bulb blades (Fig. 24-10). Another advantage of LED bulb-on-blade designs is that they do not require expensive handle-battery systems because of their low energy requirements. This extends the operational and shelf life of the handle-battery pair dramatically, an important feature when stocking laryngoscopes in code carts and other settings.

Figure 24-10 Examples of all-steel laryngoscope blades with LED bulbs on them.
(Courtesy of SunMed, Largo, FL.)
An alternative illumination system uses light-conducting fibers in the blade with a bulb mounted in the top of the laryngoscope handle. In the United States, these blades have a green dot on the base, and the handles have a green ring on the top. Different types of fiber-lit blades and handles are not interchangeable. Fiber-lit systems depend on a good fit between the base of the blade and the top of the handle. A spring-loaded mechanism depresses the light at the top of the handle, making an electrical connection with the batteries. Problems with the spring may cause erratic performance, and a poor fit can allow light to escape between the bulb source in the handle and the fiberoptic bundle in the blade. The best light-conducting material is glass fiber, and the best designed of the glass fiber–lit blades use large arrays of fiber bundles (Fig. 24-11). There is significant variation in the size and quality of these glass fibers among manufacturers. Glass fiber is relatively expensive, and its light conduction deteriorates over time, depending on sterilization techniques.25 Fast deterioration in light conduction, erosion of the bond between the glass and blade, and rusting of the blade occurs with lower-quality glass fiber blades.
Acrylic can be used for light conduction, and although it is not as effective a light conductor as glass, it is inexpensive and easy to integrate onto a laryngoscope blade (Fig. 24-12). Glass fibers must be wrapped in a steel rod and then attached to the blade or threaded through a channel that runs the length of the blade, but an acrylic rod can be easily attached as a separate component. Better acrylic fiber–lit blades enclose part or all of the acrylic rod to minimize light loss (Fig. 24-13). Acrylic fiber–lit blades usually are designed as single-use blades; they are inexpensive to produce, and their light conduction deteriorates significantly with sterilization. The inferior light-conducting performance of acrylic can be compensated by super-bright bulbs (LED is best) and powerful handles, but these features necessitate relatively expensive lamps, reflectors, and battery systems (Fig. 24-14).

Figure 24-12 Disposable, fiber-lit blades are available in stainless steel with acrylic stems (SunMed Healthcare, Largo, FL).
A major variable in laryngoscope lighting involves the battery source. Standard handles use two C-sized batteries, and most pediatric handles or stubby handles use AA batteries. Several companies offer small handles that use a single, 3-volt, CR123 lithium battery (i.e., camera type). Compared with alkaline batteries, lithium batteries (regardless of size) have a flatter discharge curve, and they slowly diminish in power output over a long time. When lithium batteries start to fade, they die quickly; but during operation, they maintain a much more steady power output. Alkaline battery–powered handles continue to turn on even though light output has diminished dramatically. This phenomenon contributes to delayed battery replacement, because few clinical settings monitor blade and handle pairs using light meters. Many manufacturers offer rechargeable fiber-lit handles using nickel–metal hydride or nickel-cadmium batteries; combined with LED bulbs and special reflectors, these handles create brilliant white light that is far superior to older illumination technology (Fig. 24-15).
C Direct Laryngoscope Blade Design
Laryngoscope blade design has evolved through trial and error and by sophisticated technical analysis. Macintosh published a series of blade design drawings with which he had experimented; models varied from the curved blade so widely accepted subsequently to entirely straight blades18,26 (Fig. 24-16). Some investigators have made use of lateral head and neck fluoroscopy and radiography during laryngoscopy to help elucidate relationships of the tongue, hyoid bone, epiglottis, and laryngoscope blade during laryngoscopy.27,28
The scientific evaluation of laryngoscope blades has been impeded by the visual restrictions inherent to laryngoscopy; for example, the target is seen monocularly and therefore cannot be simultaneously viewed by two operators.21 Although a head-mounted direct laryngoscopy video system was invented in 1998 that allowed routine recording of the procedure from the operator’s perspective, few studies of laryngoscope blade design have used this objective tool.29 Most studies have relied on subjectively reported laryngeal view (i.e., visualization of the larynx by the laryngoscopist for a few seconds). The standard reporting system of laryngeal view (i.e., Cormack-Lehane classification) has poor interobserver reliability and is not very sensitive because up to 99% of direct laryngoscopies involve Cormack-Lehane grade 1 or 2 views.30 This grading system does not allow detection of differences between blade designs without a very large number of patients because of the relative scarcity of grade 3 and 4 views. The combination of restricted visualization, subjective reporting of the view, and lack of a sensitive means of reporting has historically retarded rigorous research on laryngoscopy blade design. As observed by McIntyre in a 1989 review article on blade design, “detailed evaluations of the performance of any particular laryngoscope blade are extremely rare and critical analysis virtually nonexistent.” 31
IV Direct Laryngoscopy Blades
A Macintosh and Related Curved Blades
1 Macintosh Laryngoscope Blade
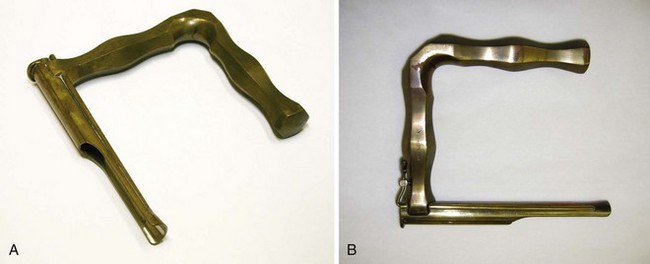
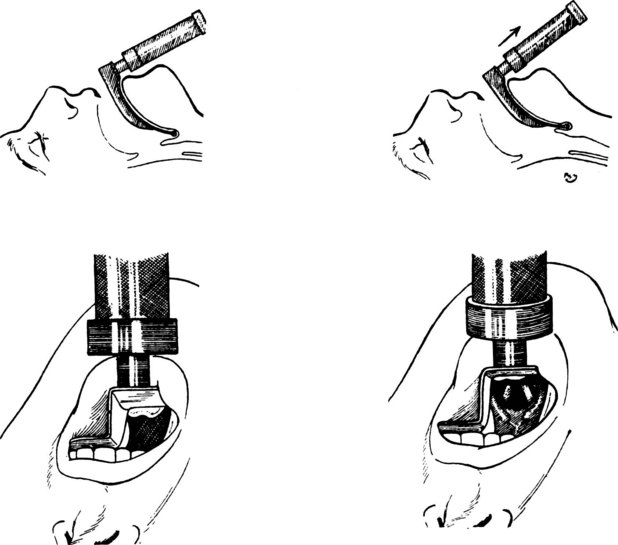
Macintosh’s 1943 publication of his curved-blade laryngoscope design defined a new blade and emphasized a novel technique of laryngeal exposure for anesthesiologists (i.e., indirect elevation of the epiglottis) (see Figs. 24-8A and 24-16).18 Although the pioneers of laryngology, including Green and Kirstein, were familiar with indirect elevation of the epiglottis, this technique was not widely appreciated in the new clinical discipline of anesthesiology. Macintosh stumbled into the design by accidentally exposing the larynx indirectly after inserting a Boyle-Davis mouth gag to keep the mouth open and depress the tongue during a tonsillectomy case: “Opening the mouth with the [Boyle-Davis] gag, I found the cords perfectly displayed.… Before the morning had finished, I had Richard Salt [senior technical assistant of his anesthesia department] … [solder] the Davis blade onto a laryngoscope handle, and this functioned quite adequately as a laryngoscope.”32 The Crowe-Davis gag had been in use for several decades (Fig. 24-17); Boyle popularized the use of this mouth gag in England during World War II.33

Figure 24-17 Davis blade.
(Courtesy of the University of Melbourne Museum Image Archives, Melbourne, Australia.)
Macintosh’s classic article in The Lancet described using his shorter, curved blade by placing its tip in the vallecula between the epiglottis and the base of the tongue, with subsequent indirect elevation of the epiglottis.18 Macintosh contended that he could use the blade at a lighter plane of anesthesia because of the predominant glossopharyngeal nerve innervation of the base of tongue area rather than the superior laryngeal nerve innervation of the dorsal surface of the epiglottis. This was important before the widespread use of neuromuscular blockers. He also mentioned the need to insert the blade to the right of the tongue, with a sweep to the left to displace and control the tongue.18 In this original communication, Macintosh stated and later reiterated that “the precise shape or curve of the blade does not seem to matter much provided that the tip does not go beyond the epiglottis.”18 However, numerous modifications of the Macintosh blade have been reported.
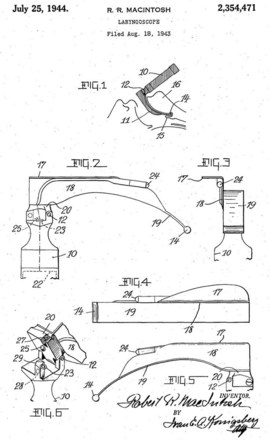
The specific design of the Macintosh blade has a circuitous history. Macintosh, a New Zealander, invented the blade while working in England. Richard Foregger, the son of Richard von Foregger, a manufacturer of early anesthesia devices, was stationed briefly in England during the Second World War. Macintosh gave his new blade to Foregger’s son to bring to America, and he also gave blades to two English manufacturers (Medical Industrial Equipment and Longworth Scientific Instruments).34 Macintosh did not pursue patents or royalties on his design. The U.S. patent application by the Foregger company shows Macintosh’s name spelled incorrectly (with a capital I in the middle), and this incorrect spelling persists on many labels34 (Fig. 24-18). The American and English Macintosh blade designs are descendants of the blades initially produced by the Foregger and Longworth companies, respectively.34 Macintosh thought that one size would fit all adults, but the blade was initially used in obstetrics cases (i.e., only in women). Eventually, a larger size was devised, which evolved into the modern Macintosh 4, whereas the original design approximates what became the Macintosh 3. Although manufacturers have produced a Macintosh 2 and Macintosh 1, these sizes were not endorsed by Macintosh, and direct laryngoscopy in small children and infants usually is done with straight blades.
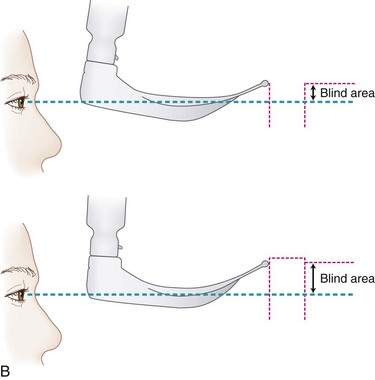
2 English Macintosh Blade
The English Macintosh laryngoscope, initially produced by Longworth in the United Kingdom, is continuously curved along the entire spatula, the flange runs to the tip of the blade, and the proximal flange is smaller34–36 (Fig. 24-19). In contrast, many versions of the American Macintosh are straight in the distal portion, have a distal tip without a flange, and have a very large proximal flange. The bulb on an English Macintosh is closer to the distal tip, increasing illuminance measured at the tip. Although not standardized across all English-labeled Macintosh blades, most English designs use a clear bulb, whereas American Macintosh designs usually come with a frosted bulb. English blades and American Macintosh blades are also offered with fiber-lit illumination systems, which typically use smaller (2- to 3-mm), round bundles.
Asai and colleagues conducted a randomized crossover study of the English blade, comparing it with the standard Macintosh in 300 patients.35 They found that the view with the English blade was better than the view with the standard blade in 34%, no different in 54%, and worse in 11% of patients. For the 42 patients with a Cormack-Lehane grade of 3 or worse with one blade, the view was rated better with the English blade than the standard blade in 60%, worse in 7%, and no different in 33% of patients.35 Yardeni and colleagues, in performing an in vitro technical analysis of various blades, concluded that the English Macintosh 4 provided the best results, surpassing those delivered by the American size 4 and English Macintosh 3 blades, even at shallow insertion depths.36 The flange heights on English Macintosh 4 and 3 blades are similar, but on the American Macintosh, the proximal flange on the 4 is much larger than the 3, and the larger size confers a significant risk of dental injury in some patients.
Levitan advocates the use of a narrow-flange-height Macintosh 4 German or English design on all adult emergency cases; if the full depth of the blade is not required, the flange height with these blades does not cause a problem (its height is the same as a Macintosh 3), but if more blade is needed, the depth can be increased without the need to switch the blade.37 As stressed originally by Chevalier Jackson, epiglottoscopy must always be performed to find the epiglottis before making any effort to expose the larynx; otherwise, a large blade can be inserted too deeply and fail to identify landmarks.38
3 German Macintosh Blade
Heine, the German medical instrument company, pioneered incorporation of a rectangular, large (4.3-mm), glass-fiber bundle combined with a small flange height and full-length flange similar to that of an English Macintosh (Fig. 24-20). Like the English Macintosh, it has a small light-to-tip distance. When paired with rechargeable batteries and especially with an LED bulb, this large fiber bundle provides an extremely intense, white light. This design is easy to clean because it has no irregular surfaces. Other manufacturers have copied this design, with some labeling it a German Macintosh.
4 Improved-Vision Macintosh Blade
In Macintosh’s original 1943 report of his curved-blade laryngoscope, the accompanying photograph of the blade showed a subtle flattening of the curve midblade. This disappeared early in the blade’s history, probably because of manufacturing considerations.32 In 1984, Gabor Racz described a modification in which the midportion of the Macintosh blade spatula was made concave (dorsally) in cross section, and the slight flattening of the midblade was reintroduced while the vertical step and flange were left intact (Fig. 24-21).39 The combined modifications should help to reduce the crest-of-hill effect whereby the midblade convexity can encroach on the direct line of sight from eye to laryngeal inlet. Racz reported that the blade had been used successfully in several cases in which conventional laryngoscopy had failed.39 The improved-view Macintosh is commercially available in multiple sizes from several manufacturers.
5 Bowen-Jackson Blade
Recognizing that curved and straight blades had advantages and disadvantages, Ronald Bowen and Ian Jackson attempted to create a blade that could be used in all difficult situations. The resulting blade is almost straight, but it has a fairly marked distal curve (Fig. 24-22). The distal beak of the blade is bifid to allow straddling of the glossoepiglottic fold. The maximum depth of the vertical step is substantially less than that of the Macintosh blade, and it occurs midblade and tapers proximally to allow its use in patients with limited mouth opening or prominent teeth. When attached to the handle, the blade forms an angle of 100 degrees to help avoid contact with the chest.40
6 Left-Handed Laryngoscope
A mirror-image version of the Macintosh blade exists for use with the right hand. Inappropriately referred to as the left-handed laryngoscope, it is identical to the regular Macintosh blade except for the reversed configuration of the flange. Potential uses include laryngoscopy of patients in the right lateral decubitus position, procedures in those with right-sided facial or oropharyngeal abnormalities, and procedures in which the endotracheal tube (ETT) should be located on the left side of the mouth.41,42
7 Curved Blades with Exaggerated Distal Curvature
Several blades have been described with a more acute curvature of the distal spatula than that of the Macintosh. Of historical interest, the Gubuya-Orkin blade, described in 1959, was unique in having an S-shaped blade with a malleable distal 3 cm. The investigators described bending it through a range of 15 to 45 degrees, with an optimal position thought to be 35 degrees from the horizontal for indirect lifting of the epiglottis (Fig. 24-23).43 Found to be effective in some cases in which Macintosh laryngoscopy had failed, the Gubuya-Orkin blade can be considered a forerunner of other blades with marked fixed or variable distal curvature.
Unlike the Macintosh blade, the Blechman blade has an accentuated curve at its distal tip. Its reverse-Z vertical step and flange begin distal to the block of the blade and extend only to within 5 cm of the blade tip. The curved Fink laryngoscope blade similarly has a sharper curve at the distal spatula and reduced vertical step proximally compared with the Macintosh. The ULX Macintosh (Upsher Laryngoscopy Systems, Mercury Medical, Clearwater, FL) blade has a more pronounced curve throughout the entire blade length than the standard Macintosh. The Wiemers or Freiburg blade, marketed in Europe, has less initial curvature than a Macintosh and has an acutely curved tip (Fig. 24-24).44 As a group, these blades may have utility in patients with limitations of mouth opening, impaired head and neck mobility, or prominent upper incisors, in whom the tip of a Macintosh blade may fail to engage the glossoepiglottic fold at the appropriate angle. More specific indications for these blades await scientific evaluation.
B Miller and Related Straight Blades
1 Miller Laryngoscope Blade
The use of straight blades, with entrapment and direct lifting of the epiglottis, was the common laryngoscopic technique when Miller introduced his modification of the straight laryngoscope blade in 1941. The blade he described was longer than the medium-sized blades available at the time, had a comparatively smaller flange height, was narrower at the tip, and featured a gradual curve starting 2 inches (5 cm) from the distal end (Fig. 24-25).17 Miller contended that the smaller flange height would allow less mouth opening (permitting freer anterior movement of the mandible) and less potential for damage to the teeth. Although Miller’s original design could accept a 38-F tube down the barrel, the flange height of modern Miller blades has become substantially smaller, and an adult-sized tracheal tube cannot fit down a Miller size 3 blade. Miller warned that the lumen should not be used for this purpose in his original description of the design.17 With a smaller degree of mouth opening, Miller conceded that available room for tube manipulation would be less and that a stylet would be desirable.17 In 1942, Cassels echoed Miller’s contention that a greater distal curvature of the straight blade would facilitate exposure of the laryngeal inlet, accompanying his report with an elegant diagram to help illustrate his theory.45 For a given position of the base of a straight blade between the teeth, especially when the mouth opening is limited, a curved distal tip can enable the laryngoscopist to visualize a more anterior aspect of the laryngeal inlet (Fig. 24-26). The Miller laryngoscope blade continues to be a commonly used straight blade.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree