CHAPTER 28 TRAUMA TO THE EYE AND ORBIT
Trauma and emergency physicians are frequently confronted with evaluating and managing severe eye injuries, most of which will require immediate consultation and referral to an ophthalmologist. We hope to describe the types of ocular emergencies that can be managed by the emergency and trauma physician, and clearly illustrate the techniques employed.
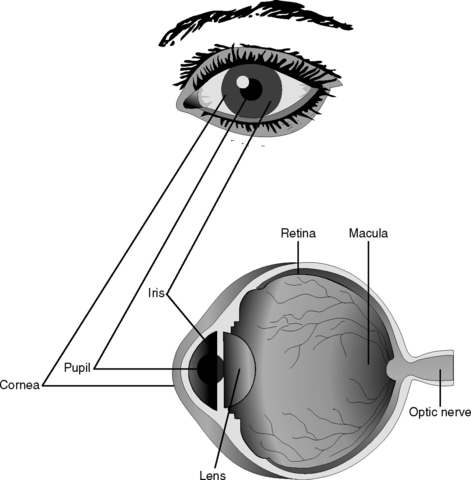
Direct injury to the eye requires the immediate involvement of eye care providers. Severely injured patients are often unable to cooperate with extensive ocular examination, and management decisions will be based on objective eye findings. In obvious open globe injuries, the emergency physician and the trauma surgeon can aid in obtaining a clear history of the injury and making the prompt decision for radiologic evaluation. Where an intraocular foreign body is suspected, or a thorough history cannot be elicited, an immediate orbital computed tomography (CT) should be obtained. A fox shield should be placed over the eye for protection and the remainder of the evaluation and management should be deferred to an ophthalmologist. In particular, the emergency medical physician should defer performing a slit-lamp examination and absolutely avoid measurement of intraocular pressure. The patient should also be asked to avoid maneuvers that may cause intraocular hemorrhage, such as coughing or Valsalva, and be urged to rest quietly until the wound has been repaired (Figure 1).1,2
When an open globe is not clearly obvious, a full ocular examination is carried out in a methodical and rational fashion, beginning with gross external inspection and visual acuity measurement in each eye, independently. Optic nerve function is assessed by testing for a relative afferent pupillary defect and, if appropriate, intraocular pressure is measured and a careful slit-lamp examination is performed. Dilated fundus exam can only be performed by trained personnel and can be left to the ophthalmologist. If the combination of clinical findings and ancillary testing is not clearly indicative of an open globe injury, but the suspicion remains high, then formal exploration under anesthesia is recommended. Photodocumentation is recommended whenever feasible.1 Prompt management by the initial emergency and trauma surgeons can have a profound impact on the ultimate visual function of these patients, and familiarity with the various types of urgent eye injuries will promote a system of ideal triage (Figure 2).
INCIDENCE
Ocular trauma in the United States occurs at an estimated rate of 2 million eye injuries per year (7 per 1000 population). Data gathered by McGwin et al.3,4 from national ambulatory care surveys and hospital discharge records reveal that most eye injuries in the United States are treated in emergency departments (50.7%), followed by private physicians’ offices (38.7%), and outpatient (8.1%) and inpatient (2.5%) facilities. Demographic analysis of the highest-risk groups reveals that eye injury rates are highest among males in their 20s, with no clear difference among ethnic groups.
The rate of eye injury begins to climb later in childhood, with peak incidence in the third decade, followed by a slow decline. A second peak occurs with very advanced age.4,5 This bimodal incidence in younger and older adults, as well as higher rates in males, is a reflection of the types of high-risk activities younger males engage in and the propensity for injuries and falls seen in older adults. These trends apply to injuries in these groups in general.
The setting in which an injury occurs has a marked impact on the severity and the prognosis for visual recovery. A study on the rate of eye injuries in the workplace reported that open globe injuries were the most common (46%), followed by injury to the surrounding ocular adnexal structures (20%), orbital fractures (11%), and traumatic hyphemas (11%).4,6 Interestingly, the vast majority (approximately 90%) of eye injuries occur in settings where protective eyewear can have a major impact (e.g., workplace, sports activities). In fact, in many of these settings, eyewear is mandated but is not being worn at the time of injury. Thus, it is estimated that up to 90% of eye injuries could be prevented if protective eyewear were worn in these settings.
Of the small number of motor vehicle–related eye injuries (estimated at 1.8% of all eye injuries in the United States), very few present as open globe injuries. The mandated use of seatbelts has resulted in a twofold decrease in the number of eye injuries. Curiously, this has been offset by a twofold increase in eye injuries in accidents where airbags have been deployed. The most frequent injury mechanism related to MVA is impact with the windshield, followed by the airbag, steering wheel, and flying glass.7 However, these statistics must be viewed in the context of the decreased number of fatalities with the advent of airbag and seatbelt use.
Overall, only a small percentage (2.3%) of eye injuries encountered in the emergency setting present as lacerations and punctures (Table 1 and Figure 3). The most common causes of eye injuries in this setting are foreign bodies (44.6%) and blunt trauma (33.0%) (Table 2 and Figure 4).4 In the subgroup of patients with blunt trauma, many of these represent ruptures of the sclera that may not be clearly obvious to the examiner. In these cases, the examiner must rely on the key clinical findings associated with occult scleral rupture, as outlined in the section on diagnosis. Werner et al.5 reported on these occult scleral ruptures and found that they can represent up to 25% of all potential ruptured globes that present to physicians. Of these suspected cases of occult rupture, roughly one-third were actually found to have eye ruptures at the time of surgical exploration.
Table 1 Post-Traumatic Eye Findings in Emergency Setting
| Type of Eye Injury | % |
|---|---|
| Contusion/abrasion | 44.6 |
| Foreign body | 30.8 |
| Conjunctivitis | 10.2 |
| Hemorrhage | 9.9 |
| Laceration | 1.8 |
| Puncture | 0.5 |
Adapted from McGwin G Jr., Owsley C: Incidence of emergency department-treated eye injury in the United States. Arch Ophthalmol 123:662–666, 2005.
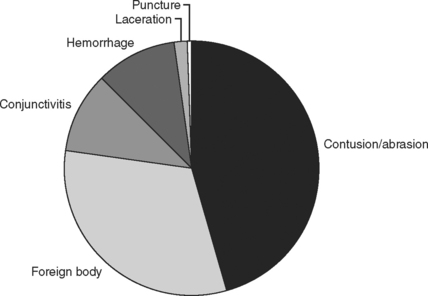
Figure 3 Post-traumatic eye findings in the emergency setting. See Table 1.
(Data from McGwin G Jr, Owsley C: Incidence of emergency department–treated eye injury in the United States. Arch Ophthalmol 123:662–666, 2005.)
Table 2 Key Mechanisms of Eye Injury in Emergency Setting
| Mechanism of Eye Injury | % |
|---|---|
| Foreign body | 44.6 |
| Blunt trauma | 33.0 |
| Fire/burn | 12.0 |
| Machinery | 3.1 |
| Motor vehicle accident | 2.3 |
| Fall | 1.8 |
| Firearm | < 1.0 |
Adapted from McGwin G Jr, Owsley C: Incidence of emergency department-treated eye injury in the United States. Arch Ophthalmol 123:662–666, 2005.
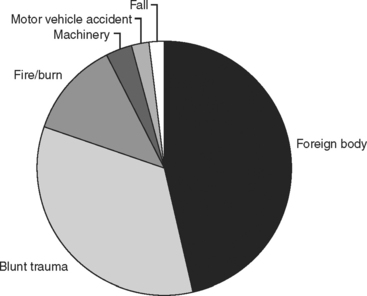
Figure 4 Key mechanisms of eye injury in the emergency setting. See Table 2.
(Data from McGwin G Jr, Owsley C: Incidence of emergency department–treated eye injury in the United States. Arch Ophthalmol 123:662–666, 2005.)
There is a significant association of orbital fractures found in patients presenting with head trauma. In a large study of 4426 U.S. Army soldiers with facial and orbital fractures, orbital floor fractures were found in 26%. Within this group, there was also a 30% incidence of injury to the globe and a 70% incidence of concomitant bodily injury.8 Fractures of the orbital floor and medial wall make up the majority of fractures, with the lateral wall being the third most likely site of fracture and a smaller number of fractures occurring in the orbital roof (Figure 5).9 The floor is most susceptible just medial to the infraorbital groove, whereas the medial wall is most likely to rupture at the lamina papyracea, a paper-thin bony septum.10
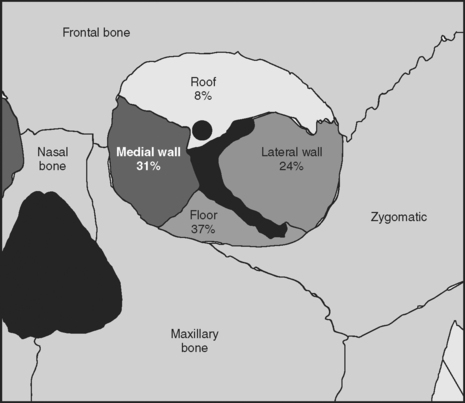
Figure 5 Diagram of orbital bones with incidence of orbital fractures.
(Original image obtained from Yanoff M, Duker JS: Ophthalmology, 2nd ed. St. Louis, Mosby, 2004, Figure 83-1. Data from Shere JL, Boole JR, Holtel MR, Amoroso PJ: An analysis of 3599 midfacial and 1141 orbital blowout fractures among 4426 United States Army Soldiers, 1980–2000. Otolaryngol Head Neck Surg 130:164–170, 2004.)
MECHANISM OF INJURY
The mechanisms of injury to the eye and surrounding structures are largely associated with foreign bodies, blunt trauma, and thermal and chemical burns. Machinery, motor vehicle, and firearms are among the less common causes (see Table 2 and Figure 4).4 There is often appreciable overlap, and the physician must consider the impact of these mechanisms in combination and treat each injury individually. For example, a ruptured globe from blunt trauma may require a short course of systemic steroids for traumatic optic neuropathy if an afferent papillary defect is noted. Blunt force on an eye can also be described as coup–contrecoup, or compressive force in a manner similar to brain injury. Examples of coup injuries are corneal abrasions, subconjunctival hemorrhages, choroidal hemorrhages, and retinal necrosis. The best example of a contrecoup injury is commotio retinae, with anterior forces being transmitted to the retina and causing shearing of the retinal layers.11 Compression of the globe usually causes scleral rupture. These open globe injuries are described below.
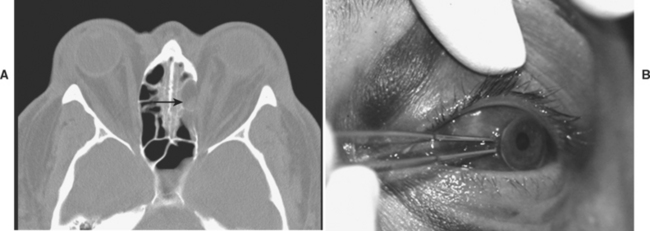
When the mechanism of injury involves penetration of the globe, the site of entry is usually visible and the decision for surgical intervention is straightforward. The three variables to consider when an entry wound is identified are whether the penetrating object has exited the eye, whether a foreign body is within the eye, or whether it has passed through the entire eye (perforation), in which case a posterior exit wound should be suspected and the foreign body may be located within the orbit.
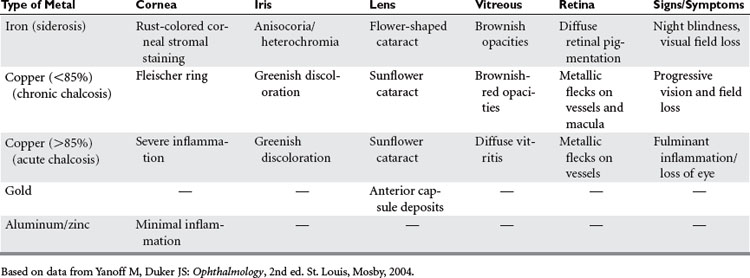
If there is evidence of an intraocular or intraorbital foreign body, the type of material may also have implications in toxicity to the eye and the risk of infection to the orbit and the eye (Table 3). When the history of the type of injury is unclear, an orbital CT should be requested immediately and a shield placed over the eye. Even if the foreign body is easily accessible and protruding from the eye or surrounding structures, the emergency or trauma surgeon should make no attempt to remove the object. A shield should be carefully placed over the eye and no manipulation attempted. The extent of injury can be assessed at the time of surgical repair.
DIAGNOSIS
Orbital Trauma
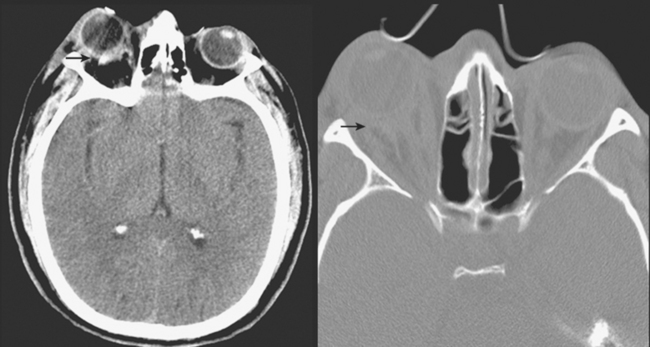
The key clinical features that aid in the decision for urgent management in cases of orbital trauma involve (1) significant limitation of ocular motility, (2) the presence of an afferent pupillary defect, (3) the presence of proptosis (abnormal anterior bulging of the eye), and (4) the presence of enophthalmos (abnormal posterior displacement of the eye). Any of these features requires an immediate orbital CT scan, ophthalmologic evaluation and consideration of surgical intervention. In a study by Lee et al.10 on the role of CT in orbital trauma, of those patients who suffered visual loss secondary to orbital trauma, the causes in order of decreasing frequency were retrobulbar hemorrhage, optic nerve thickening presumably secondary to edema, intraorbital emphysema, optic nerve impingement, retinal detachment, and ruptured globe. In addition to assessing the findings described previously the clinician should palpate the orbital rim for fractures (step-offs) and assess for hypoesthesia just below the eye in the distribution of the infraorbital nerve, and note the presence of hypoglobus (inferior displacement of the eye). Presence of hypoesthesia is indicative of a blowout fracture involving the infraorbital canal and nerve, but it has no urgent significance in itself.
Evaluation of ocular motility involves assessing for limitation of eye movement and eliciting symptoms consistent with decreased motility. The patient will often complain of double vision that disappears with the occlusion of one eye. Defining the orientation of the diplopia (horizontal, vertical, or oblique) can also help focus the exam. During the acute inflammatory period, ocular motility is often affected due to orbital congestion or muscle contusion, and supplementary tests can help distinguish between muscle palsy and muscle restriction or entrapment. Forced duction testing, where the eye is physically displaced using forceps to grasp the eye, can help discern the presence of mechanical restriction. A drop of anesthetic is placed on the eye and the patient is asked to look in the direction of the limited movement. The eye is then physically displaced in that direction to assess for a “tethering” effect (Figure 6). If significant resistance is encountered, entrapment must be suspected and an orbital CT should be obtained immediately. Clinical signs of entrapment supported by radiologic evidence require immediate surgical intervention to prevent muscle ischemia and necrosis.
The finding of post-traumatic proptosis requires immediate measurement of eye pressures to assess for retrobulbar hemorrhage. Proptosis and elevated intraocular pressures are indicative of an orbital compartment syndrome and an axial and coronal orbital CT should be obtained immediately (Figure 7). The findings on further examination are resistance to retropulsion, diffuse subconjunctival hemorrhage, tight eyelids and orbit, vision loss, an afferent pupillary defect, and decreased color vision. Medical therapy should be initiated immediately with pressure-lowering agents as described in the management section in this chapter, and intraocular pressure should be measured frequently to ensure the efficacy of the medical therapy. If the pressures are very high (>30) or if there is no response to medical therapy, a lateral canthotomy and cantholysis should be performed (described in the management section). This can be performed prior to obtaining an orbital CT if pressures are significantly elevated and there is evidence of an afferent pupillary defect.12
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree