CHAPTER 106 TRAUMA REHABILITATION
In 2002, unintentional injury was the most common cause of death between the ages of 1 and 44 years. There were 161,000 total injured deaths (56 per 100,000 population) that year. It was the fifth leading cause of death for all ages, after heart disease, malignant neoplasms, cerebrovascular events, and chronic respiratory disease. For males, it is the third leading cause of death, and seventh overall for females.1 Motor vehicle collision (MVC) was the most common cause of death related to trauma.
There were many more nonfatal than fatal injuries. In 2004, there were 29,654,475 (∼10,000/100,000) in the United States—involving all races, ages, and both sexes. Falls were most common (2756/100,000), followed by transportation-related injuries (1545/100,000). Violent nonfatal injuries occurred at a rate of 755/100,000.1
TRAUMA REHABILITATION TEAM
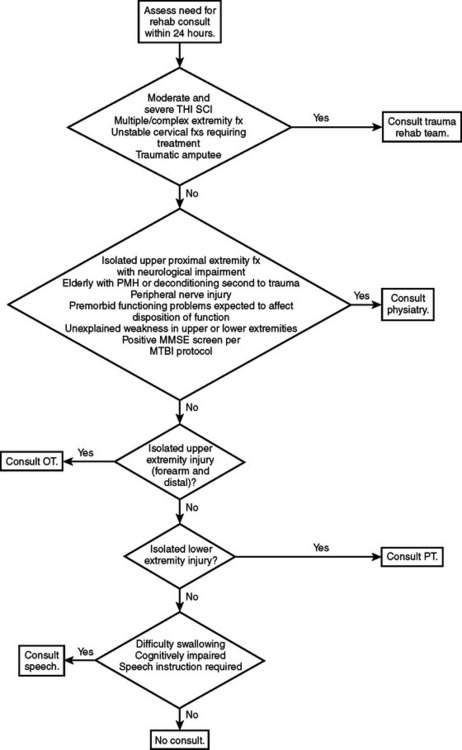
The case manager usually has a background in social service or nursing. Case managers play an integral role by assisting patients and their families with social and discharge planning issues. These managers are responsible for securing durable medical equipment, such as wheelchairs and modified commodes, for patients who are being discharged to home. See Figure 1 regarding rehabilitation screening of trauma patients.
ASSESSMENT OF PATIENTS WITH SPINAL CORD INJURY
Epidemiology of Traumatic Spinal Cord Injury in the United States
The incidence of SCI is estimated to be approximately 40 new cases per million population per year, or roughly 11,000. The estimated prevalence in the United States is 250 million persons.2 SCI primarily affects young adults. The average age at the time of injury is 37.6 years. The percentage of persons older than 60 years at injury has increased from 4.7% in 1980 to 10.9% since 2000. Of the SCI reported to the national database, 79% has occurred among males. Since 2000, MVC have accounted for 47.5% of SCI cases reported. Falls are the next most common cause of SCI, followed by acts of violence and recreational activities. Since 2000, the most frequent neurological category is incomplete tetraplegia (34.5%), followed by complete paraplegia (23.1%), complete tetraplegia (18.4%), and incomplete paraplegia (17.5%).3
Neurological Classification
Determining the neurological level and completeness of injury is the most accurate way of prognosticating recovery and functional outcome. Using the International Standards of Neurological and Functional Classification of Spinal Cord Injury, the examiner determines the motor and sensory level on the right and left and ascertains whether the injury is complete or incomplete.4
Using standard dermatomes and myotomes defined by the American Spinal Injury Association (ASIA), motor level is defined as the most caudal segment to have a muscle grade of 3. Five muscle groups are tested in the upper extremities, and five muscle groups are tested in the lower extremities. Each muscle group is supplied by two root levels, and each muscle group is graded from 0 to 5. Therefore, if the muscle grade is at least 3 of 5 the proximal root is believed to be intact. The sensory level is defined as the most caudal dermatome to have normal sensation to pin prick and light touch. Specific testing points are defined by ASIA4 (Figure 2).
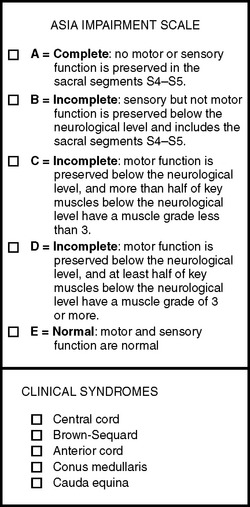
Figure 2 American Spinal Injury Association Impairment Scale.
(Adapted from American Spinal Injury Association: International Standards for Neurological Classification of Spinal Cord Injury, rev. 2006. Chicago, American Spinal Injury Association, 2006.)
In addition to defining the neurological level, the completeness of injury must be determined. See the ASIA impairment scale in Figure 2. A complete injury results in no motor or sensory function preserved in the sacral segments (ASIA A). There are four incomplete levels of ASIA: B, C, D, and E. Incomplete is defined as sparing of sensory and/or motor function below the neurological level that includes the sacral (S4-S5) segments.
Acute Medical Management
All patients with acute traumatic SCI receive methylprednisolone. This is based on the National Acute Spinal Cord Injury Studies (NASCIS), the last being NASCIS 3. This study concluded that patients treated within 3 hours of injury should receive 24 hours of steroids, and those treated in 3–8 hours of injury should receive 48 hours of steroids.5
C1-C3 neurological levels will require ventilatory support. The phrenic nerve (supplied by C3-C5 nerve roots) will be intact in patients with a C5 neurological level and below. As the level descends from mid-cervical to lower cervical, and then to thoracic, there will be greater innervation to abdominal and intercostal muscles—thereby making the work of breathing easier. The primary objective in early pulmonary management in SCI is to minimize secondary complications, including preventing hypoxemia, preventing and treating atelectasis, reducing risk of aspiration, and providing aggressive pulmonary management to compensate for impaired clearing of secretions.6
A bowel program should be established. Initially, a paralytic ileus is common. Patients may be placed on a stool softener and a daily or every-other-day suppository, with digital stimulation. This routine should be established about the same time each day. The goal is to prevent or minimize incontinence between bowel programs.
Deep venous thromboembolism (DVT) prevention is extremely important, as DVT and pulmonary embolism are major causes of morbidity and mortality in the SCI population. Sequential compression devices should be used, with or without elastic stockings, to improve lower extremity venous return. Such methods are contraindicated in patients with severe arterial insufficiency. Pharmacologic prophylaxis should be initiated within the first 72 hours, when not contraindicated. Low-molecular-weight heparin is the current recommendation. Anticoagulation should be continued for 8 weeks in patients with uncomplicated complete motor impairments, and for 12 weeks in complete motor injuries with other risk factors (lower limb fractures, history of thrombosis, cancer, heart failure, obesity, and age over 70). Vena cava filter placement is indicated in SCI patients with a contraindication for pharmacologic prophylaxis.7
ASSESSMENT OF PATIENTS WITH TRAUMATIC BRAIN INJURY
Epidemiology of Traumatic Brain Injury in the United States
There are 1.4 million people who sustain TBI in the United States annually. Approximately 50,000 will die, 235,000 are hospitalized, and 1.1 million are treated and released from the emergency department.8 Between 80,000 and 90,000 people experience long-term disability associated with TBI.9 According to the TBI Model System database, MVCs account for 48.3%—with the next most common cause of TBI being falls, followed by violence. The most common cause of death from MVCs is TBI. Approximately 5.3 million Americans (or about 2% of the population) currently live with disabilities caused by TBI.10
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree